Introduction
According to the World Health Organization, head and neck cancers (HNCs) occur in areas such as the pharynx, larynx, trachea, oral cavity, cervical lymph nodes, salivary glands, paranasal sinuses, skull base, ear, and paragangliomas in the same region. In the oral cavity, the most common primary sites include the tongue, palate, gums, lips, floor of the mouth, and base of the tongue 1.
In Brazil, the National Cancer Institute estimates there will be approximately 704,000 new cases of cancer by 2025, due to the population's increased life expectancy. This scenario makes cancer one of the greatest public health challenges globally 2. Also in Brazil, HNCs have a high prevalence with significant incidence and mortality rates with a considerable impact on patients' quality of life 3.
Treatment for HNCs can entail a range of different therapeutic modalities, such as surgery, radiotherapy, and chemotherapy, with surgery being the most recommended for initial lesions, while chemotherapy and radiotherapy are modalities that provide patients with a greater chance of survival 4. However, despite the advancements in treatment, HNCs can still have an unfavorable prognosis, with a five-year survival rate ranging from 28 % to 67 %, and with a treatment that can cause dysphagia, dysphonia, functional loss, facial disfigurement, and interference in social relationships 3.
This becomes a problem, since in oncology, which is considered a highly complex area 5, patients often find it difficult to access healthcare services 6, in contrast to the precepts of Law 12.732, which establishes the right to treatment free of charge by the Unified Health System (SUS, for its initials in Portuguese) within 60 days of diagnosis 7.
In addition, this reality is common in people with HNCs, since factors such as socioeconomic vulnerability, low level of education, male gender, senility, smoking, and alcoholism are recurrent in these patients. As a result, they often face challenges in accessing diagnosis and treatment; eventually, they access tertiary health services with cancer at an advanced stage, which makes therapeutic management difficult 8. Therefore, treatment is compromised by the late access, and the therapy adopted will have to be aggressive, with worse prognostic and survival outcomes. For this reason, it is necessary to know the profile of patients with HNCs to devise a care plan that encompasses prevention and health promotion strategies in a timely and effective manner 3.
Given this scenario, it can be noted that surgery for HNCs represents the third leading cause of care for patients with this condition, requiring a high volume of appointments and specialized care. Furthermore, in terms of frequency, the population and epidemiological profile of HNCs involving the larynx and oral cavity ranks sixth and seventh, respectively, when compared to other types of cancer, which justifies specific navigation for this population 9.
In light of this, in 2015, nursing in Brazil launched efforts to implement advanced practice nursing (APN), intending to expand access to healthcare services, placing nurses at the core of this process 10. In 2016, the National Supplementary Health Agency implemented the OncoRede project to reorganize the cancer care network by developing patient navigation programs 11. In 2023, Law 14.758 established the National Navigation Program for People with a Cancer Diagnosis to facilitate access to the SUS, as well as to overcome institutional vulnerabilities and socioeconomic and personal barriers 12.
To further strengthen the role of nurses, in 2024, the Federal Nursing Council instituted Resolution 735, which regulates the role of nurses as navigators, who must perform advanced practices with autonomy and care management, promote health education and help patients, families, and support networks to overcome the biopsychosocial barriers of services with timely care 13.
Patient navigation by nurses requires clinical experience, communication skills, and a high level of knowledge of healthcare systems. Furthermore, in oncology, the APN must be conducted to correctly identify and address the range of biopsychosocial and physical problems throughout diagnosis and treatment 14.
Therefore, nursing care for patients with HNCs must encompass a critical and reflective process 15, and patient navigation measures by oncology nurses corroborate therapeutic quality through systematized care, from diagnosis to the end of treatment, continuously, with the development of a longitudinal care plan, coordination, communication, and considering socioeconomic, sociocultural, psychological, and bureaucratic obstacles, which can lead to improved standards of care 16,17.
In this context, the aim is to research scientific evidence available on nurse navigation for patients with head and neck neoplasms.
Materials and Methods
This is an integrative review consisting of six stages 18. To select the guiding question: What is the evidence available on nurse navigation for patients with head and neck neoplasms? (stage 1), the PICo acronym was used 19, where 'P' stands for 'patient' (head and neck neoplasms); 'I' for the phenomenon of interest (patient navigation); and 'Co' for the context (nursing).
