Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista Colombiana de Obstetricia y Ginecología
versão impressa ISSN 0034-7434
Rev Colomb Obstet Ginecol vol.65 no.1 Bogotá jan./mar. 2014
https://doi.org/10.18597/rcog.77
DOI: http://dx.doi.org/10.18597/rcog.77
Edith Ángel-Müller, MD1; Jorge Andrés Rubio-Romero, MD, MSc2; Andrea Rodríguez-Hernández, MD, MSc3; Ariel Ruiz-Parra, MD, MSc4
Recibido: enero 23/14 - Aceptado: marzo 25/14
1Associate professor Department of Obstetrics and Gynecology, Universidad Nacional de Colombia. Bogotá, Colombia. eangelm@unal.edu.co
2Associate professor, Department of Obstetrics and Gynecology, Clinical Research Institute, Universidad Nacional de Colombia. Bogotá, Colombia.
3Investigator, Clinical Research Institute, Universidad Nacional de Colombia. Bogotá, Colombia.
4Titular professor, Department of Obstetrics and Gynecology, Clinical Research Institute, Universidad Nacional de Colombia. Bogotá, Colombia.
ABSTRACT
Objectives: To describe the safety and the clinical and microbiological efficacy of a single oral dose of a combined treatment with secnidazole plus fluconazole for the syndromic management of symptomatic vaginal discharge.
Materials and methods: A clinical trial without control group study was conducted including women with symptomatic vaginal discharge who assisted to a secondary level hospital in Bogota, Colombia. 118 women were included in a consecutive convenience sample who received the study treatment according to syndromic diagnosis approach. Microbiological diagnosis of bacterial vaginosis (BV) was confirmed by Nugent score, yeast infection by candida culture and trichomoniasis by wet mount. Prevalence, clinical and microbioogical efficacy and safety of the secnidazole and fluconazole combination pill was determined and a sensitivity analysis for treatment efficacy was performed.
Results: The following infections were found: BV in 57.1%, candidiasis in 28.8%, and mixed infections in 10.8%. In 8.5% of the patients, the microbiology tests were negative. No trichomonas were found. The clinical cure rate was 90.4%, and the microbiological cure rate was 94.1% with the study medication. Twelve cases (12.90%) presented drug-related non serious adverse events.
Conclusion: The most prevalent infection was BV, followed by candidiasis and mixed infection. The combination of a single dose of secnidazole plus fluconazole combined pill had an efficacy rate over 90% and was safe for the treatment of symptomatic women with vaginal discharge.
Key words: Vaginosis, bacterial, candidiasis, vulvovaginal, vaginal discharge, therapeutics, secnidazole, fluconazole.
RESUMEN
Objetivos: describir la seguridad y la eficacia clínica y microbiológica del tratamiento combinado de secnidazol mas fluconazol oral, dosis única, para el manejo del flujo vaginal sintomático.
Materiales y métodos: ensayo clínico sin grupo control, realizado en mujeres sintomáticas con flujo vaginal en un hospital de mediana complejidad localizado en la ciudad de Bogotá, Colombia. Se incluyeron 118 mujeres por muestreo consecutivo por conveniencia quienes recibieron el tratamiento de acuerdo con el diagnóstico sindrómico. El diagnóstico microbiológico se estableció usando el puntaje de Nugent para vaginosis bacteriana (VB), el cultivo para cándida y el frotis directo en fresco para tricomonas. Se estimaron la prevalencia, la efectividad clínica y microbiológica, y la seguridad del tratamiento combinado de secnidazol con fluconazol en mono dosis, y se realizó un análisis de sensibilidad para la eficacia del tratamiento.
Resultados: la prevalencia de VB fue del 57,1%, de candidiasis fue del 28,8% y de la infección mixta 10,8%. No se encontró infección por tricomonas. En 8,5% de las pacientes los resultados microbiológicos fueron negativos. La tasa de curación clínica con secnidazol más fluconazol fue de 90,4%, y la tasa de curación microbiológica fue de 94,1%. Doce pacientes (12,90%) presentaron eventos adversos no serios relacionados con el medicamento.
Conclusión: la VB fue la infección más común en este estudio, seguida por la candidiasis y las infecciones mixtas. La combinación secnidazol más fluconazol es una intervención efectiva para alcanzar la cura clínica y microbiológica en las pacientes con síndrome de flujo vaginal, con una baja frecuencia de eventos adversos no serios.
