Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Biomédica
Print version ISSN 0120-4157On-line version ISSN 2590-7379
Biomédica vol.31 no.3 Bogotá July/Sept. 2011
ARTÍCULO ORIGINAL
The Colombian Histoplasmosis Study Group7
1Facultad de Medicina, Universidad de Antioquia, Medellín, Colombia
2Corporación para Investigaciones Biológicas, Medellín, Colombia
3Grupo de Microbiología, Instituto Nacional de Salud, Bogotá, D.C., Colombia
4Escuela de Ciencias de la Salud, Universidad Pontificia Bolivariana, Medellín, Colombia
5Hospital La María, Medellín, Colombia
6Escuela de Microbiología, Universidad de Antioquia, Medellín, Colombia
7The Colombian Histoplasmosis Study Group (described at the end)
Author contributions: Myrtha Arango played an important role in the development of the project, revised the questionnaires and ascertained their completeness, participated in the analysis of the data and in the writing process. Elizabeth Castañeda conceived the plan for the surveillance program, orchestrated connections with hospitals, diagnostic centers and worked all along the development of the study, including writing and analyzing the manuscript. Clara Inés Agudelo worked all along in the surveillance study, played an important role in preparation of the manuscript and in analysis of the data, including statistical tests. Catalina De Bedout was in charge of the mycologic diagnosis for all CIB cases, established links with physicians in charge of patients, and controlled receipt of questionnaires. Carlos A. Agudelo was the physician in charge of most of the CIB patients, checked the questionnaire´s contents for medical accuracy, and analyzed the data statistics. Ángela María Tobón examined many of the CIB patients, filled in the corresponding questionnaires, supervised the clinical aspects of most patients, and served as a consultant for other physicians in charge of histoplasmosis patients. Melva Linares was in charge of the mycologic diagnosis for all INS cases, established links with physicians in charge of patients, and controlled receipt of questionnaires. Yorlady Valencia was in charge of completing and searching for missing information in questionnaires of the CIB patients and transferring information to the corresponding database. Ángela Restrepo did the surveillance of the whole program, contacting physicians and serving as consultant for all participants, analyzing data, writing the manuscript and analyzing results.The Colombian Histoplasmosis Study Group is a large group composed by all physicians and clinical personnel filling in the questionnaires when diagnosing a histoplasmosis case.
Recibido: 16/12/10; aceptado:03/05/11Introduction. Histoplasmosis, a fungal disorder characterized by a wide spectrum of manifestations that range from subclinical infections to disseminated processes, affects both immunocompetent and immunosuppressed individuals. Histoplasmosis is not a reportable disease in Colombia and consequently, a survey was designed to collect histoplasmosis cases diagnosed in the country.
Objective. The aim of this work was to analyze the data collected from 1992 to 2008.
Materials and methods. The survey included demographic data, risk factors, clinical manifestations, imaging data, diagnostic methods and antifungal treatment. Patients were grouped according to risk factors and comparisons of the various findings were done.
Results. A total of 434 surveys were gathered from 20 of the countryâs Departments. Most patients (96.1%) were adults, 77% were males with a mean age of 38.4 years. Only 3.9% were children less than 15 years of age. In the adult population, AIDS was reported in 70.5% of the cases; additionally, in 7.0% patients other immunosuppressive conditions were informed. The most frequent clinical manifestations were fever (76.1%), cough (54.8%) and constitutional symptoms (56.8%). X rays abnormalities were represented mainly by infiltrates (65.9%) and nodules (17.1%). Diagnosis was made by microscopic observation of H. capsulatum in 49.6% patients, by culture in 58.0% and by serological test in 14.6% cases. Antifungal use was recorded in 52.5% cases.
Conclusions. Histoplasmosis is frequent in Colombia, especially in certain risk factor groups such as the HIV-infected population. Data collected from this large number of cases has allowed valid comparisons on various aspects of histoplasmosis in Colombia.
Key words: histoplasmosis, surveillance, acquired immunodeficiency syndrome, children, disseminated histoplasmosis, Colombia.
Histoplasmosis en Colombia: resultados de la encuesta nacional, 1992-2008
Introducción. La histoplasmosis está caracterizada por variadas manifestaciones que van desde la afección subclínica a la enfermedad diseminada, y suele presentarse tanto en huéspedes inmunocompetentes como inmunosuprimidos. Como la enfermedad no es de notificación obligatoria en Colombia, se diseñó una encuesta para recolectar información de los casos diagnosticados en el país.
Objetivo. El objetivo de este trabajo fue analizar los datos recolectados desde 1992 hasta 2008.
Materiales y métodos. La encuesta incluyó datos demográficos, factores de riesgo, manifestaciones clínicas, estudios de imágenes, métodos diagnósticos y tratamiento antifúngico. Los pacientes se agruparon de acuerdo con los factores de riesgo y se compararon los correspondientes hallazgos.
Resultados. Se examinaron 434 encuestas provenientes de 20 de los departamentos colombianos. La mayoría (96,1 %) correspondían a adultos, 77 % eran hombres con edad promedio de 38,4 años, y sólo 3,9 % eran niños o adolescentes. En los adultos, 70,5 % tenían sida y 7 % presentaban otra inmunosupresión. Las manifestaciones predominantes fueron fiebre (76,1 %), tos (54,8 %) y síntomas constitucionales (56,8 %). En las radiografías, las anormalidades fueron principalmente infiltrados (65,9 %) y nódulos (17,1 %). El diagnóstico se estableció por observación microscópica de H. capsulatum en 49,6 % casos, por cultivo en 58 % y por pruebas serológicas en 14,6 %. El tratamiento se informó sólo en 52,5 % casos.