The literature search (stage 2) was conducted from July to August 2023, by the first author, through the Journal Website of the Coordination for the Improvement of Higher Education Personnel (Capes), Brazil, which facilitated access to databases and electronic portals. The databases searched were the following: Nursing Database (BDEnf), Latin American and Caribbean Health Sciences Literature (Lilacs), Medical Literature Analysis and Retrieval System Online (Medline) via PubMed Central® (PMC), Scopus Info Site (Scopus), Web of Science (WoS), Embase and, finally, the Scientific Electronic Library Online (SciELO) repository of scientific papers.
Search strategies were used based on health science descriptors (DeCS) in Portuguese and Spanish: "neoplasias de cabeça e pescoço", "neoplasias de cabeza y cuello", "câncer de cabeça e pescoço", "navegación de pacientes", and "enfermería" along with the Medical Subject Headings (MeSH) in English: "head and neck neoplasms," "patient navigation," and "nursing." Regarding the possibility of searching and reproduction, the strategies used in this review were stored in the Figshare repository 20.
The DeCS and MeSH were combined to model the search strategies, using the Boolean operators AND and OR to retrieve more primary articles, as shown in Table 1.
Table 1 Databases, Electronic Websites, and Search Strategies. Belém, Pará, Brazil, 2024
| Databases and electronic websites | Strategy used |
|---|---|
| Medline BDEnf Lilacs | (“neoplasias de cabeça e pescoço” OR “head and neck neoplasms” OR “neoplasias de cabeza y cuello” OR “câncer de cabeça e pescoço”) AND (“patient navigation” OR “navegación de pacientes”) AND (“nursing OR enfermeira”) |
| Scopus | ((“neoplasias de cabeça e pescoço” OR “head and neck neoplasms” OR “Neoplasias de cabeza y cuello” OR “Câncer de cabeça e pescoço”) AND (“patient navigation” OR “navegación de pacientes”) AND (“nursing” OR “enfermería” ) |
| WoS | ((ALL=("neoplasias de cabeça e pescoço" OR "head and neck neoplasms" OR "neoplasias de cabeza y cuello" OR "cáncer de cabeça e pescoço")) AND ALL=("patient navigation" OR "navegación de pacientes")) AND ALL=("nursing" OR "enfermería") |
| Embase | ('neoplasias de cabeça e pescoço' OR 'head and neck neoplasms'/exp OR 'head and neck neoplasms' OR 'neoplasias de cabeza y cuello' OR 'cáncer de cabeça e pescoço') AND ('patient navigation'/exp OR 'patient navigation' OR 'navegación de pacientes') AND ('nursing'/exp OR 'nursing' OR 'enfermería') AND [embase]/lim |
| SciELO | (*"neoplasias de cabeça e pescoço" OR "head and neck neoplasms" OR "neoplasias de cabeza y cuello" OR "cáncer de cabeça e pescoço") AND ("patient navigation" OR "navegación de pacientes") AND ("nursing" OR "enfermería") |
Source: Prepared by the authors.
The following inclusion criteria were set: primary studies in Portuguese, English, and Spanish, with no time frame. Duplicate studies, reflection articles, letters to the editor, experience reports, case reports, formative opinions, research protocols, commentaries, and short communications were excluded.
The study selection stage was conducted from September to October 2023 and was performed by two researchers, one of whom holds a master's degree and the other a doctorate, who were responsible for the two-stage selection, with blinding, to ensure a double-blind review. This stage was conducted using the Rayyan review management software 21. It should be noted that in cases where there was disagreement between the reasons for exclusion and inclusion, a third researcher with a doctorate was contacted to define the selection. At the end of the first selection-title and abstract reading-the full text was then read.
A total of 264 records were identified and, after applying the inclusion filters, reading the titles and abstracts, and reading the full text, 13 articles were included as the corpus for the synthesis, as shown in Figure 1, using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses - Prisma 22 checking flowchart.
