Introduction
Acute pancreatitis is an inflammatory disease of the pancreas, which multiple etiologies can cause; the most common are alcohol consumption and gallstones1. Acute pancreatitis has variable severity and takes a mild course in most patients; however, it may cause local injury, systemic inflammation, multiple organ failure, and even death, which has been associated with severe acute pancreatitis. The most used severity classification of acute pancreatitis is the 2012 revision of the Atlanta Classification, which is divided into mild, moderately severe, or severe2. Consistently, more severe cases of acute pancreatitis are associated with a higher incidence of complications. Two phases of acute pancreatitis are known: early and late, which can overlap. The early phase comprises the first two weeks from the onset of the disease, while the late phase extends after two weeks from the onset and can last for months3.
It has been reported that 10-20% of cases of acute pancreatitis are associated with pancreatic necrosis, necrosis of peripancreatic tissue, or both4. Vascular complications are rarer, occurring in 1.2% to 14% of cases. Among these, the most reported complications have been the formation of pseudoaneurysms, hemorrhage from pancreatic pseudocysts, and venous thrombosis5. Arterial thrombosis is an infrequent complication with a high degree of mortality, for which there is limited information in the medical literature. The present study describes a case report of mesenteric and hepatic arterial thrombosis secondary to acute necrotizing pancreatitis and reviews the available literature.
Case report
A 59-year-old female patient, originally from Sasaima, Cundinamarca, Colombia, consulted for a clinical picture of high-intensity abdominal pain associated with emesis and abdominal distension.
She has a history of systemic arterial hypertension and grade II obesity and was under pharmacological management with losartan 50 mg per day.
During the abdominal pain study, the patient was assessed by the internal medicine service with a diagnosis of acute pancreatitis of probable biliary origin, and management with analgesia and intravenous fluids with crystalloids was indicated. The paraclinical parameters on admission were: total bilirubin of 3.05 mg/dL, direct bilirubin of 1.91 mg/dL, indirect bilirubin of 1.14 mg/dL, aspartate aminotransferase (AST) of 469 U/dL, alanine-aminotransferase (ALT) of 413 U/dL, complete blood count with absolute leukocyte count of 25,200, absolute neutrophil count of 22,700, hemoglobin of 18.9 g/dL, creatinine of 0.61 mg/dL, lipase of 224,200, and triglycerides of 185 mg/dL. An abdominal ultrasound was requested, showing cholelithiasis without acute cholecystitis, intra- and extrahepatic bile duct of standard caliber, and visualization of the head and part of the body of the pancreas with increased volume and echogenicity. She was evaluated by gastroenterology, ruling severe acute pancreatitis with a Marshall score of 2 points of probable biliary etiology. Medical management and surveillance were indicated.
The patient displayed a torpid evolution due to increased abdominal pain, tachycardia, respiratory deterioration due to dyspnea, a decrease in arterial oxygen pressure/inspired fraction of oxygen (PaO2/FIO2), an increase in total bilirubin levels to 8.17 mg/dL, with direct bilirubin of 5.59 mg/dL and indirect bilirubin of 2.58 mg/dL. Transfer to the intensive care unit (ICU) with control arterial blood gases with metabolic acidosis was indicated, and it was decided to request a contrast-enhanced computed tomography (CAT) scan of the abdomen. Subsequently, the patient had a hypoxemic ventilatory failure, requiring management with orotracheal intubation and invasive mechanical ventilation. She was re-evaluated by gastroenterology, who considered a possible Tokyo III cholangitis, so they requested an endoscopic retrograde cholangiopancreatography (ERCP). However, before performing the procedure, the CT result showed acute edematous interstitial pancreatitis with signs of pancreatic necrosis in the head and tail with an extension of 80% (Figure 1), no opacification of the lumen of the superior mesenteric artery at 60 mm from its origin and no opacification of the lumen of the hepatic artery compatible with arterial thrombosis.
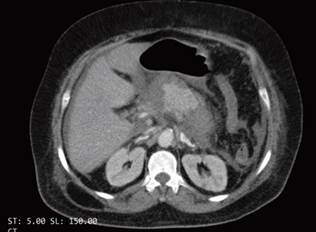
Source: Authors’ archive.
Figure 1 Computed tomography (CT) reveals acute necrotizing pancreatitis, primarily of the head and body of the pancreas.
The patient was immediately taken for an abdominal aortography, selective arteriography of the abdominal vessels, and thromboembolectomy by interventional radiology, finding occlusion of the common hepatic, superior mesenteric, and inferior mesenteric arteries (Figure 2). Using 6 Fr and 8 Fr indigo catheters, aspiration thrombectomy was performed on multiple occasions, and acute and subacute clots were obtained, with which it was only possible to revascularize the proximal third of this artery with outflow through the pancreatoduodenal arch that reperfused the hepatic artery proper and the first jejunal branch (Figure 3). The distal two-thirds of the superior mesenteric artery could not be revascularized due to poor outflow. Immediately after the procedure, the patient was taken to ERCP. In the second duodenal portion, marked edema that did not allow visualization of the papilla was observed, so the procedure was suspended.
