Introduction
Blood transfusion is a common treatment used in clinical settings. It is a therapeutic procedure characterized by the use of blood components for the treatment of various pathologies 1. This is a globally acceptable approach for a range of clinical, surgical, and emergency treatments, as it has shown remarkable efficacy when used adequately. However, this procedure is not exempt from risks, mostly related to the recipient of the blood components 1.
Although all the necessary precautions are followed, transfusion procedures have a great potential for manifesting risks, such as infectious diseases, immunosuppression, and alloimmunization, which means that its practice is restricted to situations where there is a specific clinical recommendation and in the absence of other therapeutic resources 2.
As a prerogative, transfusion can be recommended in situations such as in adults with acute hemorrhage with an Hb < 8.0 g/dl; normovolemic patients who are going to undergo orthopedic surgery or are suffering from gastrointestinal bleeding with an Hb ≤ 7.5g/dl, as a form of prevention; and intensive care unit (ICU) patients using cardiopulmonary bypass, victims of acute neurological injury, or onco-hematological patients 2.
However, hemotransfusion simultaneously has proven beneficial when administered adequately, such as oxygen supply, correction of coagulopathies, control of critical bleeding, and reduction of symptoms associated with anemia, as well as being essential in procedures such as surgeries, treatments, and chemotherapy, which cannot be performed safely without its application 3.
In the Brazilian context, the National Health Surveillance Agency (Agência Nacional de Vigilância Sanitária - Anvisa) reports that 84.21 % of transfusion reactions reported are mild and immediate 4. This scenario is validated by the epidemiological index, since febrile hemolytic reactions, infection, acute lung lesions related to transfusion, and graft-host disease are some of the complications stemming from transfusion reactions 5.
Furthermore, transfusion reactions can be avoided, as numerous transfusion-related events are caused by human error 5,6. The most common errors are incorrect identification of the recipient and incorrect sample labeling at the time of blood transfusion. These are responsible for 80 % of reported events and preventing them could avert 45 % of deaths 7,8.
Measures that promote a culture and infrastructure that reduce risks in healthcare are part of patient safety. Despite these efforts, approximately one in ten patients in rich countries and one in four in poor countries suffer avoidable errors, increasing healthcare costs and causing approximately 2.6 million deaths 9. In this sense, hemotherapy procedures should be conducted by trained nurses, as the transfusion of blood and blood components requires knowledge entailing its application, risk management, and timely measures to effectively intervene in possible complications 10. These professionals have an important role in the safe conduct of hemotherapy, detecting signs and symptoms of reactions in the various stages of the transfusion chain 11.
Considering the physical proximity that nurses have to patients and the care they provide, which must be effective and safe, these professionals need accurate knowledge and should receive a thorough education on the transfusion process while still completing their undergraduate studies to ensure safe patient care. Thus, transfusion safety is improved by measures designed to reduce the probability of human error. This implies that the use of educational techniques such as clinical simulations to achieve this goal can be effective measures even employed during undergraduate training. The implementation of plans to improve healthcare safety is included in the Global Action Plan for Patient Safety 2021-2030 12,13.
With the implementation of patient safety measures, the goal is to reduce the risk of harm related to the healthcare provided. Considering the importance of this theme, the World Health Organization established the Global Alliance for Patient Safety in 2004, setting three global challenges: Safe surgeries, hand hygiene, and harm-free medication. Blood transfusion, just as any other health procedure, offers benefits, but is not exempt from risks that can be fatal. It is therefore necessary to adopt integrated measures to ensure safe care in this setting to avoid partial or fatal injuries. Under these circumstances, patient safety consists of a set of practices that enable the creation of a culture, structure, processes, conduct, and technologies to reduce the risks related to healthcare, as well as consolidate their impact in the event of complications.
Despite the efforts directed towards the development of strategies to help improve patient safety, estimates indicate that, in developed countries, one in ten patients is subject to preventable errors related to healthcare, and this figure is higher in underdeveloped or developing countries, where one in four patients is subject to them 9.