Palabras clave: vaginosis bacteriana, candidiasis vulvovaginal, síndrome de flujo vaginal, tratamiento, secnidazol, fluconazol.
INTRODUCTION
Genital tract infections (GTIs) have increased in the past decade and there is an association between sexually transmitted infections (STIs) and HIV transmission (1). It has also been suggested that other GTIs, such as bacterial vaginosis (BV) (2) and trichomoniasis (3) are associated with HIV transmission.
In an effort to reduce the transmission of GTIs, the World Health Organization (WHO) proposed a syndromic diagnostic approach as a low cost alternative in places with no access to laboratory diagnostic tests (4, 5). This approach was initially applied in sub-Saharan Africa and was particularly effective in men and women with genital ulcers. However, its effectiveness has been controversial in certain situations (e. g., when the prevalence of causative agents is low or unknown, for asymptomatic sexually transmitted infections (STIs), and for women with vaginal discharge, for whom the syndromic approach can lead to overdiagnosis and unnecessary treatments (6)
Under the syndromic approach, an effective treatment against Candida albicans, Trichomonas vaginalis, and bacterial vaginosis is advised in patients with vaginal discharge syndrome (7). In fact, there are mixed infections in 23.2% of women with symptoms of vaginal discharge or pruritus (8). Metronidazole plus clotrimazole has been recommended as a first-line treatment, but there are other alternatives, such as fluconazole or itraconazole for the management of candidiasis (9) and secnidazole for the treatment of BV (10). Therefore, for syndromic management of vaginal discharge the combination of fluconazole and secnidazole could be used, but there were no studies evaluating this combination in the literature reviewed.
The objectives of this study were to describe the clinical and microbiological cure rate and safety of the combination of oral single dose secnidazole plus fluconazole treatment of vaginal discharge according to the syndromic diagnostic approach.
MATERIALS AND METHODS
A clinical trial without control group was carried out in order to describe the efficacy and safety of a single dose of an oral combination medication with 2 g secnidazole and 150 mg fluconazole in women with symptomatic vaginal discharge syndrome was performed. The study was conducted in the outpatient service of a public, medium level of complexity hospital in Bogota, Colombia. The participants were sexually active women with lower genital tract symptoms (leukorrhea, itching, burning, pain, foul-smelling vaginal discharge, or urethral symptoms) compatible with symptomatic vaginal discharge syndrome. Patients with a clinical diagnosis of cervicitis, severe medical conditions, liver disease, allergies, or known reactions to the drugs under study, pregnant women or breastfeeding, women who had previously participated in the study and women who had received antibiotic therapy in the previous 14 days were excluded. A consecutive convenience sample size of 100 symptomatic patients was initially calculated. An anticipated 20% rate of lost to follow-up patients was considered.
Procedures. Patients were invited to participate by a trained nurse. After signing the consent form, the subjects underwent a clinical examination. Vaginal samples were taken for wet mount microscopy, lateral vaginal wall smear was taken for Gram stain and Candida culture. The clinical diagnosis was made based on clinical examination. A blood count was performed, and transaminases were measured. Subsequently, treatment was provided under the supervision of the researchers. The subjects returned for a follow-up visit in the next three weeks, and a second return visit took place between 4 to 6 weeks after the initial visit. At the first follow-up visit, clinical cure, defined as a remission of signs or symptoms of the vaginal discharge, was assessed, and samples were taken to evaluate microbiological cure. The participants who did not attend the follow-up control visit were contacted by telephone to estimate clinical cure. The presence of adverse effects was determined using a survey, a follow-up blood count and the measurement of blood transaminases. At the second follow-up control clinical cure was evaluated. For cases of vaginitis caused by Trichomonas vaginalis treatment for the sexual partner was planned. The patients who had infections at the first post-treatment control visit were treated according to the recommended regimens (7).
Laboratory Tests. The amine test was performed with 10% KOH, and the vaginal pH was measured with litmus paper. Gram staining was performed, and BV was diagnosed by a trained bacteriologist using the Nugent criteria, when a score of 7 or more was found (11). A wet mount was performed to identify Trichomonas vaginalis. Sabouraud medium and blood agar were used to isolate yeast, and chrome agar was used to identify Candida albicans. Transaminases were measured using ALT and AST Cobas® processed in a Roche/Hitachi automated analyzer according to the manufacturer’s instructions. The blood counts were processed on a Roche XT-1800i automated hematology analyzer.