Conclusiones. Se demostró que la histoplasmosis es frecuente en Colombia, especialmente en grupos de riesgo como son los pacientes infectados con el VIH. El análisis de este número relevante de pacientes permitió establecer comparaciones válidas sobre aspectos de la histoplasmosis en nuestro país.
Palabras clave: histoplasmosis, vigilancia, síndrome de inmunodeficiencia adquirida, niños, histoplasmosis diseminada, Colombia.
Histoplasmosis is an endemic fungal infection of the Americas caused by the thermally dimorphic soil inhabitant fungus Histoplasma capsulatum var. capsulatum (1). Endemic areas have been defined in the United States especially in the Ohio and Mississippi river valleys, as well as in Central and South America (1-3).
H. capsulatum and its recently described clades,grow in vitro at 25°C and in the environment as a mold, which reproduces asexually by microconidia (2-5 µm), considered as the infectious propagules, and also by macroconidia (8-14 µm). At 37°C in vitro and in the infected tissues, it grows as a yeast cell reproducing by blastoconidia, considered the parasitic phase of the fungus (4).
In normal hosts most infections (over 90%) are asymptomatic or self-limited; however, in a few of these hosts, histoplasmosis may be a severe pulmonary disease requiring antifungal therapy. On the contrary, in immunocompromised individuals, such infections are not only severe but result in progressive disease with hematogenous dissemination and a variety of clinical manifestations. Any organ can be affected, especially lungs, bone marrow, skin, brain, adrenal glands, and the gastrointestinal tract (4,5).
In the 1980s, disseminated histoplasmosis due to H. capsulatum was described in HIV-infected patients in the histoplasmosis endemic areas of the United States. Disseminated histoplasmosis was later included in the list of opportunistic infection defining AIDS. Despite the increased use of highly active antiretroviral therapy (HAART), histoplasmosis remains an important opportunistic infection among HIV patients in endemic areas and frequently appears as the first manifestation of HIV infection or as the AIDS-defining illness (6-9).
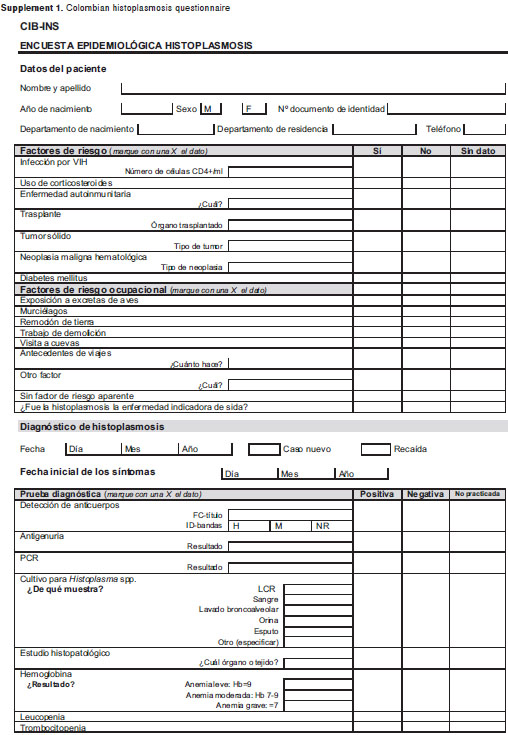
Due to the fact that histoplasmosis is not a reportable disease in Colombia and recognizing the need to better understand the characteristics of this mycosis in the country, the medical mycology groups of the Instituto Nacional de Salud (INS) and the Corporación para Investigaciones Biológicas (CIB) prepared in 1997 a questionnaire following the indications of the European Committee of Medical Mycology (10) and with their authorization distributed it amply to clinicians and laboratory personnel. Additionally, the organizing laboratories transferred to the questionnaires data from patients (n=30) diagnosed during earlier periods (1992-1996). Such a document was also sent along with mycological tests reports to physicians and personnel in charge of diagnosing infectious diseases asking for their voluntary cooperation in completing the requested information.
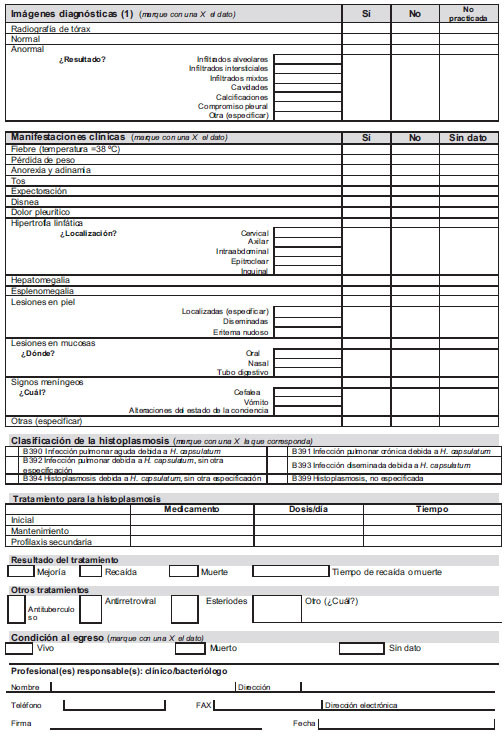
The aims of the survey were to obtain demographic data (supplement 1) from Colombian patients with the mycosis, to determine risk factors, clinical presentation, imaging data, methods by which the infection was diagnosed and antifungal treatment prescribed. Data collected from 1992 to 2008 is presented here. A preliminary report was published in 2000 (11).
Materials and methods
Data to be recorded in the questionnaire included patientâs demographics, date of diagnosis, place of birth and residence, risk factors (HIV infection, corticosteroids, autoimmune disorders, transplantation, solid tumor, hematologic malignancy, others), occupational exposure to bird excreta or bat guano, demolition work, visit to caves and soil removal activities, among others. Data on the origin of the clinical sample, the mycological tests leading to diagnosis (direct examination, cultures, immunodiffusion (ID) bands H and M, complement fixation (CF) titers were also taken into consideration (12).