In this context, nursing bears a strategic role in providing care and managing risks related to the transfusion process. The interventions performed by the nursing team aim to prevent complications and adverse reactions, thus ensuring the patient's safety and well-being. Nursing care is implemented before, during, and after transfusion. Therefore, due to their role in the transfusion process, nurses' knowledge and practices regarding blood transfusion contribute to patient safety and improved care 14.
The provision of safe patient care relies on the strategies adopted by the nursing team in the service in question. The implementation of protocols and instruments is essential for providing safe care. Regarding safe transfusion care, Anvisa has implemented Collegiate Board Resolution (Resolução da Diretoria Colegiada - RDC) No. 153/2004, which establishes a technical regulation for hemotherapy practice, covering procedures from the collection to the use of blood and blood components in human beings. Documents such as this enable the development of systematized care, contributing to the provision of safe care 15.
In light of the need to promote research and effective, safe care that contributes to patient safety, this scoping review is justified as it allows mapping nursing care for adults undergoing blood transfusion. It is believed that this research will help to identify gaps and suggest ways of developing safe care standards and advancements in the models already outlined in the literature.
Therefore, this review aims to map the scientific production related to nursing care for adults undergoing blood transfusion in the light of patient safety.
Materials and Methods
This is a scoping review, which was created in line with the methodology developed by the Joanna Briggs Institute Reviewer's Manual for Scoping Reviews and followed the guidelines of the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews Checklist (Prisma-ScR). This review was registered on the Open Science Framework Registries platform, under the identifier https://osf.io/7cqjs/ 16,17.
To map the publication landscape on the theme, especially to identify similar reviews or protocols, a search was conducted on the following platforms: Open Science Framework (OSF); The Cochrane Library; JBI Clinical Online Network of Evidence for Care and Therapeutics (ConNECT+); Database of Abstracts of Reviews of Effects (Dare); and Prospective Register of Systematic Reviews (Prospero). After the searches, the absence of similar materials was confirmed. This type of study aims to identify, map, and synthesize the evidence and gaps in the existing knowledge in a given field of research. This process preserves methodological rigor through the following outline: identification of the research question; identification of relevant studies; study selection; data analysis and extraction; and data synthesis and presentation 16,17.
The research question was devised using the core elements of the PCC acronym (Population-Concept-Context [17]), in which 'P' (population) represents hospitalized adult patients; 'C' (concept), nursing care; and 'C' (context), patients undergoing blood transfusion. In light of this, the following question was drawn: Which forms of nursing care are provided to hospitalized adult patients undergoing blood transfusion?
The searches were conducted in March and April 2024 in the following databases: Scopus, Web of Science, PubMed/Medline, Latin American and Caribbean Health Sciences Literature (Lilacs), Cumulative Index to Nursing and Allied Health Literature (Cinahl), BDEnf, and IBECS. In addition, a search for publications was conducted on Google Scholar.
A survey of the free and controlled vocabularies used in publications written on the proposed theme was conducted, which were considered when designing the search strategies for the publications, as shown in Table 1; these were adapted to each database, using the Boolean operator AND. Searches were limited to materials published from 2017 to March 15, 2024. The period was selected based on relevant advances in hemotransfusion practices identified in 2017, such as the dissemination of care 14.
Table 1 Search strategy for document retrieval. Imperatriz, Maranhão, Brazil, 2024
| Database | Search strategy |
|---|---|
| Medline (via PubMed) | (“Nursing Care”[MeSH Terms] AND (“Blood Transfusion”[MeSH Terms]) |
| Scopus | TITLE-ABS-KEY (“Nursing Care” AND “Blood Transfusion”) |
| Web of Science | ((TS = (“Nursing Care”) AND TS = (“Blood Transfusion”)) (All Fields) |
| Lilacs | Cuidados de Enfermagem AND Transfusão de Sangue |
| BDEnf | Cuidados de Enfermagem AND Transfusão de Sangue |
| IBECS | Atención de Enfermería AND Transfusión Sanguínea |
| Cinahl | MH Nursing Care AND AB Blood Transfusion |
Source: Prepared by the authors.