Variables.The following variables were evaluated: demographic variables, life style habits such as smoking and the use of contraception, anthropometric data, and gynecological examination symptoms and signs. The outcome variables included the prevalence rates of VB, vaginal candidiasis and trichomoniasis, the efficacy of treatment in terms of clinical cure and microbiological cure rates, and the cure rate for each etiological group. The frequency of adverse treatment effects was estimated; a significant elevation in transaminases, defined as a 50% increase in the blood transaminases, leukopenia or thrombocytopenia after receiving the study treatment were considered adverse effects.
The statistical analysis was performed with STATA 11.0 software (College Station, Texas, USA). Simple and relative frequencies and measures of central tendency and dispersion appropriate for the distribution of the variables were calculated. A sensitivity analysis was performed on the treatment efficacy results, taking the follow-up losses into consideration.
Ethical considerations. All women signed a written informed consent form agreeing to participate voluntarily in the study. The study was approved by the Ethics Committee of the Faculty of Medicine of the National University of Colombia and by the Research Committee (Institutional Review Board) of the Engativá Hospital. The protocol was registered at ClinicalTrialsFeeds.org under the ID number 309010018168.
RESULTS
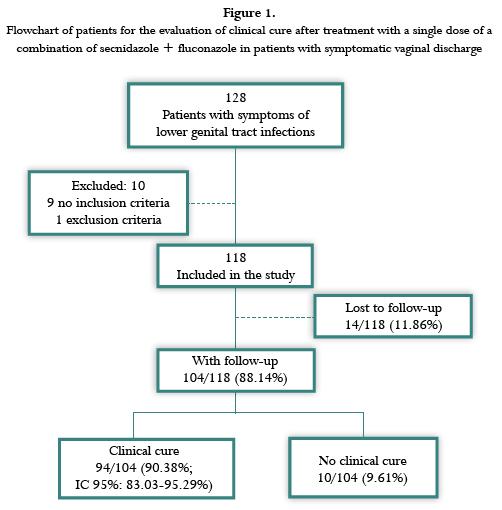
Between September 1, 2012 and February 15, 2013, 128 women with symptoms of lower genital tract infections were evaluated. Nine of these women did not meet the inclusion criteria and one was excluded because she was breast-feeding. A total of 118 women were included (figure 1).
The demographic characteristics of the patients are shown in table 1. The median age was 31 years; the mean of BMI was 24.28 kg/m2 and the median of previous pregnancies was 2.0. Fifty-nine patients (50%) reported previous episodes of genital infections.

The most frequent symptom was vaginal discharge (96.6%) followed by foul smell (57.6%) and pruritus (54.2%). The median duration of symptoms was two months (range, two days to 12 months). Vaginal discharge was present in all patients on genital examination. Other signs founded were foul smell (70.3%), erythema (47.5%) and edema (40.7%). None of the patients had genital ulcers. The amine test was positive in 48 patients (40.68%), and pH values > 5 were observed in 93 patients (88.8%).
There was a unique infection in 96 patients and mix infection in 12. The bacterial vaginosis was diagnosed by the Nugent score, in 62 (57.11%) patients, there were 46 positive cultures for Candida, of which 30 (65.22%) were Candida albicans, and 16 (34.78%) were other species of Candida. None of the patients had tricomoniasis. Table 2 shows the microbiological laboratory results.
The follow-up evaluation was conducted with a total of 104 women (At the office in 93 women and via telephone in 11 women) (figure 1). A total of 94/104 (90.38%) patients who participated in a follow-up visit, showed clinical cure.
The microbiological analyses corresponding to the index consultation were positive in 108 of 118 patients (91.53%) patients. In the follow up visit, 93 patients had microbiological control, microbiological cure was observed in 79 of the 84 (94.05%) patients who had positive results of the cultures taken at the first visit. Five patients still had an infection: One had candidiasis and four had BV. One patient who had BV at the time of admission still had BV and also presented candidiasis. Of the ten patients who had negative microbiological results at the time of admission, six continued to have negative tests, one was follow up loss and three had a de novo infection (two candidiasis and one BV) (figure 2).
