INTRODUCTION
In Brazil, Ageratumfastigiatum (Gardner) R.M. King & H. Rob. (Eupatorieae, Asteraceae) has the popular names of enxota and mata-pasto. The aerial parts of the plant are employed in folk medicine, in the form of preparations for topical use to treat pain and inflammation [1-3].
Previous studies have shown the analgesic and anti-inflammatory activities of the essential oil and ethanolic extract of A. fastigiatum branches, confirming the properties observed in folk medicine [1, 4-6]. The chemical analysis of the essential oil identified the presence of mono- and sesquiterpenes, such as a-pinene, limonene, (3-caryophyllene, germacrene D, a-humulene and others [1, 3, 4, 6, 7]. The phytochemical screening of the ethanolic extract indicated the presence of secondary metabolite classes, e.g., flavonoids, tannins, coumarins, terpenes, sterols and saponins [5], and the coumarin ayapine was identified [3]. In less polar extracts, steroids and triterpenes were found, e.g., stigmasterol, campesterol, lupeol and a- and (3-amyrin. Labdane-type diterpenes, eudesmane-type sesquiterpenes and a daucanolide sesquiterpene lactone were also found [3, 8, 9].
Despite the medicinal importance of the plant and the studies conducted to date, research on the toxicity of extracts of A. fastigiatum are still lacking. Thus, the aim of this study was to perform an initial evaluation of the toxicity of an ethanolic extract of the aerial parts of A. fastigiatum, as well as its phytochemical screening.
METHODOLOGY
Collection and identification of plant materials
Leaves, flowers and branches (the aerial parts) of A. fastigiatum were collected for the preparation of the extract. The collection was carried out on October 19, 2014, at 9:00 a.m. with dry weather at the JK Campus of the Federal University of the Jequitinhonha and Mucuri River Valleys (UFVJM), in Diamantina, State of Minas Gerais, Brazil, in an area of mixed vegetation with montane meadows and open grassland (18°12,255' S, 43°14.243' W). The plant material was identified with voucher no. 1300 (determiner F.N. Costa), which was deposited at the Diam herbarium (UFVJM).
Preparation and fractionation of the raw extract
The aerial parts of the plant were dried in a laboratory oven with circulating hot air (Biopar®) at 35°C-40°C, until a constant weight was obtained. The material was pulverised in a knife mill (SL32-Solab®) and the resulting powder (750 g) was subjected to extraction by exhaustive maceration in ethanol PA, in a proportion of 1/10 w/v (powder/solvent). The crude extract was concentrated in a rotary evaporator (Fisatom® 801) at 40-42 °C under low pressure. The dry extract (236 g; yield, 36.4%) was kept in a vacuum dryer at room temperature.
The ethanolic extract (80 g) was resuspended in a methanol:water (3:1) solution and fractionated through liquid-liquid partition using immiscible solvents (hexane followed by dichloromethane), to obtain the hexane, dichloromethane and hydroalco-holic phases (or fractions). The hexane and dichloromethane phases were concentrated in a rotary evaporator and stored at room temperature, with yields of 4.7% and 6.2%, respectively. The hydroalcoholic phase was subjected to a vacuum rotary evaporation process (35-40 °C), followed by lyophilisation (Liotop® L101 lyophilizer), and was stored at -20 °C, with a yield of 29.2%.
Phytochemical screening
An analysis of the main groups of secondary metabolites (alkaloids, anthracenosides, cumarins, steroids, flavonoids, saponins, tannins, triterpenes) was conducted on the products obtained from the fractionation of the ethanolic extract. The phytochemical screening included chromogenic and precipitation reactions, as well as TLC (thin layer chromatography) analysis [10, 11].
The reactions for phytochemical screening are carried out with samples diluted in test tubes (the hydroalcoholic fraction is diluted in water or in a hydroalcoholic mixture and the organic fractions are diluted in appropriate organic solvents) and the reagents are applied directly on this material. Mayer, Dragendorff and Bertrand reagents were used for the detection of alkaloids; precipitate formation indicates a positive result. Anthracenosides are investigated through the Borntráger Reaction; the reaction is positive when there is red color development due to the formation of anthracenoside genine salts. Coumarins can be detected by TLC; the revealing agent used is the KOH 0.5M (aqueous solution) and the exposure of the chromatographic plate to UV light 254 nm; the observation of green or bluish fluorescence spots is indicative of the presence of these metabolites. The Liebermann-Burchard reagent is used to detect steroids and triterpenes; with the formation of green or bluish coloration it is indicative of the presence of steroids and the development of brown or reddish coloration is positive for triterpenes.