The following eligibility criteria were considered: Primary studies whose authors addressed nursing care for adult patients undergoing blood transfusion; published in Portuguese, English, or Spanish; from January 2017 to March 2024. The following were excluded from the review sample: Descriptions of integrative, systematic literature review and/or meta-analysis studies, as well as reflection articles and articles that addressed the theme but did not describe the care provided. The time frame was established to limit the scope of the review to a manageable number of studies to ensure the quality and relevance of the data analyzed.
The Mendeley reference manager was used to eliminate duplicates of the publications exported from the six databases, and the Rayyan web application was used to assist in the organization and selection of articles; in addition, the searches were conducted from November 2023 to March 2024.
For the study selection process, two independent reviewers examined the titles and abstracts. The full text was selected for analysis when there were doubts concerning the relevance of a study based on its abstract. The full articles were randomly assigned to each reviewer. In addition, two reviewers conducted an independent review of the full text of the articles to determine whether they met the inclusion criteria and answered the core question of the review. In case of disagreement, a third reviewer was consulted to delimit the inclusion of the study. The authors of this manuscript were reviewers for all stages.
To extract the content, an instrument structured by the authors was used, considering the following variables: Article identification (ID), year, publication country, type of study, level of evidence classified as described by Melnyk and Fineout-Overholt 18, classified from one (I) to seven (VII) levels of nursing care; and other relevant situations among the selected studies. The reviewers mapped the data independently, discussed the results, and continually updated the data mapping form in an interactive process, in line with JBI guidelines 17.
The research was based exclusively on public domain data, eliminating the need for submission to a research ethics committee, in compliance with Resolution 510/2017. It should be noted that copyright has been duly preserved through adequate citation and bibliographic reference.
Results
The flowchart of the selection process for the primary studies included in the scoping review is presented in Figure 1. Therefore, of the 515 publications found in the databases, after applying the eligibility criteria, 26 primary studies were selected to be read in full and 19 comprised the review sample.
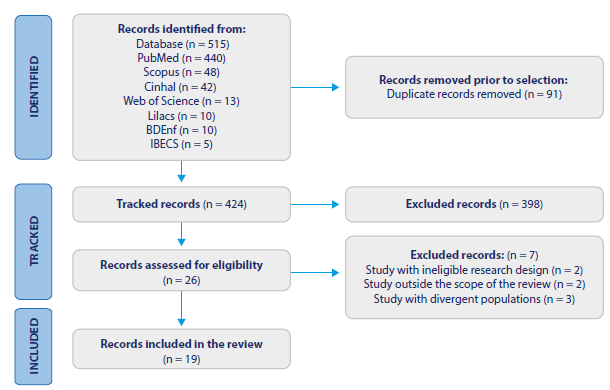
Source: Prepared by the authors.
Figure 1 Flowchart of the Selection of Publications for the Scoping Review in Line with Prisma-ScR guidelines. Imperatriz, Maranhão, Brazil, 2024
Among the countries in which the studies were conducted, this article found that most of the published studies were from Brazil, with a total of six (33.3 °%) studies, with a less dense distribution among the other countries analyzed, as shown in the thematic map in Figure 2, which is a proportional choropleth representation of the distribution of articles.
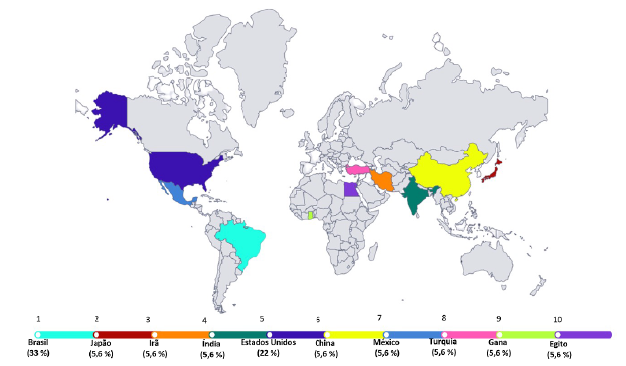
Source: Prepared by the authors.