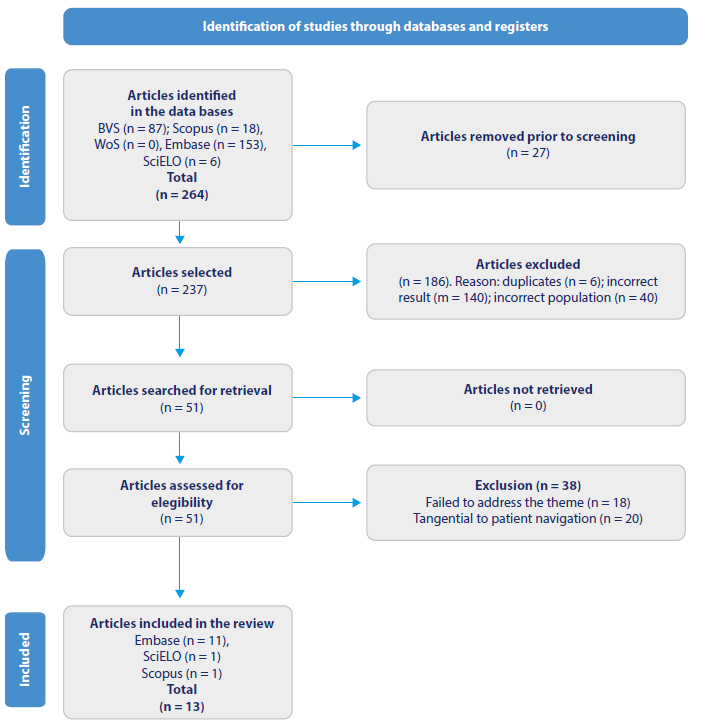
Source: Adapted from Prisma 22.
Figure 1 Flowchart for study selection in the integrative review, Belém, Pará, Brazil, 2024
The evidence extracted (step 3) considered the elements of an instrument from the Joanna Briggs Institute, used to extract data in integrative reviews 23 to obtain the summary table: Author, country, publication year, title, database, and level of evidence.
After applying the inclusion filters, the articles selected for this review were further assessed using the Escala de Evaluación de Artículos con Metodologías Heterogéneas para Revisiones Integrativas -(EAMH) Scale for Evaluating Articles with Heterogeneous Methodologies for Integrative Reviews-24. It contains the following six questions regarding the article: i. Does it have a clear definition of the objectives?; ii. Does it have a clear definition of the type of methodology used?; iii. Are objectives consistent with the methodology?; iv. What is the justification for the quantity and type of sample?; v. Does it have a description of access to the sample?; and vi. Do the results or conclusions address the objectives? The EAMH provides the following scores: 0-3 points: exclude article from analysis; 4-5 points: article suitable for analysis; 6 points: ideal article 23. Thus, the final sample of this review consisted of 11 articles. The metadata relating to the scores of each article was recorded and is available on the Figshare platform 25.
Seven levels of evidence were used to assess the scientific evidence (step 4), as follows: Level I: systematic review or meta-analysis of randomized controlled clinical trials; Level II: well-designed randomized controlled clinical trial; Level III: well-designed clinical trial studies without randomization; Level IV: well-designed cohort and case-control studies (non-experimental); Level V: systematic review studies of descriptive and qualitative studies; Level VI: evidence from a single descriptive or qualitative study; and Level VII: evidence stemming from the opinion of authorities in editorials and/ or specialist committee reports 26.
In the stage of interpretation and synthesis of the findings (stages 5 and 6), the evidence was grouped by level of theme similarity, in a descriptive-narrative way, into thematic axes that used the integrated convergent approach of the Joanna Briggs Institute 23.
Results
The results presented in Table 2 show that, in terms of databases and electronic websites, 11 (84.6 %) articles were retrieved from Embase, 1 (7.7 %) from SciELO, and 1 (7.7 %) from Scopus. Regarding the country of origin, most of the articles were from international journals, with 2 (15.4 %) from China, 2 (15.4 %) from the Netherlands, and 2 (15.4 %) from the United Kingdom. Germany, Belgium, Brazil, Denmark, the United States of America, Taiwan, and Turkey had 1 (7.7 %) study each.
