INTRODUCTION
The progressive institutionalization of birth has resulted in evident improvements in fetal and neonatal care, but also in a a growing number of cesarean sections 1,2. In the United States, the rate of cesarean section has been estimated at around 32.8% of all deliveries, with a more marked increase among African-Americans 3,4. In Colombia, the rate of cesarean section has also shown a rising trend during the last decade, reaching 43.4% of all births in the year 2012 2. In the rest of Latin America, cesarean sections have also increased 5.
An important contributor to this rising trend is the surge in cesarean deliveries upon maternal request (CDMR): A cesarean section performed in a woman with a singleton, term pregnancy, by maternal request and with no medical indication 6. The use of this procedure has given rise to in-depth medical, legal, ethical and financial debates, especially concerning the use of limited health resources for an elective procedure 7. On the other hand, it is not possible to ignore that CMDR is a frequent procedure. Despite under-registration, CDMR is estimated to represent up to 4-15% of all deliveries in the United States, and up to 82% of obstetricians recognize having performed at least one CDMR 8,9. There is also a great degree of variation in the use of CDMR, ranging between close to 6% in the United Kingdom 10 and up to 80% of deliveries in Brazil 11. There are a host of patient and obstetrician-associated factors that contribute to this increase in CDMR. Patient factors include fear of pain, a sense of greater safety and control over a somewhat unpredictable event, and the perceived lower risk of urinary incontinence in the mother and/or hypoxic complications in the neonate 12. Obstetrician factors include a pragmatic view of birth, optimization of work time, avoidance of legal complications, while improvements in surgical safety may also play a role 13.
There is a great deal of controversy regarding the conveniency of CDMR for the mother and the baby. A summary review of the evidence by the United States National Institutes of Health found that CDMR may be accompanied by a lower risk of hemorrhage or need for transfusion and a lower risk of trauma/organ injury in the index pregnancy 14. However, there is still uncertainty about the impact of CDMR on other short-term maternal and neonatal outcomes, as well as on subsequent pregnancies 13. Direct evidence about the risks of CDMR, particularly when compared to alternative modes of delivery, is extremely limited 6.
Since the evidence to support the practice of CDMR is mostly based on retrospective analyses, the objective of this study was to compare, in a prospective observational setting, a) Multiple maternal outcomes among low-risk women who intended to have CDMR versus vaginal delivery, and b) Multiple neonatal outcomes among the same types of delivery in the same study sample. We hypothesized that the frequency of maternal and neonatal outcomes would not be different between CDMR and vaginal deliveries.
MATERIALS AND METHODS
Study design and setting: This was a prospective observational cohort study. Our institution is a private university hospital affiliated to Universidad de los Andes. Most of our patients are from a low risk obstetric population and have private medical insurance, or are affiliated to the health system under the contributive regime for employed individuals.
Study participants. For this study we selected obstetric patients between 18 and 45 years of age with a singleton, term, low risk pregnancy, defined as any uncomplicated pregnancy up to the moment of the mother's choice of mode of delivery. Patients were mothers who delivered in our institution and were recruited in the study between June 2008 and April 2012. Exclusion criteria were any medical indication or contraindication for cesarean delivery, and any maternal or fetal disease or condition potentially associated with a poor perinatal outcome.
For sample size calculation purposes, and based on data from historic records of our Department, we assumed an expected cumulative incidence of the primary endpoint (any adverse neonatal event over a 1-year timeframe) of 9.9% in the CDMR group, and of 19.7% in the spontaneous labor group. Among eligible low-risk pregnant women, we expected a ratio of 1 CDMR for every 2 spontaneous deliveries. Using the expression for the calculation of sample sizes in cohort studies that contrast hypotheses between independent groups, in order to have at least 90% power to reject the null hypothesis of equal rates of neonatal complications with a type I error rate of 5%, we needed a minimum of 200 CDMRs and 400 vaginal deliveries.
Procedure. Mothers who intended to have a vaginal delivery and spontaneously initiated labor were admitted to the obstetric unit with onset of uterine activity at or after 37 weeks of gestational age. All mothers deemed eligible for the study were invited to participate by their obstetrician or one of the researchers, and those who accepted signed an informed consent form before week 36 of pregnancy during a prenatal consultation. There were no informed consent refusals. All Department obstetricians agreed to participate voluntarily in the study, got acquainted with the study case report forms beforehand, and committed to entering all the required information in the patient´s medical record. Two research assistants manually extracted from the medical record to the study case report forms the baseline information on the day of delivery, and did the same with the outcomes information 15 days later during the postnatal consultation. They also checked for data validity and completeness. Given the nature of the study, researchers in charge of collecting the information were not masked to each patient's exposure.