Clinical findings recorded included signs and symptoms: fever, weight loss, pleuritic pain, anorexia, adynamia, vomiting, diarrhea, expectoration, meningeal symptoms, erythema nodosum, hepato-splenomegaly and adenomegalies, radiographic and hematologic abnormalities, as well as other lesions attributable to the mycoses. In HIV patients, data included CD4+ lymphocyte counts, HAART and indications on whether or not histoplasmosis had been a marker of AIDS. Finally, information on the type of antifungal treatment administered was added to the files (Supplement 1, on line version). Once completed, the questionnaires were sent to one of the coordinating institutions for their recording and analysis.
Definition of histoplasmosis was based in the presence of a compatible clinical record and in, at least, one of the following laboratory-based parameters (4):
Isolation of H. capsulatum in culture.
A positive direct examination by Wright or other histological (silver methenamine, PAS) stains.
A reactive ID test with bands M/H or both, done in the reference laboratories only (INS and CIB) (12).
A reactive CF test with a 1:32 titer with either the H antigen (histoplasmin, a fungus mycelia form filtrate) or with the Y antigen (whole yeast cells). Also done in the two reference laboratories (INS and CIB) (12).
Incidences were calculated by departments taking into account the mean number of cases in four years with the estimated 2005 population.
Data were stored in a database in Excel® (Microsoft, Redmond, WA) and processed with the statistical programs SPSS® 16.0 (SPSS Inc., Chicago, Illinois) and EPIDAT 3.1 (OPS Xunta de Galicia). A descriptive analysis of all patients included in the study was made with the quantitative data being presented as averages and standard deviation, and the qualitative data as absolute frequency and percentage. For the bivariate analysis individuals were split in 4 groups according to the information available in the questionnaire, as follows: patients with AIDS, patients with other immunosuppression, with known occupational risk and with no information available. The corresponding results were compared among themselves by means of the chi2 with the Yates correction or the Fischer exact test according to the need. The Student t test was employed to compare the continuous variables. A value of p<0.05 was considered as statistically significant. Data are presented with a p value and odds ratios with confidence intervals of 95% (13).
Ethics statement
The present study received the approval of the Ethics Committee of the CIB. Its implementation was subjected to the principles stated in the Helsinki declaration concerning medical research in human beings. Due to the descriptive character of the study and considering that the research reported was exempt of any risk to the subjects whose data were employed; their informed consent was not obtained. This is in accordance with Resolution 8430 issued in 1993 by the Ministry of Health of Colombia in charge of regulating medical research in the country. Furthermore all clinical and para-clinical procedures employed were those required by the consulting physician for the establishment of the diagnosis with no extra tests being carried. The authors did not intervene with the patients and only processed their samples as ordered by the physician in charge.
Results
Questionnaires, yearly distribution and origin
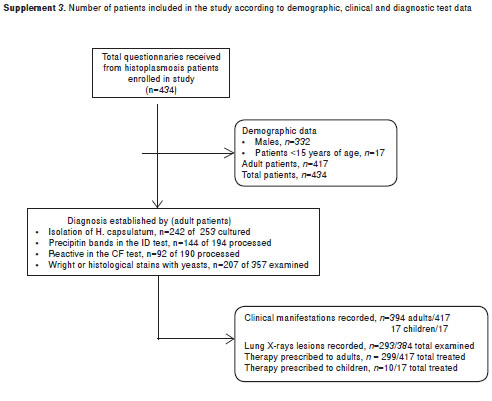
A total of 434 questionnaires from histoplasmosis patients were gathered in 16 years (1992-2008) and their distribution were as follows: 1992-1996 (n=30); 1997-2000 (n=98); 2001-2004 (n=149); 2005-2008 (n=157).
The patients originated in 20 of the 32 (62.5%) of the Colombian political divisions (Departments) and of the Capital District. In figure 1 a Colombian map is presented with the number and percentages of cases by Department with more than five cases. The other departments submitting cases were Cauca 3 (0.69%); Cesar, Chocó, Tolima and Risaralda, 2 each (0.46%). Arauca, Atlántico, Bolívar, Caquetá, Casanare, Córdoba, Huila and Sucre had one case each (0.23%).
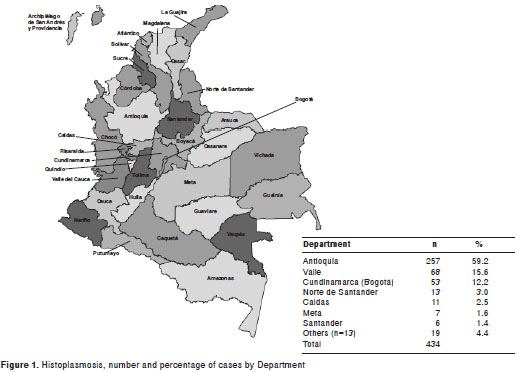
Incidences are presented in supplement 2 (http://www.revistabiomedica.org/index.php/biomedica/article/view/348) on line version. The only change observed was in Antioquia where in the period 2001-2004, the incidence was 0.317 per 100,000 habitants to increase in 2005-2008: to 0.462 per 100,000 habitants.
Demographic data
From the 434 questionnaires available, 417 (96.1%) corresponded to adult patients and the remaining 17 (3.9%) to children less than 15 years of age. supplement 3, on line version, shows patient distribution according to the various parameters taken into consideration for the study.