For the detection of flavonoids, the Shinoda reaction is used; with the formation of a reddish color, it is positive for the presence of flavonoids in the analyzed material. The afrogenic test is used to detect saponins; this test consists of shaking the test tube containing the material diluted in water for 15 seconds, thus, if there are saponins, persistent foam will form for more than 15 minutes. A FeCl3 2 % (aqueous solution) can detect condensed tannins by developing a green color and can detect hydrolyzable tannins due to the formation of a bluish color; the confirmation of the presence of tannins is done with a gelatin 2.5 % (aqueous solution), if there are tannins there is the precipitation of the tannin-protein complex.
GC-MS analysis
GC-MS analysis of hexane and dichloromethane phases were performed on a chromatograph Shimadzu® GC-MS-QP2010 gas chromatography-mass spectrometer equipped with capillary column RTx-5ms (Restek Co. Bellefonte, PA, USA), (30 m x 0.25 mm, film thickness 0.25 fim) under the following conditions: Helium was used as the carrier gas with linear velocity of 43.2 cm/s; at pressure of 86.7 kPa; the injection was made in split mode (1:5), with injector temperature at 260 °C; the initial analysis temperature was 60 °C, increasing 4 °C/min and remaining at 320 °C for 25 minutes. The mass spectrometer was operated in an electronic ionization mode at 70 eV with m/z scan at 35 to 600 Da. The interface was maintained at 320 °C and an ion source at 250 °C. The components of the samples were measured based on the relative area of the peaks (%). The task of identifying the chemical constituents of the samples was performed by analysing the mass spectra obtained experimentally and comparing them with the spectra from the NIST11, WILEY7 and FFNSC 1.3 mass spectral libraries. To aid in the identification, the relative retention index (RRI) was calculated by applying the classic Van den Dool-Kratz equation [12]; for this calculation, a chromatogram (Alltech®) with a homologous series of linear chain aliphatic hydrocarbons (C9-C40) was obtained under the same chromatographic conditions that were used in the analysis of the hexane and dichloromethane phases.
Cytotoxic assay
The mouse fibroblast (L929) was obtained from American Type Culture Collection (ATCC, LGC Promochem®, Rockville, MD, USA). L929 were cultured in Roswell Park Memorial Institute 1640 medium (RPMI1640) supplemented with 10 % heat-inactivated fetal bovine serum (FBS) (Gibco® Invitrogen Corp., Grand Island, NY, USA) and antibiotics (100 mg/mL of streptomycin and 100 unit/ml of G penicillin, Sigma®, St. Louis, USA) at cells were harvested at 37 °C in a balanced air humidified incubator with an atmosphere of 5 % CO2. Cells were maintained in exponential growth phase and submitted periodical peal after treatment with trypsin-EDTA (Sigma®, St. Louis, USA) treatment. Cell viability was determined by 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) dye reduction assay [13]. The cell line was exponentially grown and 1x105 cells/well plated at in 96-well flat-bottom plates and allowed to adhere for 24 h. The crude extracts of Ageratum fastigiatum were tested in the concentrations range to 1000 a 7.8 µg/mL and after their addition, cells were incubated for 72 hours. The cadmium chloride (Próquimios®, 0.2 M) was used as positive controls. Cells without a test compound were used as a viability control and only the medium served as the blank. MTT dye solution was added (0.5 mg/mL) and after 4 h of incubation, medium was removed and 100 µL of DMSO was added to solubilize the reduced formazan deposit. After shaking for 10 min, the optical density (OD) value was measured on a spectrophotometer at wave length of 540 nm (Molecular Devices, Sunnyvale, California, USA). The relative growth rate (RGR) was calculated to evaluate the cytotoxicity of extracts. Inhibitory concentration 50 (IC50) was determined by the method of logarithmic regression analysis of data obtained GraphPad Prism (GraphPad Software®, San Diego California USA). All analysis was performed in triplicate, and the average data were reported as the results.
