Introduction
Benign esophageal strictures resulting from the aftermath of radiotherapy, surgical interventions, caustic ingestion, or endoscopic mucosal resection are predominantly treated through endoscopic dilation procedures1. Despite this, between 30% and 40% of patients experience recurrence even after undergoing thorough dilation processes1,2. Refractory esophageal stricture (RBES) is characterized as a condition in which it is impossible to maintain luminal patency following five dilation attempts1,3. Managing RBES poses a significant therapeutic challenge. Available treatment strategies include repeated endoscopic dilations, injections of corticosteroids or mitomycin C, incisional therapy, or the placement of a temporary stent; however, these treatments have a limited efficacy over the long term and significantly burden both the patient and the healthcare system3. One study highlighted that the period free from dysphagia in patients with RBES treated with endoscopic dilations lasted for three months, and 2.4 months for those who underwent esophageal stent placement4.
Clinical case
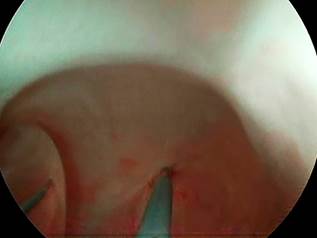
A 32-year-old patient experienced an accidental ingestion of caustic substances, leading to chemical pneumonitis and a complete obstruction of the esophagus. Following a two-week admission to the intensive care unit (ICU), the patient recovered from the acute episode and was discharged with an endoscopic gastrostomy. One month later, the patient was referred for dilation treatments. During the initial dilation endoscopy, a complete obstruction of the esophageal lumen was observed. Attempts to recanalize the esophagus through both digestive endoscopy and retrograde endoscopy via the gastrostomy were unsuccessful (Figure 1). Consequently, the patient underwent esophagectomy with esophago-pharyngeal anastomosis and the creation of a neoesophagus. Due to the high location of the stricture, the neoesophagus was anastomosed parallel to the oropharynx. Subsequently, the anastomosis developed a post-surgical stricture, necessitating radial incisions of the anastomosis (Figure 2).
The patient revisited one month later presenting with strictures, prompting the initiation of a dilation regimen using Savary dilators (Figure 3). Regrettably, the patient experienced recurrent strictures every 10 to 15 days. Attempts at management with corticosteroid injections in all four quadrants proved unsuccessful, as did the application of mitomycin C instilled at the site of the stricture. Consequently, the decision was made to transition to a self-dilation protocol as the final option, given the patient’s requirement for sedation every 8 to 10 days for dilation via endoscopy. Initially, the patient underwent training under endoscopic supervision (Figure 4), and upon becoming proficient, commenced interdiary self-dilations using a Savary dilator number 14 (Figure 5), achieving successful outcomes that have persisted to the present, completing approximately three years.
Discussion
The practice of esophageal self-dilation, wherein the patient learns to routinely introduce a dilator (e.g., Maloney dilator) through the mouth, has been documented since the 1970s3. Several studies, predominantly retrospective in nature, have underscored the efficacy of this therapeutic approach in the management of RBES, demonstrating a decrease in the necessity for endoscopic dilations from an average of 21.7 annually to merely one5. A specific study involving 52 RBES patients at Clínica Mayo recorded a significant reduction in the frequency of endoscopic dilations from 9.5 (range 5-30) per year to 0 (range 0-3) annually, pre and post initiation of esophageal self-dilations, respectively (p < 0.0001). This intervention not only improved dysphagia symptoms but also increased the likelihood of discontinuing enteral nutrition tubes3.
Our report showcases a successful instance of self-dilations in managing RBES. Illustrated in Figures 1-5 and a step-by-step video on YouTube (https://youtu.be/94KkDmKgMsQ), all techniques utilized for addressing the complex stenosis, culminating in the self-dilations, are meticulously delineated. Specifically, a Savary dilator size 14 was employed. The intention is for these procedures to be disseminated within the medical community, thereby benefiting similarly selected patients.
Conclusion
Despite long-standing recognition in medical literature, research on self-dilation remains limited, primarily encompassing small, retrospective studies5. It can be concluded that self-dilation presents a viable therapeutic option for patients with RBES, characterized by high effectiveness and minimal adverse effects. Successful outcomes are contingent upon careful patient selection for this therapy.











 text in
text in