The characteristics of histoplasmosis in the latter population are shown in table 1. Findings of importance were the predominance of boys 11 (64.7%) and the presence of immunosuppression in 6 patients, 2 (11.8%) with AIDS and 4 (29.4%) with diverse hematologic malignancies. In 7 of the 10 (70%) patients with chest X-rays, abnormalities were recorded. In this series, the clinical presentation of histoplasmosis in 17 children indicated that 14 of them had the progressive disseminated form; only one case could take as representing the acute form of the mycosis. Data were considered insufficient in the remaining cases. The diagnostic methods rendering higher positive results were the isolation of H. capsulatum in culture and the presence of a reactive ID test, 85.7% each.
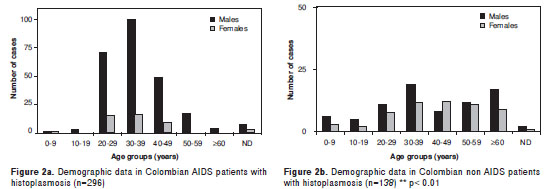
As shown in supplement 4, on line version, the 417 adult patients had a mean age of 38.4 (+12.3) years. The majority, 321 (77%) were males and the remaining 96 (23%) females. The global ratio male: female was 3:1; when occupational factors existed, the ratio was 1.5:1; if a non-AIDS immunosupression had been reported, this ratio was 1.2:1. Nonetheless, in AIDS patients such ratio was 5.5:1. When analyzing time and sex ratios in the latter group, it was found that in the period 1995-1999, it increased to 9.3:1 and between 2004-2008, it was 5.8:1 but with no significant difference (p=0.3).
Risk factors
AIDS was reported in 294/417 (70.5%) of the cases while in 29 (7.0%) there was other immunosuppressive conditions such as use of steroids in 13 (44.8%), presence of neoplasia in 7 (24.1%), transplantation in 4 (13.8%), diabetes in 2 (6.9%), cirrhosis in 1 (3.4%), alcoholism or malnourishment in 1 (3.4%) case each. In 51 (12.2%) patients an environmental factor leading to H. capsulatum exposition such as contactwithbat guano, bird excreta, cave or wheel entry, demolition work or soil removal, was indicated in the records. On this token, 23 patients had been involved in six different histoplasmosis outbreaks. In 43 (10.3%) patients the records did not reveal the presence or absence of a risk factor.
At time of diagnosis, 43 of the 294 AIDS patients (14.6%) had a mean of 66.5 (±82.1) T CD4+ lymphocytes/µl. In 81 (27.6%) antiretroviral treatment had been given. Histoplasmosis was the AIDS defining condition in 86 (29.3%) of these patients.
Demographic data, age distribution and sex-related factors in AIDS and non-AIDS patients with histoplasmosis are presented in figures 2a and 2b.
Clinical aspects
The pertaining data was recorded in 394 out of the 417 (94.5%) questionnaires received (table 2). Mean duration of symptoms before diagnosis was 3.42 (±6.5) months. In AIDS patients it was 2.68 (±3.92), in other immunosuppression states, 6.10 (±6.66), in those with occupational risk factors 5.53 (±12.22) and when no information was given, it was 4.43 (±7.18). There was a significant difference between the mean duration of symptoms, in months, before diagnosis between AIDS (2.68±3.92) and non-AIDS patients (5.3±9.27), p=0.01.

In the 394 patients referred to above, the most frequent clinical manifestation was fever recorded in 300 (76.1%) of them. Other frequent findings were cough present in 216 (54.8%) and constitutional symptoms (asthenia, adynamia, anorexia) seen in 224 (56.8%) patients. The latter were informed more regularly (178/280, 63.6%) in the AIDS group than in the remaining patients (table 2).
Diarrhea, odynophagia/dysphagia and seizures were recorded almost exclusively in AIDS patients. Hematologic abnormalities, especially anemia, were observed in the same group of patients (47.9%), as well as in those with other immunosuppresion (27.6% p<0.01). Skin lesions were recorded in 109 (38.9%) of the AIDS patients, in 5 (17.2%) in those with other immunosuppressive conditions (p=0.03) and in 2 (4.8%) of the patients with occupational risk factors (p<0.01). In 21 (5.3%) patients meningeal symptoms were recorded although H. capsulatum infection of the CNS by was demonstrated only in 9 (2.3%) of them.
All patients coinfected with HIV could be considered as progressive disseminated histoplasmosis, as well as the cases with other immunossupressive conditions. In the 51 cases classified as occupational, the data revealed disseminated histoplasmosis in 6 but the 23 patients belonging to outbreaks had the acute form clinically restricted to lungs. In those patients classified in the non-risk factor group that also included those that had had no occupational exposure (n=44), 24 (54.5%) showed only pulmonary involvement probably representing the acute form of histoplasmosis, 18 (40.9%) had more than one abnormal, fungal-colonized sites indicative of progressive disseminated histoplasmosis while in the remaining 2 cases (4.5%) the data provided was not enough to allow establishment of the clinical form.
Lung X-rays
Table 3 illustrates the radiographic data according to the risk factor. In 67 out of the 394 (22.8%) patients, the X-rays were within normal limits while in 294 (74.6%) abnormalities were revealed and represented mostly by infiltrative lesions194 (66.2 %).
Diagnostic methods
In the 417 patients included in the study, the tests employed to establish the diagnosis of histoplasmosis were not always the same and at times, more than one method was applied. The diagnosis of histoplasmosis was made by isolation in culture of H. capsulatum, microscopic observation of yeast cells using Wright or histological stains, a combination of the two or by serological tests. In the 417 adult patients, diagnosis by culturing H. capsulatum was done in 58%, by microscopic observation in 49.6% and by serological test in 14.6%. For each of the four groups analyzed, namely, AIDS, other immunosuppression, occupational and no factor declared, results of the diagnostic tests are presented in table 4.