Figure 2 Distribution of the Frequency of Articles Published by Country. Imperatriz, Maranhão, Brazil, 2024
The articles included in this review were from 10 countries, including Brazil (n = 6), Japan (n = 1), Iran (n = 1), India (n = 1), the United States (n = 5), China (n = 1), Mexico (n = 1), Turkey (n = 1), Ghana (n = 1), and Egypt (n = 1). Most of the studies included were cross-sectional (n = 9), qualitative (n = 3), experience report (n = 1), methodological (n = 1), observational (n = 3), pilot (n = 1), and exploratory (n = 1).
In general, the nursing care presented in this review was provided in a hospital setting and one instance took place in a hemotherapy reference unit, as shown in Table 2. The studies cited trauma, emergency, medical-surgical wards, ICU, and oncology units as hospitalization sites.
Table 2 Synthesis of the Studies Included in the Review, with Characterization, Level of Evidence, and Nursing Care. Imperatriz, Maranhão, Brazil, 2024
| ID/Year/Publication Country | Type of Study/Level of Evidence |
|---|---|
| Nursing Care | |
| S1(19)/2021/Brazil | Cross-sectional study/VI |
| 1. Perform hand hygiene; 2. Use personal protective equipment (gloves and masks); 3. Check and verify medical prescriptions; 4. Confirm the patient’s full name; 5. Compare patient data with blood bag data; 6. Double-check the data; 7. Document in the patient’s protocol whether the correct blood component has been transfused; 8. Perform peripheral venipuncture; 9. Administer blood pre-transfusion medication; 10. Connect the equipment to the blood bag using an aseptic technique; 11. Check label compliance; 12. Perform macroscopic inspection of the blood bag; 13. Check the blood bag’s integrity; 14. Monitor the patient closely and personally for the first 10 minutes; 15. Monitor the patient during the transfusion; 16. Check vital signs: 30min/1h/2h/3h/4h. | |
| S2(20)/2021/Brazil | Qualitative study/VI |
| 1. Communicate effectively with the hemotherapy center to avoid irregularities and ensure product availability; 2. Check the need for transfusion in the perioperative period, considering the patient’s physiological conditions and clinical referrals; 3. Secure adequate venous access with a large-bore catheter to ensure effective transfusion and prevent red cell hemolysis; 4. Use specific equipment, such as 170μ filters, to prevent the formation of clots and aggregates during transfusion; 5. Check the blood bag for air bubbles and the right consistency to ensure the safety of the procedure; 6. Constantly monitor the patient’s vital signs and watch for possible adverse reactions during and after the transfusion; 7. Correctly identify the patient before the transfusion to avoid administration errors; 8. Promote patient education and empowerment in relation to blood transfusion. | |
| S3(21)/2023/Brazil | Cross-sectional exploratory study/VI |
| 1. Ensure the transfusion label is attached to the bag throughout the procedure; 2. Interrupt the transfusion immediately, maintain intravenous access, and inform the medical doctor of any signs of an adverse reaction, such as restlessness, hives, nausea, vomiting, back pain, fever, or chills; 3. Check on the patient periodically to enable early detection of adverse reactions. | |
| S4(1)/2019/Brazil | Quali-quantitative and explanatory study/VI |
| 1. Recognize the signs and symptoms of a transfusion reaction; 2. Know which course of action to take in the event of complications during transfusion; 3. Understand what to do with the blood component after use; 4. Identify the differences between transfusion associated with circulatory overload (Taco) and transfusion-related acute lung injury. | |
| S5(22)/2021/Brazil | Analytical cross-sectional study with a quantitative approach/VI |
| 1. Infuse the red blood cell concentrate within the time allowed; 2. Avoid administering medications simultaneously in the same venous access as the transfusion; 3. Perform direct and individualized transfusion monitoring, focusing on preventing failures; 4. Knowledge of the ABO system to avoid acute hemolytic reactions, ensuring compatibility between donor and recipient; 5. Be aware of the maximum infusion time for a red blood cell concentrate, which should not exceed 4 hours to avoid the risk of bacterial proliferation and sepsis; 6. Interrupt the transfusion in the event of an adverse reaction, notify the medical doctor and nurse, store the blood bag and notify the transfusion agency; 7. Identify the signs and symptoms of an immediate transfusion reaction, such as fever, chills, pain, and changes in blood pressure, among others, to intervene quickly and adequately; 8. Be prepared to manage different types of transfusion reactions, such as acute hemolytic reactions, circulatory overload, bacterial contamination, and hypotension; 9. Follow established standards and protocols, such as RDC 34, which advises healthcare professionals on how to monitor and identify adverse events during transfusion. | |