For all cases, the routine protocol for vaginal delivery in our hospital included the following: a) venous access for administration of parenteral fluids; b) intra-partum fetal monitoring at the discretion of the treating obstetrician; c) obstetric analgesia; d) permanent on-site availability of obstetric medical staff; e) permanent observation and follow-up of the mother by professional nursing staff; f) newborn care by a neonatologist; and g) monitoring of the mother during the immediate postpartum in a recovery room prior to transfer to the ward.
The decision to induce labor was made when women who intended to have a vaginal delivery presented a medical/obstetric indication for finishing pregnancy or when there was evidence of unsatisfactory fetal status on fetal surveillance ("non-reassuring fetal status") in the presence of a favorable cervix. The induction protocol comprised cervical application of dinoprostone (prostaglandin E2) gel 0.5 mg every 6 hours (maximum 3 doses in 24 hours), and elective complementary use of oxytocin 6-12 hours after the last dinoprostone dose. Once the woman was in labor, the vaginal delivery protocol was followed as explained above.
The decision to undergo vaginal delivery or CDMR was entirely dependent on the woman's personal preference. Mothers in the CDMR group were admitted to the obstetric unit on the scheduled date. In all cases, the routine protocol included, a) verification of gestational age >=39 weeks estimated by first trimester ultrasound; informed consent procedure; c) venous access for administration of parenteral fluids; d) antepartum fetal monitoring at the discretion of the treating obstetrician; e) Reservation of blood; f)permanent availability of anesthesia by a specialized obstetric anesthesiologist; g) Permanent availability of an operating room and of an additional shift obstetrician; h) newborn care by a neonatologist; i) Permanent observation and follow-up of the mother by professional nursing staff; and j) monitoring of the mother during the immediate postpartum in a recovery room prior to transfer to the ward.
Follow-up lasted for 15 days after delivery. Information on study outcomes was actively collected and recorded during each mother's hospital stay, and during the ensuing 15 days.
Variables to be measured: maternal age was recorded on the day of delivery. Intergestational period was defined as the time between the last delivery and the last menstruation before the index pregnancy. Inter-gestational period was only computed for non-primiparous mothers. Gestational age was confirmed in every participant by a fetal crown-rump length determination before 14 weeks of pregnancy, using Hadlock's standard growth curves for gestational age. Type of insurance was considered according to the structure of the Colombian health system: mandated medical insurance is the mandatory insurance that every employee must have, and is paid in part from salary discounts and in part from direct contributions by the employer. Private medical insurance is a voluntary coverage taken by citizens who want to have a wider coverage than what is included in mandatory insurance. There is also a group of patients without insurance who pay out of pocket for medical care. Occupation was considered in three categories: housewife, full-time worker or student. Number of gestations including current gestation, number of prior deliveries and number of abortions were treated as discrete numeric variables.
The study exposure was the mode of delivery intended by the mother. Within the vaginal delivery group, and given the potentially different impact on mother and child, induced deliveries were analyzed separately. Thus, the three cohorts being compared were 1) CDMR (women with >=39 weeks of pregnancy); 2) spontaneous vaginal delivery (per study protocol, women with >= 37 weeks of pregnancy were eligible, analyses were restricted to women with >= 39 weeks of pregnancy); 3) induced vaginal delivery (women with >= 39 weeks of pregnancy). The primary maternal endpoint was the occurrence of at least one of the following conditions in the mother: need for blood transfusion during the delivery or during the postpartum period, hysterectomy, admission to the intensive care unit (ICU), obstetric trauma and puerperal infection (surgical site infection, myometritis or endometritis). Secondary maternal endpoints were: development of a perineal tear during delivery (grade 1, 2, 3 or 4), length of mother's hospitalization, and maternal mortality. The primary neonatal endpoint was the occurrence of at least one of the following conditions in the neonate: 5 minutes APGAR score below 7, low birth weight, cephalohematoma, jaundice, hypoglycemia, hypokalemia, neonatal sepsis, transient tachypnea of the newborn, hyaline membrane disease, pneumonia, enterocolitis, asphyxia, meconium aspiration, apparent life-threatening event (ALTE - characterized by a combination of apnea, cyanosis and abnormal muscle tone), malformations, intubation or neonatal death. Secondary neonatal endpoints were low birth weight and need for hospitalization of the neonate. All study participants were followed for 15 days after delivery for the evaluation of maternal or neonatal outcomes.