As for the immunologic methods used, the ID test was done in 194 of the 417 cases on record proving reactive in 144 (74.2%) of them while the CF carried out in 189 cases, proved reactive en 92 (48.7%), (table 5). The ID revealed precipitin bands between 70% and 85.7% of the cases while the CF was less reactive in the various groups tested, going from 38.8% in AIDS patients to 57.1% in non-AIDS and showing 65% reactivity in those individuals having an occupational risk factor.
Treatment
From the 417 cases collected, information concerning antifungals used was recorded in 299 (52.5%). Therapy based on a single medication was given to 219 (73.2%) patients while 80 (26.7%) received combined therapy. Deoxycholate amphotericin B was used as single therapy in 106 patients and in 72 of them was followed by different maintenance medications. Itraconazole was prescribed as single therapy in 83 patients or following amphotericin B in 62 patients; it was used with other antifungals in 5 cases. Fluconazole was given in 41 cases as single therapy or in combination. Ketoconazole was prescribed in 8 instances (2.6%) while posaconazole was given as salvage therapy to 2 patients (0.7%).
Discussion
Among the endemic mycoses of the Americas the larger number of human cases reported correspond to histoplasmosis (1,3,4,14,15). Despite the fact that the larger endemic areas are those surrounding the Ohio and Mississippi River Valleys of the United States, this mycosis also occurs frequently in most Central and South American countries, Mexico (16,17), Panama (18), Venezuela (19,20) French Guyana (21), Brazil (22-26), and Argentina (27,28).
In Colombia, histoplasmosis is frequently informed in certain patient groups and, additionally, an important number of outbreaks have been reported. Nonetheless, the fact that it is not a reportable disorder hinders precise determination of its real incidence and impact on public health issues (29-33).
By means of the questionnaire adapted from the original format successfully used by the European Confederation of Medical Mycology Working Group (34), the present study represents the largest series of histoplasmosis cases informed in Colombia and Latin America and consists of 434 questionnaires filled in by physicians in charge of diagnosing and treating patients with the mycosis across the country during a 16-year period (1992-2008). Case distribution according to time of report showed a five-fold increase from 30 at start of the study to 157 patients at the end; however, this may not reflect a more frequent presentation of the mycosis in the studyâs latter period but a greater interest in the survey by the medical community.
Histoplasmosis cases were reported in 20 of the 32 (62.5%) political divisions in Colombia, including the Capital District, a finding indicative of the surveyâs ample coverage. A striking number of patients (59.2%) corresponded to residents in the Department of Antioquia. These data disagree with the percentage of histoplasmin skin test reactors (10%) reported for healthy residents of such Department in a national survey (35) and contrast with other regions informing a higher (up to 35%) histoplasmin reactivity such as in the Valle Department represented here by a low number of case reports (15.6%). All the above suggest that other factors different to environmental circumstances influence case detection, such as a higher suspicion index by physicians and the local availability of diagnostic resources, as well as increased interest in the mycosis by the medical community in the area.
Another important finding in the series was the predominance of male patients (77%) who had a mean age of 38.4 (±12.3) years, as previously reported (29-31). By grouping the cases in non-AIDS/AIDS it was noticed that in the former no differences existed by age or sex of the patients assigned to the various sub-groups, indicating that these factors play a negligible role in non-immunosuppressed patients. In the AIDS group, on the other hand, young males 20 to 39 years of age predominated with significant differences being noticed among them, females and patients in other age groups. This finding agrees with the pattern of AIDS distribution in the Colombian population (36). Such a tendency has been reported in other series as well (2,3,7,17-19,23).
The number of children and adolescents albeit low (4.1%) was indicative of the non-selective nature of histoplasmosis, a mycosis known to afflict all ages (1,2). In this series, the ratio male to female was 3:1 when no risk factor was reported although the presence of AIDS increased such ratio from 5.5:1 in the early period to 5.8:1 in the latter part of the study but with no significant differences (p=0.3).
Among the risk factors recorded for the histoplasmosis patients reported here, AIDS was the predominant condition as shown by its occurrence in 70.5% of them; additionally, the mycosis was the AIDS defining illness in 29.3% cases. As expected, the patientsâ T CD4+ mean counts were low, 66.5 (±82.1) cells/µl, as only 27.6% of them had been receiving HAART at time of diagnosis. Late diagnosis was also important as indicated by the proportion of patients (29.3%) in whom full-blown AIDS was defined by clinically apparent histoplasmosis The coincidence of HIV and histoplasmosis has been noticed in most of the series reported (6-9,16-18,21,24,26-28,29,31,37-39), but the role played by the mycosis as the AIDS defining opportunistic infection varies according to the country of report (37).
Since 1987 when progressive disseminated histoplasmosis became a marker of AIDS, it was assumed that the mycosis represented reactivation of latent foci as most patients were residents of the well-defined endemic areas of the United States, namely, the Ohio and Mississippi river valleys. Nonetheless, throughout the years it became evident that the primary infection occurs regularly in such areas (1,2,4,7,9).
Based on the data presented above and taking into consideration that histoplasmosis is endemic in certain Colombian regions (29,31,33), we believe that some of the patients could be considered as having had endogenous reactivation of a latent foci while in others, especially in those infected with the AIDS virus, histoplasmosis could well represent newly acquired infections from exposure to the fungus natural habitat.
Other immunosuppressive conditions such as steroid use, organ transplants, malnourishment, alcohol abuse, diabetes and cancer, were also recorded in small proportion of our patients (7.0%), such as reported by others (1,2,40). In 12.2% of the cases direct exposure to H. capsulatum (work with bat guano, bird excreta, exploration of caves or wells, demolition work or soil removal), was indicated in the records. All these circumstances have been reported as leading cause of fungal infection (1,2,5,32,33,41).