Assay standardisation, obtaining Artemia salina and toxicity test
The bioassay that was used to verify the toxicity of the extract in the microcrustacean Artemia salina Leach (Artemiidae) was obtained from the literature [14] and was standardised in our laboratory by testing the optimal water temperature (26-30 °C), pH (7-9), aeration intensity (low or medium), luminosity (24 h of constant light or a 12 h illumination cycle) and concentration of sea salt (15-30 g/L). The determination of the optimal parameters was performed using a magnifying glass, to verify the motility of the A. salina subjects 24 h after the cysts hatched. To obtain A. salina larvae (nauplii) for the toxicity test, the cysts were incubated until hatching in the following conditions: artificially salted water (15 g/L), pH adjusted to 8, moderate aeration and constant agitation at 28-29 °C for 48 h and constant luminosity. The toxicity test was carried out in triplicate under the same conditions as those used to obtain nauplii. For each replication of the experiment, 60 test tubes were used, each containing 10 mL of artificially salted water and 10 nauplii. The tubes were then divided into five groups, which received different treatments: (I) negative control, containing saltwater and 5 % Tween 80; (II) positive toxicity control, containing K2Cr2O7 at 0.1 %; (Ill) test groups with different concentrations (1, 5 and 10 mg/mL) of the ethanolic extract and of the dichloromethane, hexane and hydroal-coholic phases, all dissolved in saltwater containing 5 % Tween 80. No nauplii died at concentrations below 1 mg/mL; therefore, the tested concentrations were all >1 mg/mL. Nauplius mortality was measured after 24 h of incubation. The percentage of mortality was calculated and LC50 values (lethal concentration for 50 % of nauplii) were calculated by linear regression (sample concentration versus % of viable nauplii). Statistical treatment was performed using an analysis of variance (Anova one-way) followed by Tukey's test (Graph Pad Prism 8.0).
RESULTS AND DISCUSSION
The phytochemical screening indicated the presence of coumarins, triterpenes and steroids in all three phases obtained from the ethanolic extract. In the hydroalcoholic phase, hydrolysable tannins, saponins and alkaloids were also detected. Coumarins, terpenoids, steroids and saponins have also been reported in A. fastigiatum extracts [3, 5, 8, 15].
The list of the constituents of the hexane and dichloromethane phases identified by GC-MS can be found in table 1. In the hexane phase, 54 constituents were detected, whereas the dichloromethane phase contained 23 constituents, not all of which could be identified. Because of the chemical characteristics of the hydroalcoholic fraction, it was not analysed by GC-MS.
Table 1 Compounds identified by gas chromatography coupled to mass spectrometry and present in the hexane and dichloromethane phases obtained by partition of the ethanolic extract of Ageratum fastigiatum aerial parts.
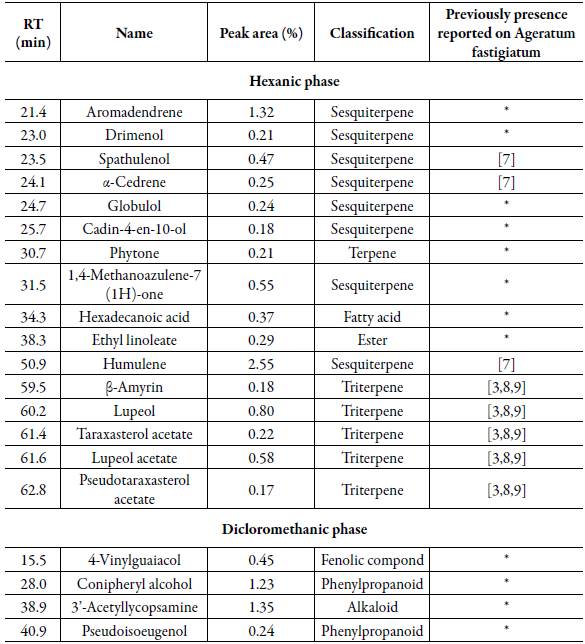
RT: retention time; * Not previously reported.