Statistical analysis. In the descriptive analysis of demographic and clinical variables in the three groups (CDMR, induced labor and spontaneous labor), means ± standard deviation (SD) were used for continuous numeric variables, medians and ranges for discrete numeric variables, and proportions were expressed as percentages for nominal variables. A chi-square test was used for proportion comparisons, and continuous variables using independent sample t-tests (for comparisons between two groups), and one-way ANOVA with mode of delivery as fixed factor were used for comparisons among more than 2 groups. For discrete numerical variables, comparisons of medians between groups were made using Wilcoxon's test. Normality of continuous variables was tested with a Kolmogorov-Smirnov goodness of fit test, and for comparisons of non-normally distributed variables we intended to use Wilcoxon's test, even though we did not have to. For all post-hoc pairwise comparisons with Tukey's test, spontaneous labor was the reference group (i.e., induced vaginal versus spontaneous vaginal, CDMR versus spontaneous vaginal). We analyzed the association between mode of delivery and the primary and secondary outcomes in a univariate model that included only mode of delivery as single predictor, and in a fully adjusted multivariate model that included confounders that either, a) had a high biological plausibility of impact on maternal/ neonatal outcomes, or b) exhibited significant (even if small) differences among the groups under comparison. We used a 5% significance level and reported 95% confidence intervals for all crude and adjusted relative risks. Only patients with complete data on all relevant exposures and outcomes were analyzed. We performed sensitivity analyses of both the maternal and the neonatal outcome, excluding all mothers who started their labor as spontaneous or induced, but later had an unplanned cesarean section.
Ethical aspects. The study was approved by the Institutional Ethics Committee of Fundación Santa Fe de Bogotá (Reference number CCEI-1412-2011). All participants provided a written informed consent. All CDMR procedures were discussed and approved by the Ob/Gyn Department Board Meeting.
RESULTS
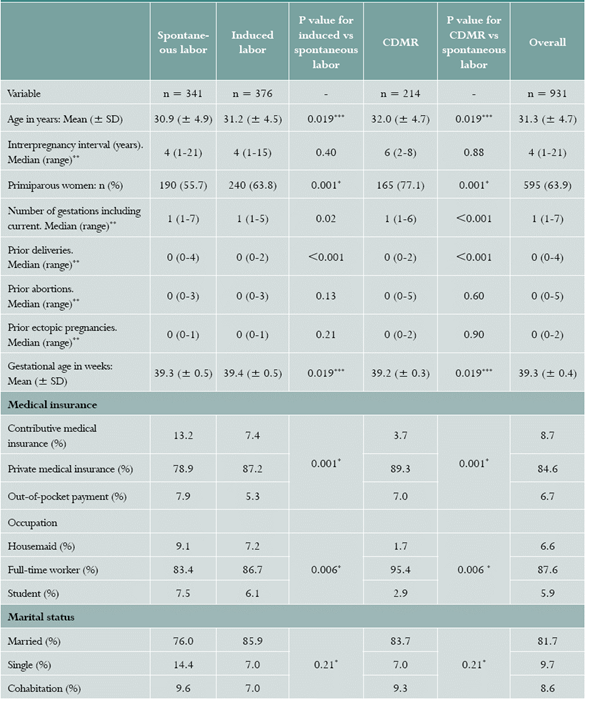
During the study follow-up, 214 women had cesarean delivery upon maternal request, and 717 went into labor: 341 labors started spontaneously and 376 were induced. The number of patients enrolled by year was: 95 patients in 2008, 62 patients in 2009, 287 patients in 2010, 301 patients in 2011, and 186 patients in 2012. Among the 341 women who began labor spontaneously, there were 57 cesarean sections (16.7% rate of unplanned cesarean delivery), while among the 376 women who had an induced labor, there were 148 cesarean sections (39.4% rate of unplanned cesarean delivery). Thus, the total study population comprised 931 women and their newborns (Table 1). The average age of study participants was 31.3 ± 4.7 years, being slightly but significantly higher in the CDMR group compared to the spontaneous labor group. The overall median length of the inter-gestational period among non-primiparous women was 4 years, without significant differences across groups. There was a larger proportion of primiparous women in the CDMR group (Table 1). These differences are of little clinical significance due to their small magnitude. Mean gestational age at delivery was similar between the spontaneous and induced labor groups and significantly shorter in the CDMR group, albeit by a very small magnitude (0.1 weeks shorter). Relative to women in the spontaneous and induced labor cohorts, a larger proportion of women in the CDMR cohort had private medical insurance or reported their work status as "full-time worker".