The pertaining clinical data were recorded in 94.5% of the questionnaires received and the corresponding analysis indicated a mean duration of symptoms before diagnosis of 3.42 (±6.0) months, this period being shorter in AIDS patients 2.68 (±3.92). A significant difference, p=0.01, was found between AIDS and non- AIDS patients, a difference already noticed in other reports and considered to be connected to the seriousness of the disease course in HIV patients (2,4,5,31,37-39). The advanced stage of the latter infection in this series explains the clinical behavior of the mycosis, as observed by the lesser age found in this group as compared with those in the other risk factor groups; it may also explain, partially at least, the observed sex differences although here a more intense environmental exposure is also attributed to males.
Besides presenting a more rapid course, the clinical course of the AIDS patients was also more aggressive and exhibited peculiar characteristics rarely informed in other patients groups, such as indicated by hematologic abnormalities and frequency and severity of skin lesions, as described earlier (2,4,5,31,37-39). It should be noticed that skin lesions are seldom observed in North American patients (8,9). Virulence and tropism of the isolates predominant in the sub-continents may explain these differences (8) although late diagnosis in Latin American countries may also explain the more extensive dissemination observed in these patients.
The lungs X-ray also revealed significant differences among the groups with the AIDS patients showing infiltrative lesions more frequently (71.6%) than patients in other groups (63.5%). This tends to indicate that in AIDS patients, lung lesions are of shorter duration than in those whose immune responses are not depressed. On the other hand, nodules were predominantly recorded (53.1%) in the non-immunosuppressed patients and only in 17.1% of the HIV population, a difference that reflects the higher immune capacity of the former resulting in delayed fungal multiplication as reflected in the formation of more solid lesions characteristic of a later stage of the mycosis. Also of importance was the number of patients (23.2%) in whom no lung radiographic abnormalities were detected, a finding that indicates that X-ray exams are not as reliable as expected. Probably other image studies, such as CAT and MRI would detect the primary lung lesions (1,2,4,5).
In this study children and adolescents with histoplasmosis were only 17 but three findings were peculiar, namely, a certain predominance of boys (64.7%), the simultaneous presence of AIDS (11.8%) and of diverse hematologic malignancies (29.4%). Here again, histoplasmosis appears as an opportunistic disorder that profits from the host immune incapacity to induce a pathologic state of considerable importance (1,2).
As it concerns serologic tests, the CF was unreliable in the AIDS population with only 48.7% of the patients proving reactive. On the other hand, the ID test revealed precipitin bands in 74.2% of the patients that were tested, a figure lower that in non-compromised patients (85.7%). Similar findings had been previously presented by Tobón et al. in a smaller series (32). Despite this promising result, a more extensive study aimed at evaluating the effectiveness on serologic tests in patients with various types of immunosuppression should be carried out. Antigen detection should be included in the new studies as they are reliable, faster and adequate diagnostic procedures in immunosupressed patients (7,42).
Exception made of fluconazole prescription for 11.4% of the cases, something that is against present recommendations patients were treated according to the current guidelines (43). However no further assessment of treatment results could be made due to the temporal nature of the survey.
This survey has important limitations because the quality of the data suffers while the larger volume of information brings forth important determinants. The fact that the questionnaires were answered voluntarily may impact on case distribution in function of the availability of diagnostic resources and of the interest and knowledge of the local physicians. Nonetheless, few studies have included a similar number of histoplasmosis cases, numbers that have allowed the establishment of valid comparisons on risk factors thus furnishing significant information concerning this fungal disorder in Colombia.
In conclusion, histoplasmosis is a frequent disease in Colombia, especially in certain risk factor groups and whose clinical manifestations and epidemiologic behavior vary according to the patient´s immunosuppression. Additional efforts should be done in order to identify and diagnose the mycosis in individuals with compatible manifestations and risk factors in order to establish an early diagnosis and treatment thus limiting the seriousness of the disease course and reducing its mortality and morbidity.
Competing Interests
The authors declare that no competing interests existed.
Funding
This work was supported by the Instituto Nacional de Salud, Bogotá, D.C, Colombia, and the Corporación para Investigaciones Biológicas (CIB), Medellín, Colombia.
Acknowledgments
We are grateful to the anonymous reviewers for their critical review of the manuscript.
The Colombian Histoplasmosis Study Group is composed of the following individuals who actively participated in the data collection (by departments): A. Vélez, A. Zuluaga, A. L. Correa, A. M. Restrepo, B. Orozco, B. Muñoz, C. Betancourt, C. Vélez, D. H. Cáceres, J. M. Anaya, E. Jaramillo, F. Díaz, G. A. Benítez, P. Cárdenas, G. A. González, G. M. Ortiz, I. C. Vélez, J. Cárdenas, J. Henao, J. Ortega, J. C. Pizano, L. Vélez, L. Franco, M. Gaviria, M. Soto, M. Gaviria, O. Uribe, P. Sierra, R. Castrillón, R. Panesso, R. Ramírez, S. Estrada, S. Jaramillo, M. I. Múnera (Antioquia); N. Villamarín, L. A. Castro, J. Galindo, J. Oñate, J. Vélez, C. Castañeda, M. Recalde (Valle);A. Motta, D. Palacios, M. Gutiérrez, A. Morales, M. Paláu, E. Ojeda, F. Alvarado, E. Morón, P. Castellar, I. Padilla, G. Rodríguez, C. Díaz, C. Sánchez, E. Rojas, C. Fajardo, D. I. Ríos, F. Arboleda, L. Sopó, L. G. Uribe, R. Monroy, E. Ospina, N. Torres, R. Vega, S. López, S. Valderrama, S. F. Ramírez, S. Páez, J. C. Díez (Bogotá D.C.,Cundinamarca); F. Berbesi, M. C. Rodríguez, J. Lizarazo (Norte de Santander); J. Pérez, M. C. Kogson (Caldas); M. Rincón, J. Suárez, R. Calderón (Santander); G. Collazos (Cauca); H. J. Ortega (Córdoba); M.I. Vargas (Meta).