| S6(23)/2022/Brazil | Exploratory, descriptive, and prospective study/VI |
| 1. Check patient identification data; 2. Check sample identification data; 3. Check vital signs at the start of the transfusion; 4. Check vital signs at the end of the transfusion; 5. Report on transfusion reactions; 6. Write notes covering the first 10 minutes 7. Check vital signs 30 minutes after transfusion. | |
| S7(24)/2021/Brazil | Qualitative study/VI |
| 1. Check the patient’s clinical condition; 2. Check vital signs (before, during, and after transfusion); 3. Record the necessary pre-transfusion information; 4. Perform double-checks; 5. Identify patients with a potential risk of transfusion reaction; 6. If necessary, fill in the transfusion reaction investigation form and collect a sample for laboratory analysis; 7. Guide the patient over the signs suggestive of a transfusion reaction. | |
| S8(25)/2020/United States | Experience Report/VII |
| 1. Have at least two people check the patient’s name and medical record number; 2. Have at least two people check the patient and the product to be transfused; 3. Identify the patient’s blood type and Rh; 4. Screen the patient’s plasma for antibodies; 5. Ensure the label is attached to the bag during the transfusion; 6. Record the time and date of blood collection on the form. | |
| S9(26)/2022/United States | Methodological study/VI |
| 1. Continuously check vital signs; 2. Continuously monitor patients during transfusion; 3. Review clinical data in real time by nurses specialized in hemovigilance; 4. Respond quickly to possible transfusion reactions, with immediate intervention by trained healthcare professionals; 5. Educate and implement auditing programs to raise awareness of transfusion reactions. | |
| S10(27)/2020/United States | Retrospective observational study/VI |
| 1. Monitor and maintain constant control of blood administration throughout the procedure by specialized nurses; 2. Reduce the infusion of solutions into the patient during transfusion. | |
| S11(28)/2019/United States | Pilot study/III |
| 1. Review patient history and risk factors for adverse events associated with transfusion (advanced age; multiple units transfused within the last 24 hours; history of renal or cardiac insufficiency); 2. Confirm the provision of informed consent; 3. Confirm patient identification; 4. Confirm that the IV catheter is working; 5. Physical assessment (lung sounds); 6. Skin assessment; 7. Check vital signs pre-, intra-, and post-transfusion; 8. Notify the medical doctor in the event of any abnormal findings during the assessment; 9. Assess the patient 15 minutes after starting the transfusion; 10. Assess evidence of adverse events (chills, back pain, urticaria, dyspnea, tachycardia, cough, rales, hypotension, hypertension, increased pulse pressure, decreased O2 saturation) within the intra- and post-transfusion period; 11. Interrupt transfusion if there is a sign of an adverse event; 12. Notify the medical doctor if there is any sign of an adverse event; 13. Perform post-transfusion physical assessment; 14. Discard the blood product and blood tube if there are no signs of an adverse event; 15. Document the infused volume in the patient’s clinical record. | |
| S12(29)/2021/Japan | Cross-sectional descriptive study/VI |
| 1. Have two professionals check the patient during the collection of pre-transfusion blood samples; 2. Have two people (medical doctor and nurse) check the blood administration; 3. Perform electronic pre-transfusion verification using an electronic identification system before blood administration; 4. Raise awareness of blood transfusion safety after completing the electronic pre-transfusion check using an electronic identification system; 5. Perform a double-check of the bag label. | |
| S13(30)/2021/Iran | Cross-sectional descriptive study/VI |
| 1. Adequately identify the patient before transfusion; 2. Precisely document the blood transfusion; 3. Use warmed blood when necessary; 4. Determine the correct time to start the transfusion; 5. Adequately regulate the blood transfusion flow rate; 6. Know the adequate duration of the transfusion; 7. Know how to use medications/solutions with blood simultaneously; 8. Monitor the patient closely for possible reactions to the transfusion. | |