Maternal outcomes. The primary maternal outcome occurred in 29 participants (3.1% of the total study sample). The absolute frequency of the primary maternal outcome was lower in the CDMR group (0.9%) than in the vaginal delivery groups (3.5% in the spontaneous, 4.0% in the induced) (Table 2). The relative risk of the primary maternal outcome in the CDMR group relative to the spontaneous labor group was 0.26 (95% CI: 0.06-1.17). After adjusting for multiple confounders including the final way of delivery (vaginal or cesarean) in logistical models, the negative association of CDMR with the primary maternal outcome persisted and became significant (OR 0.21 [95% CI: 0.05- 0.97]) (Table 3). The risk of the primary maternal outcome was not significantly different between the spontaneous and induced labor groups (Table 3).
Table 2 Cumulative incidence of adverse maternal outcomes, by mode of delivery
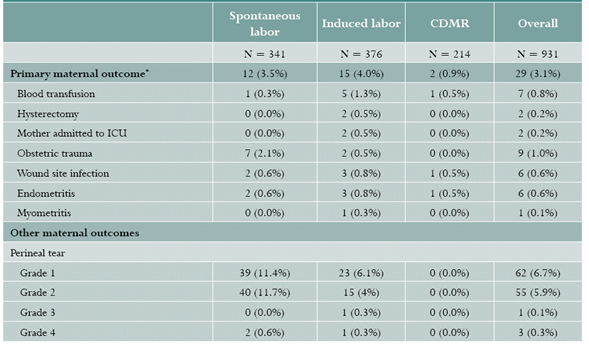
* Women who presented more than one separate component of the primary outcome were counted only once for the aggregate primary outcome.
CDMR: Cesarean delivery on maternal request.
Table 3 Odds ratios (OR) and 95% confidence intervals of the maternal primary outcome in univariate and multivariate logistic models

Univariate model: Mode of delivery as only predictive variable. Fully adjusted model: Additional adjustment for age, number of gestations, gestational age and type of medical insurance. Data are OR (95% CI). Ref: Reference group. CDMR: Cesarean delivery on maternal request.
Perineal tears, especially grades 1 and 2, occurred more frequently in spontaneous deliveries than in induced ones (Table 2). Naturally, there were no perineal tears in the CDMR group. Hospitalization of the mother was significantly longer in the induced and CDMR groups than in the spontaneous groups, but only by a small magnitude (2.3 ± 0.6 days in the spontaneous group, 2.6 ± 0.7 days in the induced group, 2.8 ± 0.6 days in the CDMR group, p<0.001 for both comparisons versus spontaneous). When comparing spontaneous and induced labor deliveries, the frequency of episiotomies (40.8% versus 39.1%, respectively) and of instrumented deliveries (21.1% versus 22.1%, respectively), was very similar.
Neonatal outcomes. The proportion of neonates of each gender was similar in the CDMR, spontaneous and induced labor groups (49.6%, 51.3% and 50.5% female newborns, respectively). The primary neonatal outcome occurred in 189 neonates (20.3% of the total study sample). The absolute frequency of the primary neonatal outcome was lower in the CDMR group (15.0%) than in either of the vaginal delivery groups (23.5% in the spontaneous, 20.5% in the induced) (Table 4). The relative risks of the neonatal outcome were 0.64 (95% CI: 0.44-0.93) for CDMR delivery and 0.87 (95% CI: 0.66-1.15) for IVD. After adjusting for multiple confounders in logistical models (including final form of delivery), the negative association of CDMR with the primary neonatal outcome was still significant (OR 0.59 [95% CI: 0.36-0.93]) (Table 5). After multivariate adjustment, induced labor was no longer associated with increased or decreased incidence of the primary neonatal outcome (OR 0.84 relative to spontaneous labor, 95% CI:0.59-1.21) (Table 5).