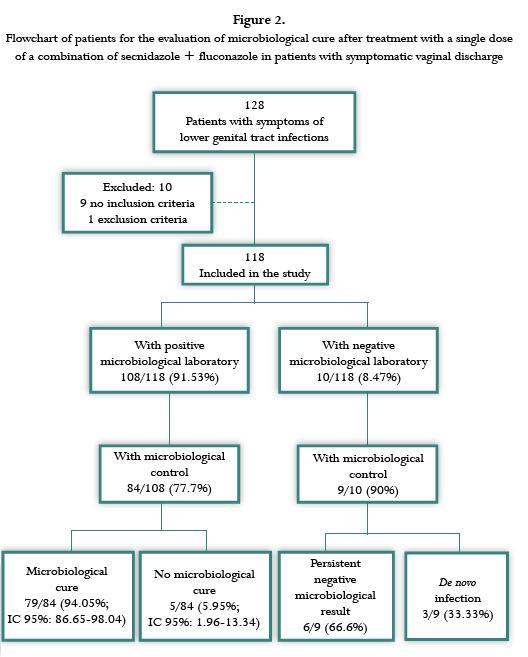
In the group of patient with microbiological control, after treatment, 33 of the 34 patients with candidiasis diagnosed by culture at the time of admission had negative cultures, founding a microbiological cure rate for candidiasis of 97.1%, and of the 58 patients with an initial BV diagnosis and with microbiological control, 55 demonstrated microbiological cure (94.38%).
A second follow-up evaluation was performed face-to-face or over the phone with 96 patients. At this visit three participants (3.12%) had a syndromic diagnosis of vaginal discharge, that corresponded in the microbiological results to a one persistent candidiasis, one recurrent candidiasis (a positive culture at the time of admission and a negative culture at the first follow-up visit), and the other patient has recurrent candidiasis plus de novo BV.
Adverse events occurred in 15 patients (16.13%): 12 experienced nausea (12.90%), three experienced headache (3.23%), three experienced gastritis (3.23%), and two experienced vomiting (2.15%). Twelve cases (12.90%) were considered drug-related, and there were no serious adverse events. Five patients (4.76%) had a blood count at the time of admission that indicated mild leukocytosis, but these blood counts normalized in the follow-up laboratory test. Two patients (2.11%) who initially had a normal blood count showed slight changes at the time of the follow-up visit but did not demonstrate leukopenia or thrombocytopenia.
The median AST level at the time of admission was 18.5 U/L (interquartile range (IQR): 7-42), and the median ALT level was 18.5 U/L (IQR: 8-77). At the first follow-up visit, the median AST and ALT levels were 20 U/L (IQR: 10-38) and 18 U/L (IQR: 9-67), without differences with the baseline values (p = 0.0536 for AST and p = 0.8829 for ALT). No patients showed a significant increase in the blood transaminase levels.
DISCUSSION
The specific prevalence of the infections found in this study of symptomatic women with vaginal discharge were 57.11% for BV, 28.81% for candidiasis, and 10.17% for mixed infections (BV plus candidiasis). There were no cases of Trichomonas infection, and 10 patients (8.47%) had negative laboratory results at the time of admission. Of the Candida species, 65.22% were Candida albicans, and the remaining samples were other Candida species.
These results are consistent with those published worldwide. BV and Candida are the most common causes of vaginal infections in symptomatic women, the prevalence of BV being 22-50% and the prevalence of Candida 17-39% (12). One study reported that among women with symptoms of genital tract infections in Colombia, the prevalence of BV was 39.6%, the prevalence of candidiasis was 11%, and the prevalence of trichomoniasis was 1% (8). In that study, Candida albicans accounted for 96.1% of the Candida isolates, a higher proportion than the founded in the present investigation. This study was not designed to determine the etiological prevalence of all genital tract infections because the participants included were patients with symptomatic vaginal discharge who required treatment.
In the present study, the overall clinical cure rate with the combination of oral secnidazole plus fluconazole was 90.38%, and the microbiological cure rate was 94.05%. Sensitivity analysis: For clinical cure, assuming that all 14 patients lost to follow-up would not have shown clinical cure, the cure rate would be 79.66% (94/118). Assuming that all 14 patients lost to follow-up were clinically cured, the cure rate would be 91.52% (108/118).
For microbiological cure, assuming that all 24 patients lost to follow up, had not demonstrated microbiological cure, the cure rate would be 66.94% (79/118). Assuming that all 24 patients, who did not have microbiological control, had demonstrated microbiological cure, the cure rate would be 95.37% (103/108).