| S14(31)/2021/India | Cross-sectional descriptive study/VI |
| 1. Check patient details with the blood bag at the bedside; 2. Administer intravenous fluids compatible with the blood; 3. Infuse the red blood cell concentrate within the maximum time allowed; 4. Return the transfusion reaction form to the blood bank; 5. Return the blood to the blood bank if not transfused within the allotted time; 6. Respect the maximum time allowed for blood to be kept at room temperature before transfusion; 7. Dispose of waste adequately; 8. Warm the red blood cell concentrate before transfusion; 9. Monitor the patient after the transfusion; 10. Check the size of the catheter to be used for routine transfusion; 11. Analyze the transfusion rate of concentrated red blood cells in non- emergency situations; 12. Administer pre-transfusion medications. | |
| S15(32)/2024/China | Retrospective observational study/VI |
| 1. Warm the blood bag before infusion; 2. Monitor vital signs with stress indicators; 3. Practice predictive nursing measures; 4. Prepare the blood and blood components for shock rescue; 5. Heat disinfection materials, washing fluids, infusion bags, and blood transfusion sets; 6. Control the room temperature during operation to maintain a warm and comfortable environment for the patient. | |
| S16(33)/2021/Mexico | Descriptive observational study/VI |
| 1. Check the number of units, volume, identification number of health units, blood, or complement; 2. Record the date and time of the start and end of the transfusion; 3. Record the procedures conducted in cases of transfusion reactions 4. Record vital signs in the pre-, trans-, and post-transfusion periods; 5. Check the medical prescription; 6. Adequately record the number of units, volume, and identification number of the blood units or complement; 7. Control the vital signs before, during, and after the blood transfusion, this being a lower performance criterion; 8. Systematically perform the blood product administration technique. 9. Continuously assess the patient during the administration of blood products. 10. Prevent errors in the selection and administration of blood products. 11. Prevent and control possible transfusion-related complications. | |
| S17(34)/2024/Turkey | Descriptive and cross-sectional/VI |
| 1. Administer the correct blood and blood products to the correct patient at the adequate time; 2. Monitor the patient for adverse reactions during and after transfusion; 3. Provide feedback to the blood center; 4. Implement measures to reduce the risk of transfusion-related complications; 5. Actively participate in the entire transfusion process, from the blood and blood product collection to the post-transfusion period. | |
| S18(35)/2021/Ghana | Descriptive cross-sectional study/VI |
| 1. Interrupt the transfusion immediately if there are signs and symptoms of a reaction; 2. Check and record vital signs 30 minutes before starting the transfusion; 3. Identify the correct patient; 4. Guide the patient or their family regarding blood transfusion, its benefits, associated risks, and symptoms of transfusion reactions; 5. Warm the blood in cases where it is necessary (cases of rapid/massive transfusion, exsanguinotransfusion in babies, in patients with cold agglutinins, and in trauma cases where basic rewarming measures are necessary); 6. Define the adequate flow rate of the transfusion; 7. Document the care provided throughout the transfusion process. | |
| S19(36)/2020/Egypt | Descriptive cross-sectional study/VI |
| 1. Check the information on the bag label and perform a double-check; 2. Check and identify the correct patient; 3. Administer blood components at the adequate time; 4. Use the adequate aseptic technique in administration and preparation; 5. Monitor signs and symptoms of circulatory overload; 6. Check for signs of a reaction within the first 15 minutes of the transfusion; 7. Check vital signs every hour during the transfusion. | |
Source: Prepared by the authors.
The results show that the care mapped is related to the pre-, intra-, and post-transfusion phases. In addition, simple precautions, such as hand hygiene, are essential for ensuring safe transfusion care. Table 3 shows the main nursing care associated with adult patients undergoing blood transfusion, according to the data collected in this synthesis.