Author for correspondence: Elizabeth Castañeda, Ph.D., Calle 53 No. 3-27, torre 6, apartamento 303, Bogotá, D.C., Colombia Teléfono: (571) 217 2408 ecastaneda21@gmail.com
References
1. Anstead GM, Pattersson TF. Endemic mycoses. In: Anaisse EJ, McGinnis MR, Pfaller MA, eds. Clinical Mycology. 2 edition. New York: Churchill Livingstone Elsevier; 2009. p. 355-73. [ Links ]
2. Kauffman CA. Histoplasmosis. Clin Chest Med. 2009; 30:217-25. [ Links ]
3. Couppie P, Aznarb C, Carme B, Nacher M. American histoplasmosis in developing countries with a special focus on patients with HIV: Diagnosis, treatment, and prognosis. Curr Opin Infect Dis. 2006;19:443-9. [ Links ]
4. Kauffman CA. Histoplasmosis: A clinical and laboratory update. Clin Microb Rev. 2007;20:115-32. [ Links ]
5. Hage CA, Wheat LJ, Lloyd J, Allen SD, Blue D, Knox KS. Pulmonary histoplasmosis. Semin Respir Crit Care Med. 2008;29:151-65. [ Links ]
6. Chu JH, Feudtner C, Heydon K, Walsh TJ, Zaoutis TE. Hospitalizations for endemic mycoses: A population-based national study. Clin Infect Dis. 2006;42:822-5. [ Links ]
7. Kauffman CA. Diagnosis of histoplasmosis in immunosuppressed patients. Curr Opin Infect Dis. 2008;21:421-5. [ Links ]
8. Karimi K, Wheat LJ, Conolly P, Cloud G, Hajjeh R, Wheat E, et al. Differences in histoplasmosis in patients with acquired immunodeficiency syndrome in the United States and Brazil. J Infect Dis. 2002;186:1655-60. [ Links ]
9. Hajjeh RA, Pappas PG, Henderson HD, Lancaster DM, Bamberger KJ, Skahan KJ, et al. Multicenter case-control study of risk factors for histoplasmosis in human immunodeficiency virus-infected people. Clin Infect Dis. 2001;32:1215-20. [ Links ]
10. Ashbee HR. European Committee Medical Mycology (ECMM) Newsletter, 1997. [ Links ]
11. Arango M, Bedout C, Tobón AM, Restrepo A, Torrado E, Castañeda E, et al. Histoplasmosis en Colombia: estudio interinstitucional. Inf Quinc Epidemiol Nac. 2000;5:119-23. [ Links ]
12. Chinchilla M, Kogson MC, Insignares R, Rodríguez MC, Vargas M, Torrado E, et al. Valor de las pruebas inmunológicas en el diagnóstico de las enfermedades micóticas. Biomédica. 1998;18:179-84. [ Links ]
13. Dawson B, Trapp R. Bioestadística Médica. 4° edición México DF: Editorial Manual Moderno; 2005. [ Links ]
14. Wheat LJ. Approach to the diagnosis of the endemic mycoses. Clin Chest Med. 2009;30:379-89. [ Links ]
15. Assi MA, Sandid MS, Baddour LM, Roberts GD, Walker RC. Systemic histoplasmosis: A 15-year retrospective institutional review of 111 patients. Medicine (Baltimore). 2007;86:162-9. [ Links ]
16. Reyes-Montes MR, Bobadilla-Del Valle M, Martínez-Rivera MA, Rodríguez-Arellanes G, Maravilla E, Sifuentes-Osornio J, et al.Relatedness analyses of Histoplasma capsulatum isolates from Mexican patients with AIDS-associated histoplasmosis by using histoplasmin electrophoretic profiles and randomly amplified polymorphic DNA patterns. J Clin Microbiol. 1999;37:1404-8. [ Links ]
17. Bonifaz A, Chang P, Moreno K, Fernández-Fernández V, Montes de Oca G, Araiza J, et al. Disseminated cutaneous histoplasmosis in acquired immunodeficiency syndrome: Report of 23 cases. Clin Exp Dermatol. 2009;34:481-6. [ Links ]
18. Gutiérrez ME, Canton A, Sosa N, Puga E, Talavera L. Disseminated histoplasmosis in patients with AIDS in Panamá: A review of 104 cases. Clin Infect Dis. 2005;40:1199-202. [ Links ]
19. Mata-Essayag S, Colella MT, Roselló A, de Capriles CH, Landaeta ME, de Salazar CP, et al. Histoplasmosis: A study of 158 cases in Venezuela, 2000-2005. Medicine (Baltimore). 2008;87:193-202. [ Links ]
20. Cermeño J, Cermeño J, Godoy G, Hernández I, Orellán Y, Blanco Y, et al.Epidemiological study of paracoccidioidomycosis and histoplasmosis in a suburb of San Félix City, Bolívar State, Venezuela. Invest Clin. 2009;50:213-20. [ Links ]
21. Huber F, Nacher M, Aznar C, Pierre-Demar M, El Guedj M, Vaz T, et al.AIDS-related Histoplasma capsulatum var. capsulatum infection: 25 years experience of French Guiana. AIDS. 2008;22:1047-53. [ Links ]
22. Severo LC, Oliveira FM, Irion K, Porto NS, Londero AT. Histoplasmosis in Rio Grande do Sul, Brazil: A 21-year experience. Rev Inst Med Trop Sao Paulo. 2001;43:183-7. [ Links ]
23. Rodrigues M, Ledesma C, Melo AM, Ledesma D, Venâncio R, Wanke B. Study of 30 cases of histoplasmosis observed in Mato Grosso do Sul Stae, Brazil. Rev Inst Med Trop Sao Paulo. 2007;49:37-9. [ Links ]