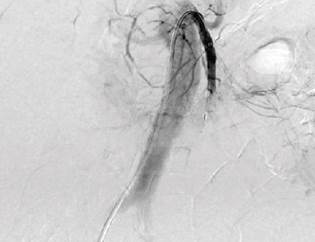
Source: Authors’ archive.
Figure 2 Selective arteriography of abdominal vessels denoting occlusion of the common hepatic, superior mesenteric, and inferior mesenteric arteries.
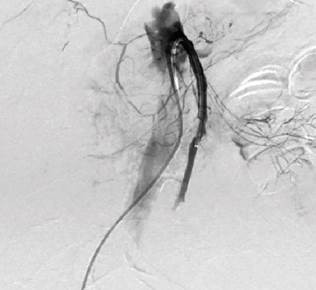
Source: Authors’ archive.
Figure 3 Reperfusion of the hepatic artery proper and first jejunal branch.
The patient presented with clinical and paraclinical deterioration; multi-organ failure was considered due to cardiovascular, pulmonary, and renal involvement, and she subsequently died.
Discussion
Acute pancreatitis is one of the most common gastroenterological pathologies for which patients consult the emergency room. It involves significant morbidity and mortality and an economic burden on the health system since it represents high costs, particularly when associated with severe complications3. In Colombia, it has been reported that the most common cause of acute pancreatitis is of biliary origin; besides, most cases are classified as mild6. Mortality in Colombia has been reported around 2.5% and 4.1% in the general population7,8. However, in cases of severe acute pancreatitis, mortality rates of up to 8.25% have been reported6.
Vascular complications of acute pancreatitis are rare but are highly feared due to their high mortality rate9. The most frequent vascular complications are venous thromboses, which are more associated with alcoholic etiologies. Among these, the most frequently involved veins are the splenic vein, the portal vein, and the superior mesenteric vein9, and they are rarely associated with bleeding from necrotic tissue. Among the arterial complications, the most frequent is the formation of pseudoaneurysms, which have been reported in up to 10% of patients with acute necrotizing pancreatitis5. It may involve any pancreatic or peripancreatic artery, and involvement of the splenic artery, gastroduodenal artery, and left gastric artery is most common. Arterial pseudoaneurysm is the cause of 60% of massive hemorrhages related to acute necrotizing pancreatitis, with high mortality rates.
Arterial thromboses are the rarest vascular complication of pancreatitis; a prospective study that sought to evaluate arterial complications in 189 patients with acute pancreatitis did not find arterial thrombosis10, and reports of these complications have been limited to case series. During the review of the literature, case reports of thrombosis of the superior mesenteric artery11,12, renal arteries13, aortic thrombosis14, and the celiac trunk15 were found. No reports of hepatic artery were identified. Moreover, no other apparent causes of mesenteric arterial thrombosis were detected in our patient.
In recent decades, the pathophysiology of arterial complications has moved away from the proposal of enzymatic autodigestion. It is currently considered that there is a cascade of microvascular events related to systemic and local inflammation that results in episodes of ischemia and reperfusion; these episodes produce acinar damage, release of pancreatin, recruitment of lymphocytes, and subsequent release of proinflammatory cytokines, which translates into proteolytic leak that, together with reactive oxygen species and cytokines, generate microvascular damage in the endothelium. This has been proposed as the pathophysiological mechanism of the vasa vasorum that would lead to thrombus formation9. The above has been related to the systemic inflammatory response and multi-organ failure1.
The clinical manifestation of arterial thrombosis secondary to acute necrotizing pancreatitis is not well established due to the lack of high-quality information; however, its manifestation is associated with severe abdominal pain that does not modulate with analgesia or match the clinical status of patients. The diagnosis can be made through contrast-enhanced CT, contrast-enhanced magnetic resonance imaging of the abdomen, Doppler ultrasound, or angiography5. The treatment is poorly established; still, in previous case reports, mechanical thrombectomy, pharmacological thrombectomy, and pharmacomechanical thrombectomy (a combination of both techniques) have been described as alternatives, especially in the context of the absence of intestinal ischemia, suggesting that management should be surgical11. The procedure should be strictly monitored, and surgical management should be considered in case of clinical deterioration. Adequate water management has also been described as paramount; in recent studies, it has been suggested that aggressive early management with intravenous fluids results in a higher incidence of fluid overload without improvement in clinical outcomes16.
The mortality of arterial thrombosis is extremely high; in different series of cases, it has been reported to be greater than 90%10,11. The majority of cases were reported in women and patients with a history of obesity, high blood pressure, or diabetes, which constitute a metabolic syndrome. Nonetheless, information is too limited to establish apparent risk factors.
In conclusion, this article presents a case report of thrombosis of the superior mesenteric artery and hepatic artery secondary to acute necrotizing pancreatitis of biliary origin, a rare entity with high mortality rates. Early identification of this pathology is essential to determine early endovascular or surgical treatment. High-quality studies identifying risk factors, clinical manifestation, and better management strategies for this pathology are needed. For now, it requires timely multidisciplinary management due to the high complexity and unfavorable outcomes.











 text in
text in 