Table 3 Synthesis of the most Prevalent Nursing Care in the Studies. Imperatriz, Maranhão, Brazil, 2024
| Nursing care | f = Frequency (n = 19) | % (n = 19) |
|---|---|---|
| Check vital signs: S1, S2, S6, S7, S9, S11, S15, S16, S18, S19 | 10 | 52.6 |
| Monitor the patient during the transfusion: S1, S3, S5, S9, S10, S16 | 6 | 31.5 |
| Perform double-checks: S1, S7, S8, S12, S19 | 5 | 26.3 |
| Interrupt the transfusion immediately in the event of a transfusion reaction: S3, S5, S9, S11, S18 | 5 | 26.3 |
| Nursing care | f = Frequency (n = 19) | % (n = 19) |
| Avoid administering medications through the same access: S5, S10, S13 | 3 | 15.7 |
| Warm the blood bag before infusion: S14, S15, S18. | 3 | 15.7 |
| Advise the patient/family on the benefits and associated risks of blood transfusion and transfusion reactions: S7, S9, S18 | 3 | 15.7 |
| Check and confirm the medical prescription: S1, S16. | 2 | 10.5 |
| Administer pre-transfusion blood medication: S1, S14 | 2 | 10.5 |
| Use the adequate aseptic technique for administration and preparation: S1, S19 | 2 | 10.5 |
| Use personal protective equipment (gloves and masks): S1 | 1 | 5.2 |
| Perform hand hygiene: S1 | 1 | 5.2 |
Source: Prepared by the authors.
Discussion
This review mapped primary evidence that showed great thematic relevance, but which is still underexplored in the literature. It summarized several types of evidence related to nursing care for adult patients undergoing hemotransfusion, which should be implemented in care to improve effective and safe care. These findings highlight the need for professionals to adhere to good practices.
Among the various types of care provided by the nursing team to patients undergoing blood transfusion, after analyzing the selected studies, it was found that the most common are checking vital signs, double-checking, monitoring the patient during the transfusion, and interrupting the transfusion immediately in the event of a transfusion reaction. In total, 10 studies mentioned "check vital signs," which corresponds to 52.6 %; the second most common nursing care was "monitor the patient during the transfusion," with 31.5 °%. Other precautions mentioned were: "perform a double-check," and "interrupt the transfusion immediately in the event of a transfusion reaction," both representing 26.3 %; "avoid administering medications through the same access," "warm the blood bag before infusion," and "advise the patient/family on the benefits and associated risks of blood transfusion and transfusion reactions" represented 15.7 °%; "check and verify the medical prescription," "administer pre-transfusion blood medication," and "use the adequate aseptic technique in administration and preparation" represented 10.5 %; "use personal protective equipment (gloves and masks)" and "perform hand hygiene" represented 5.2 °%.
It was found that checking vital signs, double-checking, monitoring the patient during the transfusion and interrupting the transfusion immediately if the patient experiences a transfusion reaction are important tasks to ensure safe, effective, and quality nursing care in terms of patient safety 19,21,29,30.
Hand hygiene is an essential, simple, effective, and low-cost method that is widely used in the healthcare sector, including nursing. Its importance for patient safety is undeniable, and it is important for preventing infections 37. Adherence to this practice can vary due to various factors, such as risk perception, organizational culture, supervision, and availability of resources. It is crucial to promote and emphasize the importance of hand hygiene to ensure patient safety and well-being 38.
In this review, this type of care was only highlighted by one study, representing 5.2 °% of the total. Similarly, a study that assessed the administration of medication by nursing students and another that assessed the knowledge and practice of nurses and students showed the importance of performing the hand hygiene procedure and suggested increasing strategies for greater adherence to this practice 39-41. This presents an opportunity to improve patient safety during transfusions and to prevent patient complications.
The present study highlights the importance of nursing care during blood transfusions, emphasizing the need for rigorous practices to ensure patient safety. While some studies emphasize hand hygiene, detailed checking of patient data, and constant monitoring during transfusion, others highlight the checking process by two professionals at different stages of the process, including sample collection and blood administration. Similarly, some studies highlight the importance of double-checking, the use of personal protective equipment, and careful monitoring of the patient's vital signs, all of which contribute to preventing errors and promoting safety during blood transfusion 42,43. However, there is still a need for studies that assess the establishment of these precautions.