Table 4 Cumulative incidence of adverse neonatal outcomes, by mode of delivery
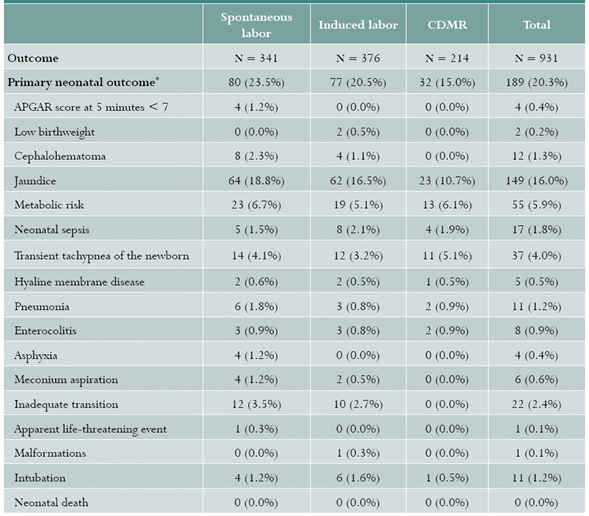
Babies who presented more than one separate component of the primary outcome were counted only once for the aggregate primary outcome.
Table 5 Odds ratios (OR) of the neonatal primary outcome in multivariate logistic models
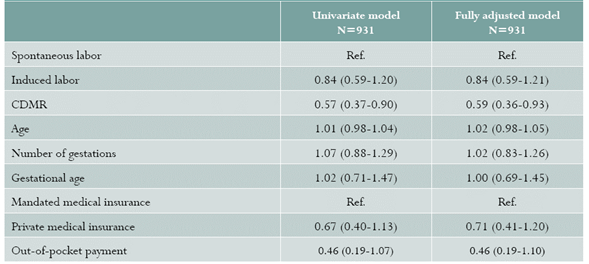
Univariate model: Mode of delivery as only predictive variable. Fully adjusted model: Additional adjustment for age, number of gestations, gestational age and type of medical insurance. Data are OR (95% CI). Ref: Reference group. CDMR: Cesarean delivery on maternal request.
The frequency of hospitalization of the baby was lowest in the CDMR group (10.3% versus 15.8% for spontaneous, 16.2% for induced), this association was close to statistical significance (OR for hospitalization of the baby in the CDMR group with spontaneous labor as reference group: 0.64 [95% CI: 0.41 - 1.03])(Figure 1). The average weight of the baby did not differ significantly among the three groups: 3161 (± 311 g) in spontaneous labor; 3153 (± 298 g) in induced labor; 3117 (± 300 g) in CDMR; p=0.9 for induced vs spontaneous, p=0.17 for CDMR versus spontaneous. APGAR score at 5 minutes was similar in the three study groups (Median 9.0, interquartile range 9-10 for the three groups).
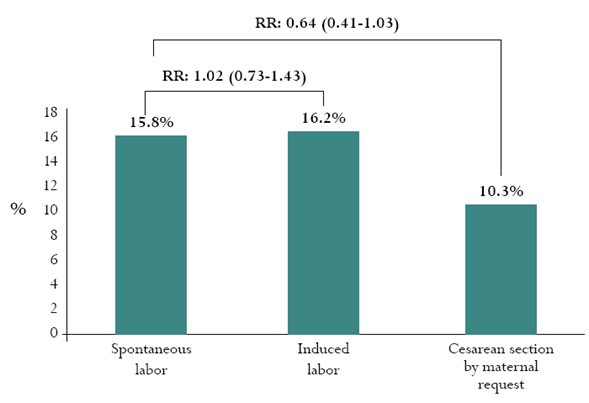
Figure 1 Rates of newborn hospitalization by mode of delivery Legends above bars represent relative risks and their 95% confidence intervals, with the spontaneous labor group as reference.
Sensitivity analyses. In a sensitivity analysis excluding all patients who had an unplanned cesarean section (n=726 for this analysis), the frequency of the maternal outcome was still lowest in the CDMR group, in a proportion similar to that observed in the complete study sample (0.9% in the CDMR group, 3.2% in the spontaneous vaginal group, 3.1% in the induced vaginal group). When compared only to women in the spontaneous vaginal group who actually delivered vaginally, the RR of the maternal outcome for CDMR was 0.29 (95% CI: 0.06-1.35, p=0.11). Results for the neonatal outcome were similar: 15.0% in the CDMR group, 21.9% in the induced vaginal group, 24.3% in the spontaneous vaginal group. The RR of neonatal outcome for CDMR compared with babies born to women in the spontaneous vaginal group who actually delivered vaginally was 0.62 (95% CI: 0.42-0.90, p=0.012). Relative to women in the spontaneous vaginal group who delivered via unplanned cesarean section, the RR of the maternal outcome in the CDMR group was 0.17 (95% CI: 0.03-1.37). Similarly, relative to women in the induced vaginal group who delivered via unplanned cesarean section, the RR of the maternal outcome in the CDMR group was 0.33 (95% CI: 0.07-1.52).