The microbiological cure rate for BV was 94.38%. The reported effectiveness of BV treatment is similar to the reported effectiveness of metronidazole treatment in a meta-analysis, which found cure rates of 85% to 87% for treatments with different schedules (13). A recent meta-analysis on BV treatment for non-pregnant women concluded that in comparison with a placebo, clindamycin showed a lower failure rate (RR = 0.25; 95% CI: 0.16-0.37), but clindamycin and metronidazole had identical rates of failure regardless of the regimen (RR = 1.01; 95% CI: 0.69-1.46) (14). This meta-analysis included only one treatment regimen with secnidazole. The study compared 1 g vs. 2 g and found clinical cure rates of 95.5 and 97.4%, respectively with similar adverse events (10). The efficacy observed in the present study is similar to the results reported in the meta-analysis (15).
With regard to the treatment of candidiasis, the present study found a 97.1% microbiological cure rate. A systematic review comparing intravaginal treatment with nitroimidazoles (clotrimazole, miconazole, econazole, and butoconazole) to oral fluconazole or itraconazole found that both treatments were equally effective in the short and long term, with cure rates of 82% vs. 83% (OR = 1.03; 95% CI: 0.72-1.49) (16).
Regarding the safety of the combination of oral secnidazole plus fluconazole, 16.13 % of the patients in this study reported no serious adverse events. It has been reported in the literature that treatments with clindamycin tend to cause fewer adverse events than those with metronidazole (RR = 0.75; 95% CI: 0.56-1.02) (14). A metallic taste, nausea, and vomiting are more common with metronidazole treatment (14).
The changes in blood count and liver function tests observed in the present study did not reach clinical significance. It has been reported that increased transaminases occurs in 1% to 9% of asymptomatic and apparently healthy individuals. Likewise, some laboratories consider the normal reference values as under 40 U/L for AST and under 50 U/L for ALT (17).
One of the consequences of BV treatment is Candida albicans superinfection, which occurred in 3.23% of the patients of the present study. This frequency is lower than the figures that have been reported in the literature. Studies have found that Candida superinfection rates were between 15% (13, 18) to 25% (19) after treatment with metronidazole.
The strengths of this study include the design, the standardization of the syndromic diagnostic process and of the techniques and interpretation of laboratory results and the use of gold standard methods for determining the etiologic diagnoses. The adherence to treatment was 100% because the drug was administered in a controlled manner during the consultation.
The limitation of the present study is not to have a control group, although it included etiologic diagnoses and follow-up. The number of patients included was determined by convenience; however, it was possible to obtain an adequate number of patients to assess the efficacy of treatment for two types of infections. Twenty two percent of the patients were lost for the microbiological follow-up, but a sensitivity analysis for the worst and best scenarios was conducted.
CONCLUSION
BV was the most common infection in this study, followed by candidiasis and mixed infections. A single dose of the combination of oral secnidazole plus fluconazole achieved clinical and microbiological cure rates greater than 90% in patients with symptomatic lower genital tract infections. The patients reported gastrointestinal side effects but there were no serious adverse events. RCT comparing this combination against single treatment for each type of infection should be done in order to evaluate its effectiveness.
ACKNOWLEDGMENTS
The authors wish to thank the Engativá Hospital, which provided facilities for the study, the patients who participated, and the staff members who recruited, evaluated, and treated the patients (Dr. Tatiana Pacheco, bacteriologist Marleny Sierra, and Nurse Jenny Bonilla). We also thank to nurse Natalia Calderon, for coordinating the study and digitizing the database.