Table 2 Summary of the Reviewed Articles (n = 13), Belém, Pará, Brazil, 2024
| Code | Author/country/year/ database | Title | Method/level of evidence/ EAMH scale |
|---|---|---|---|
| A (27) | Li X, Lou S, Li J/ China/2023/Embase | Application and effect evaluation of case management nursing practice mode in patients with precision radiotherapy for nasopharyngeal carcinoma | Randomized clinical trial (II) 6 points |
| A (28) | Anagnos VJ, Brody RM, Carey RM, Ravin E, Kendall KB, Newman JG et al./Estados Unidos da América/2023/Embase | Post-operative monitoring for head and neck microvascular reconstruction in the era of resident duty hour restrictions: A retrospective cohort study comparing 2 monitoring protocols | Retrospective cohort study (IV) 5 points |
| A (29) | Otto B, Borzikowsky C, Cristã F, Purz N, Hertrampf C/ Alemanha/2023/ Embase | The influence of diagnoses on patient satisfaction during inpatient stays: a prospective study | Prospective observational study (descriptive) (VI) 6 points |
| A (30) | Li T, Zhang Y, Kong J, Kong M, Meng G, Shi W/ China/2022/Embase | Effect of "timing it right" on comprehensive unmet needs and psychological pain in patients with head and neck cancer undergoing radiotherapy: A randomized controlled trial | Randomized clinical trial (II) 6 points |
| A (31) | Mortensen A, Wessel I, Rogers SN, Tolver A, Jardim M/ Dinamarca/2022 Embase | Needs assessment in patients surgically treated for head and neck cancer: A randomized controlled trial | Randomized clinical trial (II) 6 points |
| A (32) | Braat C, Verduijn GM, Stege HA, Offerman MPJ, Peeters MAC, Staa AL et al./Holanda/2022/ Embase | Evaluation of a nurse-led aftercare intervention for patients with head and neck cancer treated with radiotherapy and cisplatin or cetuximab | Qualitative study (VI) 4 points |
| A (33) | Prins A, Saelens J, Duprez F, Bruycker A, Huvenne W, Deron P/ Bélgica/2021/Embase | Implementation of cancer nurse-led consultations for patients with head and neck cancer through the care pathway: A renewed care | Retrospective cohort study (IV) 4 points |
| A (34) | Waltho A, Thompson D, Pattinson R, Woolley J, Hawthorn T/Reino Unido/2021/Embase | Developing and evaluating a pathway for screening and treatment of depression in patients with head and neck cancer | Descriptive study (VI) 5 points |
| A (35) | Lee P, Chan T/ Taiwan/2015/Embase | Application of integrative information system improves the quality and effectiveness of cancer case management | Descriptive study (VI) 5 points |
| A (36) | Leeuw J, Prns JB, Teerenstra S, Merkx MAW, Marres HAM, Achterberg TV/ Holanda/2013/Embase | Nurse-led follow-up care for head and neck cancer patients: a quasi-experimental prospective trial | Quasi-experimental study (IV) 6 points |
| A (37) | Rogers SN, Clifford N, Lowe D/Reino Unido/2011/Embase | Patient and carer unmet needs: a survey of the British association of head and neck oncology nurses | Descriptive study (VI) 6 points |
| A (9) | Pautasso FF, Lobo TC, Flores CD, Caregnato RCA/Brasil/2020/SciELO | Nurse Navigator: Development of a program for Brazil* | Qualitative study (convergent care) (VI) 6 points |
| A (38) | Duzova US, Pode G/ Turquia/2021/Scopus | The effect of navigation programme on the management of symptoms related to head and neck radiotherapy | Randomized clinical trial (II) 6 points |
Source: Prepared by the authors.
Regarding the publication year, research on the theme has started recently, given that the publication years 2021, 2022, and 2023 had 3 (23.1 %) publications each; the years 2011, 2013, 2015, and 2020 had 1 (7.7 °%) publication each. As for the level of evidence, most of them were Level VI (6) (46.2 °%), Level II (4) (30.8 °%), and Level IV (3) (23.1 °%). In terms of the EAMH score, 8 (61.5 °%) publications scored 6 points, 3 (23.1 °%) scored 5 points, and 2 (15.4 °%) scored 4 points.
The interpretation of the findings enabled the following thematic categories to be compiled: 'Effectiveness of care processes (management and continuity of care);' 'Advanced practices in the navigation of patients with HNCs by nurses,' and 'Evaluation of the results of the navigation of patients with HNCs by nurses.' The synthesis of the evidence is presented in Table 3.
Table 3 Synthesis of the evidence. Belém, Pará, Brazil, 2024
Source: Prepared by the authors.
Discussion
Effectiveness of Care Processes (Management and Continuity of Care)
In this review, it was found that nursing interventions in the navigation of patients with HNCs, from diagnosis until after hospital discharge, included important health-related instructions through health education, not only for patients, but also for family members and/or caregivers regarding the roles of the multi-professional team, hospitalization instructions, and the healthcare system 9,27.
A Chinese study showed the role of oncology nurses in patient navigation significantly reduced the number of patients who did not receive adequate care in the healthcare service and who had difficulties in receiving guidance and follow-up from professionals, either due to the navigators' constant contact with patients, the coordination of continuity of care, referrals, or the fact that the navigators organized and instructed patients on hospitalization processes 39.