An alkaloid was detected in the GC-MS analysis of the dichloromethane phase. However, the class of alkaloids was not identified in the phytochemical screening; this can be explained by the fact that the typical reactions (Dragendorff, Mayer, Bertrand) used for the detection of this class of compounds are more sensitive to alkaloids in the form of salts. In the dichloromethane phase, alkaloids should be predominantly in the free-base form. In addition, the concentration of alkaloids in the dichloromethane phase may have been being the detection threshold of the usual screening. However, as GC-MS is more sensitive than the classical screening, the presence of 3'-acetyl lycopsamine was suggested. Pyrrolizidine alkaloids occur in the tribe Eupatorieae, especially in the genus Ageratum, and have been reported mainly in Ageratum conyzoides L. [16, 17]. Coumarins and phenylpropanoid derivatives are also common in the tribe Eupatorieae [17].
Some constituents identified in the ethanolic extract of A. fastigiatum, e.g., coumarins, terpenoids, steroids and saponins, exhibit anti-inflammatory and analgesic activity [18]. More specifically, the following constituents identified here have anti-inflammatory activity: ethyl linoleate, palmitic acid (hexadecanoic acid), humulene, lupeol, lupeol acetate, 4-vinyl guaiacol and coniferyl alcohol [19-25]. Thus, these constituents may contribute to the therapeutic activity that has been reported for this plant in folk medicine.
Pyrrolizidine alkaloids are hepatotropic and are potentially toxic to humans [26]. Therefore, there are risks in the use of medicinal plants containing these alkaloids, especially if the medicinal preparation is taken by mouth. However, reports of the medicinal use of A. fastigiatum indicate only topical administration.
Artemia salina has been used to verify the toxicity of plant extracts [27]. The results of the percentage of mortality of A. salina nauplii treated with the ethanolic extract from A. fastigiatum and its fractions at different concentrations are presented in table 2. The crude ethanolic extract was the least toxic of all treatments, yielding low mortality at the highest tested concentration (10 mg/mL) and an activity that was comparable to that of the negative control at the lowest tested concentration (1 mg/mL). The dichloromethane phase was the most toxic, causing 100 % nauplius mortality at a concentration of 10 mg/mL. The hexane and hydroalcoholic phases caused significant mortality of microcrustacean larvae at medium (5 mg/mL) and high (10 mg/mL) concentrations.
Table 2 Percentage (±SEM) of mortality of Artemia salina larvae (nauplii) caused by the ethanolic extract of Ageratumfastigiatum aerial parts and by its hexane, dichloromethane and hydroalcoholic fractions in different concentrations and LC50.
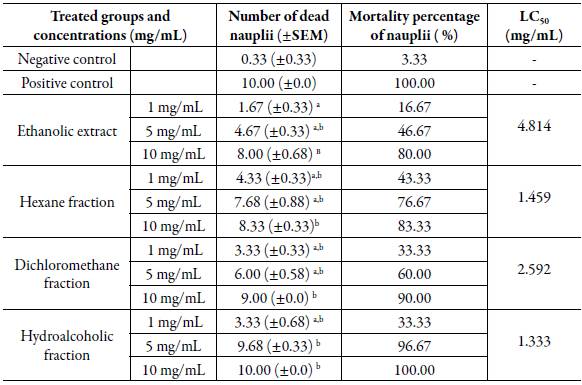
N: 10 in each test; tests performed in triplicate. a significant difference of the treated group in relation to the positive control (K2Cr2O7 at 0.1 %); bsignificant difference of the treated group in relation to the negative control (saltwater and 5 % Tween 80); significant difference p <0.05 (one-way Anova; Tukey Test).
The calculated LC50 values indicated that the ethanolic extract had lower toxicity compared with the other treatments (LC50, 4.814 mg/mL). The hexane and dichloromethane phases exhibited LC50 values of 1.459 and 2.592 mg/mL, respectively. The hydroalcoholic phase was the most toxic, with an LC50 value of 1.333 mg/mL. The fractions showed higher toxicity than did the crude extract, probably because the toxic substances were more diluted in the extract compared with the fractions. Meyer et al. [14] established a relationship between the degree of toxicity and the LC50 of plant extracts in A. salina larvae. Thus, extracts with LC50 values >1 mg/mL are considered non-toxic. This was the case with the analyses performed using A. fastigiatum. It is possible that the chemical constituents present in the extract and in its phases exhibited low toxicity to nauplii because of the complexity of the interactions between the different molecules present or their low concentration in the extract or phases, or because of the crustacean's resistance to certain substances at the concentrations at which they were present.