REFERENCES
1. Sewankambo N, Gray RH, Wawer MJ, et al. HIV and HIV-2 infection associated with abnormal vaginal flora morphology and bacterial vaginosis. Lancet. 1997;350:546-50. [ Links ]
2. Hashemi FB, Ghassemi M, Roebuck KA, Spear GT. Activation of human immunodeficiency virus type 1 expression by Gardnerella vaginalis. J Infect Dis. 1999;179:924-30. [ Links ]
3. Jackson DJ, Rakwar JP, Bwayo JJ, Kreiss JK, Moses S. Urethral Trichomonas vaginalis infection and HIV-1 transmission. Lancet. 1997;350: 1076. [ Links ]
4. World Health Organization. Guidelines for the management of sexually transmitted infections 2005. [Visited 2011 nov 11]. Available in: http://www.who.int/hiv/pub/sti/pub6/en/. [ Links ]
5. van Dam CJ, Becker KM, Ndowa F, Islam MQ. Syndromic approach to STD case management: where do we go from here? Sex Transm Infect. 1998;74(Suppl 1):S175-8. [ Links ]
6. Msuya SE, Uriyo J, Stray-Pedersen B, Sam NE, Mbizvo EM. The effectiveness of a syndromic approach in managing vaginal infections among pregnant women in northern Tanzania. East Afr J Public Health. 2009;6:263-7. [ Links ]
7. República de Colombia. Ministerio de Salud. Dirección General de Promoción y Prevención. Normas técnicas y guías de atención. Acuerdo 117/98, Resolución 412/2000. [Republic of Colombia. Ministry of Health. Promotion and Prevention Directorate-General. Technical standards and guidelines of care.Agreement 117/98, Resolution 412/2000. [ Links ]]
8. Angel-Müller E, Rodríguez A, Núñez-Forero LM, Moyano LF, González P, Osorio E, et al. The prevalence of and factors associated with C. Trachomatis, N. Gonorrhoeae, T. Vaginalis, C. Albicans infection, syphilis, HIV and bacterial vaginosis in females suffering lower genital tract infection symptoms in three healthcare attention sites in Bogotá, Colombia, 2010. Rev Colomb Obstet Ginecol. 2010;63:25-35. [ Links ]
9. De Punzio C, Garutti P, Mollica G et al. Fluconazol 150 mg single dose versus itraconazol 200 mg per day for 3 days in the treatment of acute vaginal candidiasis: a double-blind randomized study. Europ J Obstet Gynecol Reprod Biol. 2003;106:193-7. [ Links ]
10. Nuñez JT, Gómez G. Low-dose secnidazole in the treatment of bacterial vaginosis. Int J Obstet Gynecol. 2005;88:281-5. [ Links ]
11. Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol. 1991;29:297-301. [ Links ]
12. Nyirjesy P. Vulvovaginal candidiasis and bacterial vaginosis. Infect Dis Clin N Am. 2008;22:637-52. [ Links ]
13. Lugo-Miro VI, Green M, Mazur L. Comparison of different metronidazole therapeutic regimens for bacterial vaginosis. A meta-analysis. JAMA. 1992;268: 92-5. [ Links ]
14. Oduyebo O, Anorlu RI, Ogunsola FT. The effects of antimicrobial therapy on bacterial vaginosis in nonpregnant women. Cochrane Database of Systematic Reviews 2009, Issue 3. Art. No.: CD006055. DOI: 10.1002/14651858. CD006055. pub2. [ Links ]
15. Armstrong NR, Wilson JD. Tinidazole in the treatment of bacterial vaginosis. Int J Womens Health. 2009;1:59-65. [ Links ]
16. Nurbhai M, Grimshaw J, Watson M, et al. Oral versus intra-vaginal imidazole and triazole antifungal treatment of uncomplicated vulvovaginal candidiasis (thrush). In: The Cochrane Library, Issue 4, Chichester: John Wiley & Sons; 2007. [ Links ]
17. Aragon G, Younossi ZM. When and how to evaluate mildly elevated liver enzymes in apparently healthy patients. Cleve Clin J Med. 2010;77:195-204. [ Links ]
18. Jerve F, Berdal TB, Boham P, et al. Metronidazole in the treatment of non-specific vaginitis (NSV). Br J Vener Dis. 1984;60:171-174. [ Links ]
19. Hovik P. Nonspecific vaginitis in an outpatient clinic: comparison of three dose regimens of metronidazole. Scand J Infect Dis Suppl. 1983;40:107-110. [ Links ]
Conflict of interest statement and intellectual property. The study: "Effectiveness and safety of the combination of fluconazole and secnidazole for the treatment of symptomatic vaginal discharge. Bogotá D. C., Colombia", is of intelectual property of the National University of Colombia. It was funded by Lafrancol S.A.S., which had access to the information only to verify the quality of the recorded data. The data analysis and results and the preparation of the manuscript were completely independent from the funding body. The funding body previously agreed to the publication of the study regardless of the direction of the results.