A study conducted in Australia with a focus group of seven nurse navigators showed nursing interventions in the navigation of cancer patients include the coordination of patient care and continuity of care through timely referrals between specialized services, such as radiotherapy, and integrated care between points of care; nurses also work as educators, in other words, they train patients, families, and caregivers to make them co-responsible for the care process and facilitate navigation in the cancer care network 40.
In this integrative review, it was found the effectiveness of care processes in HNCs is achieved through case management with communication skills provided by nurses navigating patients with HNCs, enabling the use of communication as a care tool between patients and their families and/or caregivers and the other professionals in the multi-professional healthcare team who are co-responsible for the treatment to establish and improve results 9,27.
In this sense, it can be noted that the navigation of patients with HNCs by nurses has led to the beginning of a political change in healthcare institutions and the creation of forms of management to achieve excellence in navigation through nursing measures, providing the necessary improvements by acting in a leadership position to promote change 41.
Still in this line of thought, longitudinality is part of the care process promoted by nurses in the context of navigating patients with HNCs, perpetuated by supported self-care, which is possible through excellence in consecutive care, referrals to the multidisciplinary team, in addition to monitoring and managing navigation based on integrality, resoluteness, and prioritizing user satisfaction 9,27,35.
Regarding these findings, the evidence showed that navigation was converted into effective care through health education measures, with a significant improvement in patients' understanding, adaptation, and coping with the disease, favoring evaluation, management, and continuity of care due to the fact that nurses in the context of navigating cancer patients represent the communication link between the patient and the multi-professional team 17.
A study that aimed to develop a navigation program for cancer patients, especially for patients with HNCs, conducted in a highly complex center in Brazil, showed that, for care processes to be effective, it is imperative to help patients identify and overcome obstacles to their access to the healthcare system 9, given that diagnosis is sometimes provided late and thus it is necessary to adopt educational measures to help the population identify signs and symptoms and access the system in search of adequate care 40. Therefore, the navigation of patients with HNCs is a promising approach to overcoming obstacles to their access to cancer care and should include patients and their families/caregivers in all processes 9,39.
Therefore, the nurses' competencies in navigating patients with HNC consist of education, collaboration, and communication measures to help patients, family members and/or caregivers overcome obstacles within healthcare services 42, given that cancer patients face physical, psychosocial, and economic obstacles from the moment they are diagnosed onwards 43. Furthermore, cancer patient navigation entails the quality of the close relationship between primary care and the specialized care provided in medium and high complexity, as well as effective communication between patients and nurses to reduce knowledge gaps 44.
However, in the Brazilian scenario, scientific knowledge and empirical/practical knowledge concerning patient navigation and the core role of nurses are still limited, highlighting the urgency of reporting successful experiences capable of expanding this model of professional practice 45.
In any case, the reduction in the drop-out rate 27 from cancer treatment and the allocation of resources 9 are also realities promoted by the nurse navigation program, given that there is a laborious attempt to overcome the organizational and functional deficiencies of healthcare systems, the fragmentation of the support network, and the lack of knowledge about the disease 46. In addition, there are efforts to ensure that resources are available, both to adequately assist patients and to provide continuity of care 47.
[t2] Advanced navigation practices for patients with HNCs by nurses The articles included in this category cover the advanced practices of patient navigation by nurses in the processes related to care for patients with HNCs, especially follow-up after cancer treatment 28,32,36,37. APN is a field in expansion and aims to improve the model of care, as a result of the scientific development in the field of nursing, strengthening the class struggle, with the prospect of achieving and ensuring ethical, scientific, and political values, corroborating with clinical practice 48.
The results of a scoping review showed that nurses, by performing the role of navigators, have an impact, through their actions, on the processes that are interrelated with care, including post-cancer treatment. Thus, it is essential that navigation measures start at the beginning of cancer treatment 49.
Regarding the APN focused on patients with HNCs, the studies in this review indicate self-care as a potential developed via navigation 9,32. A study conducted in Canada, in the province of Ontario, corroborates this finding by emphasizing that self-care is a strategy mapped by nurses, in the context of navigation, regarded as preventive practices to support the care of cancer patients 48. Furthermore, the follow-up of patients with HNC led by nurses who work in patient navigation is a viable alternative to the financial burden that comes with cancer treatment 36. In a Brazilian editorial on APN in Latin America and the Caribbean, the benefits achieved by countries where APN is a reality were highlighted, with results such as oncology user satisfaction scores, a reduction in treatment costs with increased and facilitated access to services, making it an instrument of autonomy for nurses in oncology 50.