The administration of any medication into the same venous access used for transfusions can result in serious complications for the patient, including death 44. Two studies highlighted the importance of avoiding the simultaneous administration of medications into the same venous access used for transfusions, a precaution presented in 10.5 °% of the studies 45,46. These results raise a significant concern due to the crucial importance of this care in patient safety 47.
Therefore, working jointly with risk managers to analyze transfusión practices raises awareness and leads to the implementation of corrective measures. In addition, studies suggest the need for training as, despite the regular training, there are malpractices that need to be addressed through periodic training to raise the culture of safe care 48,49.
The studies used to develop the review address issues related to the transfusion process and show a range of nursing interventions targeting blood transfusion. Checking vital signs (blood pressure, heart rate, respiratory rate, and temperature) includes the pre-, trans-, and post-transfusion periods since the pre-transfusion period begins 10 minutes before the infusion 50. Last but not least, it is worth highlighting the importance of immediately interrupting the transfusion at the sign of transfusion reactions 51.
The literature covering the standardization of nursing care for adult patients undergoing blood transfusion is limited. In Brazil, although there is legislation defining the roles of the nursing team and standard operating procedures in hospitals, these materials are not widely disseminated in the relevant literature. The studies included in this review report similar barriers in f other contexts.
The scoping review on nursing care for adult patients undergoing blood transfusion shows that, despite the existence of widely accepted guidelines for transfusion practices, there is a significant gap in the development of specific protocols that ensure the safety and quality of care. The development of such protocols is essential for achieving international transfusion safety targets, which aim to minimize the risks associated with transfusions, such as adverse reactions and infections.
The studies analyzed highlight several aspects of nursing care, including identifying the patient, checking blood type, monitoring vital signs, and monitoring for possible adverse reactions. However, the regulation and standardization of procedures warrant more attention, as the lack of clear regulations can lead to variability in practices and subsequent errors. Adequate training for nursing professionals, efficient adverse event reporting systems, and strict informed consent protocols are crucial to protect patients and ensure that care is in line with international best practices.
In terms of the limitations of the study, the scarcity of materials that explicitly address nursing care for adults undergoing blood transfusion stands out as a limiting factor for the progress of evidence-based discussions on the theme. Despite mapping nursing care in blood transfusion, this study has limitations. The prevalence of Brazilian research, methodological heterogeneity, and the lack of quantitative and cost-effectiveness analyses reduce the generalizability and robustness of the results. The restriction to adult patients in hospitals limits its applicability, while the lack of standardization in care and data on training are relevant gaps. Future studies should address these issues with cost analyses and standardized protocols for greater transfusion safety.
The contributions of this study to the field of healthcare, especially nursing, are based on mapping nursing care in the context of patient safety regarding transfusion. In addition, it provides solid evidence that can support the development of protocols for the implementation of a transfusion safety policy.
The findings of this review can be integrated into daily clinical practice by adopting evidence-based protocols that improve transfusion safety. Continuous training for nursing personnel, the use of technologies for identity verification and blood component tracking, as well as the implementation of protocols for rapid response to adverse reactions, are essential measures. Strict monitoring of vital signs and double-checking during transfusion reduce risks, while patient and family education contributes to the early recognition of complications. These strategies improve the culture of patient safety, promoting more effective care in line with the best practices in transfusion nursing.
Conclusion
The present study mapped nursing care for hospitalized patients undergoing blood transfusion. In this context, this research contributes significantly to the knowledge field by highlighting safe behaviors that improve the standard of care for patients undergoing transfusion therapy.
The main precautions mapped in the present study were checking vital signs, double-checking, monitoring the patient during the transfusion, and interrupting the transfusion immediately if the patient has a transfusion reaction. In addition, the need to work on the standardized development of techniques such as hand hygiene as a safety culture in transfusion assistance was exposed.
Based on the scoping review conducted, it can be concluded that there is a vast field to be explored to create protocols and practices that meet international transfusion safety culture targets.