24. Mora DJ, dos Santos CT, Silva-Vergara ML. Disseminated histoplasmosis in acquired immunodeficiency syndrome patients in Uberaba, MG, Brazil. Mycoses. 2008;51:136-40. [ Links ]
25. Goldman LZ, Aquino VR, Lunardi LW, Cunha VS, Santos RP. Two specific strains of Histoplasma capsulatum causing mucocutaneous manifestations of histoplasmosis: Preliminary analysis of a frequent manifestation of histoplasmosis in southern Brazil. Mycopathologia. 2009;167:181-6. [ Links ]
26. Prado M, Silva MB, Laurenti R, Travassos LR, Taborda CP. Mortality due to systemic mycoses as a primary cause of death or in association with AIDS in Brazil: A review from 1996 to 2006. Mem Inst Oswaldo Cruz. 2009;104:513-21. [ Links ]
27. Negroni R, Taborda A, Robles AM, Arechevala A. Itraconazole in the treatment of histoplasmosis associated with AIDS. Mycoses. 1992;35:281-7. [ Links ]
28. Pietrobon D, Negro-Marquinez L, Kilstein J, Galíndez J, Greca A, Battagliotti C. Disseminated histoplasmosis and AIDS in an Argentine hospital: Clinical manifestations, diagnosis and treatment. Enferm Infecc Microbiol Clin. 2004;22:156-9. [ Links ]
29. Arango M, Cano LE, De Bedout C, Estrada S, Gómez I, Restrepo A, et al.Histoplasmosis y criptococosis diseminadas en pacientes con el síndrome de inmunodeficiencia adquirida (SIDA). Acta Med Colomb. 1990;15:84-91. [ Links ]
30. Tobón A, Franco L, Correa AL, Bedoya F, Ortega J, Soto M. et al.La Histoplasmosis en el adulto, pasos para su diagnóstico. Acta Med Colomb. 1997;22:277-84. [ Links ]
31. Tobón AM, Agudelo CA, Rosero DS, Ochoa JE, De Bedout C, Zuluaga A, et al.Disseminated histoplasmosis: A comparative study between patients with acquired immunodeficiency syndrome and non-human immunodeficiency virus-infected individuals. Am J Trop Med Hyg. 2005;73:576-82. [ Links ]
32. Ordoñéz N, Tobón A, Arango M, Tabares A, De Bedout C, Gómez B, et al. Brotes de histoplasmosis registrados en el área andina colombiana. Biomédica. 1997;17:105-11. [ Links ]
33. Jiménez R, Urán M, De Bedout C, Arango M, Tobón AM, Cano LE, et al. Brote de histoplasmosis aguda en un grupo familiar: identificación de la fuente de infección. Biomédica. 2002;22:155-9. [ Links ]
34. Ashbee HR, Evans EG, Viviani MA, Dupont B, Chryssanthou E, Surmont I, et al.Histoplasmosis in Europe: Report on an epidemiological survey from the European Confederation of Medical Mycology Working Group. Med Mycol. 2008;46:57-65. [ Links ]
35. Carmona J. Análisis estadístico y ecológico-epidemiológico de la sensibilidad a la histoplasmina en Colombia 1950-1968. Antioquia Med. 1971;21:109-54. [ Links ]
36. Ministerio de la Protección Social, Instituto Nacional de Salud. Manual de Referencia. Observatorio Nacional de la Gestión en VIH-SIDA. 2006. Fecha de consulta: 7 de abril de 2011. Disponible en: http://www.minproteccionsocial.gov.co/salud/Documents/INS.pdf [ Links ]
37. Baddley JW, Sankara IR, Rodriquez JM, Pappas PG, Many WJ Jr. Histoplasmosis in HIV-infected patients in a southern regional medical center: Poor prognosis in the era of highly active antiretroviral therapy. Diagn Microbiol Infect Dis. 2008;62:151-6. [ Links ]
38. Ferreira MS, Borges AS. Histoplasmosis. Rev Soc Bras Med Trop. 2009;42:192-8. [ Links ]
39. McKinsey DS, Spiegel RA, Hutwagner L, Stanford J, Driks MR, Brewer J, et al. Prospective study of histoplasmosis in patients infected with human immunodeficiency virus: Incidence, risk factors, and pathophysiology. Clin Infect Dis. 1997;24:1195-203. [ Links ]
40. Cuellar-Rodríguez J, Avery RK, Lard M, Budev M, Gordon SM, Shrestha NK, et al.Histoplasmosis in solid organ transplant recipients: 10 years of experience at a large transplant center in an endemic area. Clin Infect Dis. 2009;49:710-6. [ Links ]
41. CDC. Histoplasmosis: Protecting workers at risk. Revised edition. Cincinnati, OH: US Department of Health and Human Services, CDC, National Institute for Occupational Safety and Health (2004). Fecha de consulta: 12 de agosto de 2009. Disponible en: http://www.cdc.gov/niosh/docs/2005-109. [ Links ]
42. Scheel CM, Samayoa B, Herrera A, Lindsley MD, Benjamin L, Reed Y, et al. Development and evaluation of an enzyme-linked immunosorbent assay to detect Histoplasma capsulatum antigenuria in immunocompromised patients. Clin Vaccine Immunol. 2009;16:852-8. [ Links ]
43. Wheat LJ, Freifeld AG, Kleiman MB, Baddley JW, McKinsey DS, Loyd JE, et al.Clinical practiceguidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis.2007;45:807-25. [ Links ]