The quality of life of patients with HNCs is a variable positively affected by APN since the studies in this review show that nurses who work in navigation in the context of HNCs develop expertise in planning, management, assessment of care, development of better services, and follow-up 29,33,36.
In this regard, studies show that APN, in general, leads to a positive outcome in the care of patients with HNCs in terms of health results, and these results extend to better access to healthcare services and quality of life, with user satisfaction, during and after cancer treatment 51,52.
The results of APN in the context of HNCs also include management and leadership of the multi-professional team through assertive knowledge of the pathology, with the opportunity for shared decision-making between the team, patients, families, and/or caregivers 35,37.
This reality is remarkable and highlights the fact that nurses who work with patients with HNCs develop their role with a focus on care management, possessing the skills to work collaboratively and to inform patients of their health-disease process 17,53.
Evaluation of the Outcomes of Navigation of Patients with HNCs by Nurses
It is clear that patients with HNCs who receive nurse-led navigation receive timely follow-up on the management of the disease, with a significant improvement in needs such as information, pain, improvement in general health, and psychological care 30. A mixed-methods study that researched what makes patient navigation more effective showed that patient navigation is a recognized aspect of high-quality care 54 and, when conducted by nurses, it is mainly responsible for ensuring follow-up without hurdles, strengthening communication, identifying information needs and providing psychosocial and/or emotional support 55. In addition, a randomized controlled clinical trial conducted with 92 surgical patients with HNCs showed in its results that navigation is rooted in the identification and monitoring of patients' needs, including emotional and care needs, as shown in the article 31.
A positive point assessed as an outcome of the navigation of patients with HNCs by nurses is the quality of life as a result of the reduction and adequate management of the severity of symptoms, especially those related to radiotherapy treatment 39. The clinical outcomes of navigating patients with HNCs therefore result in reduced suffering, improvement, and adequate management of symptoms, improved quality and continuity of care and, consequently, quality of life 17.
Thus, as a treatment modality, radiotherapy is used with curative and/or palliative intent to treat early-stage or locally advanced tumors and to manage symptoms in advanced diseases; although technical improvements have reduced the occurrence of radiotherapy-related toxicity, most patients still report side effects associated with the therapy 56.
Radiotherapy-related toxicity compromises the general state of health of people undergoing cancer treatment and negatively influences their quality of life, leading to pain, discomfort, aesthetic changes, and emotional problems 5. For this reason, it is necessary to thoroughly understand the needs of patients with HNCs, including those undergoing radiotherapy to promote measures to improve their quality of life 8.
Conclusion
The evidence from the present review addressed three main aspects, namely: the effectiveness of care processes, such as management and continuity of care, the advanced practices of nurse navigation of patients with HNCs, and the evaluation of the outcomes of nurse navigation of patients with HNCs show improved clinical outcomes in patients with HNCs through nurse navigation at all stages of the cancer patients' line of care.
The nurse's role in navigating patients with HNCs focuses on coordinating continuity of care and monitoring the patient's self-care, which ensures that the patient with HNCs is monitored from diagnosis until after hospital discharge. The focus is on health education, which allows nurses' efforts to encompass comprehensive, co-responsible, and multi-professional care.
Some relevant aspects of the navigation of patients with HNCs by nurses shown by the research were that the nurse's representation of leadership in the navigation of patients with HNCs enhances self-care practices and quality of life in patients with HNCs. It is clear, therefore, that the results of nurse navigation of patients with HNCs constitute an improvement in the oncology specialty, resulting in quality care and follow-up without hurdles for patients, their families/caregivers, and the community.
The review also highlights the fact that the scientific knowledge produced on the theme can be found in countries such as Belgium, Brazil, China, Denmark, the United States, the Netherlands, the United Kingdom, Taiwan, and Turkey, all of which are countries where navigation is a mainstream practice or where efforts have been directed towards its implementation. Therefore, most of the studies found were published in international journals, and the only Brazilian study included was indexed internationally. It can therefore be concluded the study of the navigation of patients with HNCs by nurses has taken its first steps in research in the Brazilian scenario and still needs to be expanded in the Latin American context.
Therefore, it is hoped that this evidence will not only help and encourage Brazilian nursing to organize and implement navigation programs, especially in the context of head and neck neoplasms but also contribute to the publication of studies that present successful experiences in the Brazilian scenario.
The limitations of this review include the fact that the evidence described stems from countries with different care network designs, which hinders broad generalizations of the evidence found for underdeveloped countries, for instance.