The crude ethanolic extract of the aerial parts of A. fastigiatum and its fractions showed varying degrees of toxicity in L929 cells. The crude ethanolic extract promoted cell death at a rate ranging from 92.42 % to 32.33 %, with a toxic concentration range of 1000-15.62 µg/mL and an LC50 value of 62.92 µg/mL for the L929 cell line (table 3). The hexane fraction was significantly toxic at concentrations ranging from 1000 to 7.81 µg/mL, with the percentage of cell death ranging from 93.84 % to 33.34 % and an LC50 value of 36.69 µg/mL. The hydroalcoholic fraction yielded a percentage of cell death ranging from 55.67 % to 19.38 %, with the cytotoxic concentration ranging from 1000 to 125 µg/mL and an LC50 value of 174.2 µg/mL. Finally, the dichloromethane fraction also showed toxicity in L929 cells at all concentrations tested (10007.81 µg/mL), with the cell death percentage ranging from 95.48 % to 47.15 % and an LC50 value of 11.39 µg/mL, thus being the fraction that reduced cell viability the most.
Table 3 Cytotoxicity evaluation (active concentration range, cell death percentage and LC50) of crude ethanolic extract and fractions of Ageratum fastigiatum aerial on L929 cells.
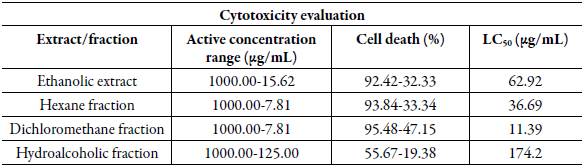
Active concentration range, there are significant differences at p <0.05, 95 % confidence interval compared to respective negative controls or viability; Reduction of cell viability observed for the highest and lowest active concentration of the extract; LC50: Concentration that inhibits 50 % of cells. The results present the evaluation of three independent experiments performed in triplicate.
According to Rajabi et al. [28], tests performed using MTT in L929 fibroblast cells and bioassays using the A. salina microcrustacean are comparable. Thus, at the concentrations evaluated and with the standard methodologies used, the extract and its fractions were not highly toxic to the microcrustacean, but a higher toxicity to the fibroblast culture could be noted. Differences in toxicity in different cells and organisms may occur, as toxicity may be related to the types of substances present in the extracts and the types of receptors present in isolated cells or in an organism. Moreover, a pluricellular organism has a more complex biochemistry and compartmentalisation (into systems) than do isolated cells. Other toxicity studies using extracts of A. fastigiatum, especially those performed using mammals and different experimental models, should be conducted to assess this issue better.
It is known for a fact that toxicity of the extract and its fractions, however low, occurs due to the presence of several metabolites, and it is not possible to attribute the effect to a single metabolite or class of metabolite of A. fastigiatum. It is likely that a combination of different metabolites is responsible for the activity of an extract or its fractions. The toxicity observed in the assays does not occur solely because of the presence of hepatotoxic alkaloids. The extract and fractions are phyto-complexes; therefore, several constituents contribute to the biological activity (therapeutic or toxic) of these plant products.
Toxicity studies conducted using two different experimental models detected the cytotoxicity of products from this plant species. Thus, the presence of pyrolizidine alkaloids and the detected cytotoxicity are important data to guide future research on medicinal preparations of this plant that are already used empirically by the population, as well as to re-evaluate the studies of this plant that were aimed at producing phytotherapeutic preparations from its extract and, of course, to guide a more cautious or controlled folk use of medicinal A. fastigiatum preparations. However, toxicological studies using other experimental models, both in vitro and in vivo, should be conducted to determine the toxicity of this medicinal plant and guide the population regarding the safety of its use.