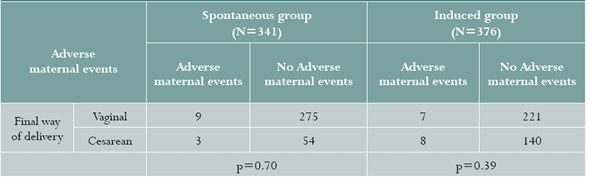
In a descriptive analysis, we explored the frequency of adverse maternal and neonatal events simultaneously among patients who intended to have a vaginal delivery, stratifying by study group (spontaneous, induced) and final form of delivery (vaginal or cesarean); these results are presented in Table 6. The frequency of adverse maternal events in either group was not associated with the final form of delivery (p from Chi-square test=0.70 for spontaneous, p=0.39 for induced).
Table 6 Frequency of adverse maternal outcomes, stratified by study group (excluding CDMR) and final way of delivery
In one additional sensitivity analysis, we explored the occurrence of a modified neonatal outcome that did not include jaundice. The frequency of this outcome was also lowest in the CDMR group: 14.1% for spontaneous, 11.7% for induced and 9.3% for CMDR. The OR for CDMR versus spontaneous was 0.63 (95% CI: 0.36-1.09), and the OR for induced versus spontaneous was 0.81 (95% CI: 0.52-1.26).
DISCUSSION
In this study, we assessed the short-term impact of CDMR, spontaneous vaginal delivery or induced vaginal delivery on the mother and the newborn.
Despite the three groups being remarkably similar at inclusion, we found a lower absolute rate of adverse maternal and neonatal outcomes among women who chose CDMR over a vaginal delivery. Furthermore, when we adjusted for the effects of variables with the highest potential to be confounders, this result persisted to be significant, in some cases yielding even lower estimates of the Odds ratio. Despite the widely held belief that cesarean sections translate into longer hospitalizations, the absolute difference in length of stay between the CDMR and spontaneous vaginal delivery groups was on average 0.5 days, a difference that carries very little clinical significance.
Somewhat unexpectedly, the rate of the primary neonatal outcome was also lower in the CDMR group, a difference that also persisted after correction in multivariate models. We consider this a notable result, since multiple relevant adverse neonatal outcomes were closely assessed and registered. Moreover, newborns from CDMR women were hospitalized significantly less, and had slightly higher APGAR scores than those born vaginally. Clearly our results do not match those of other studies like the World Health Organization (WHO) Global Survey on Maternal and Perinatal Health 15. In this study, cesarean sections were associated with an increased risk of severe adverse maternal outcomes. A key part of the answer lies in the fact that this and many other studies have analyzed elective and emergency, term and preterm, low and high risk cesarean sections as a single group. Our results seem to point out that, under the right conditions, CDMR may be an intervention with a positive impact on both mother and child.
Different factors have led to a consistent worldwide rise in the number of cesarean deliveries, including common perceptions about risks associated with each route of delivery 16,17. Given the constant increase in women's request for CDMR and the difficulty of conducting randomized trials to address this particular question 18, it is essential to generate good observational evidence that may inform clinical recommendations.
We found a very low rate of obstetric hemorrhage requiring blood transfusion in all groups (0.3% in spontaneous vaginal, 1.3% in induced vaginal, 0.5% in CDMR). In a retrospective analysis of more than 400,000 deliveries, Holm et al. found a lower risk of severe post-partum hemorrhage with CDMR in both nulliparous women and in women with a previous cesarean section 19. There is evidence that the incidence of hemorrhage and obstetric shock is generally lower with elective cesarean section, and that the overall risk of blood transfusion is low except when associated with antepartum anemia and placenta praevia 20. In a Canadian population-based study of vaginal birth versus cesarean section indicated for breech presentation, maternal morbidity was similar between groups, but neonatal morbidity was lower among babies born by cesarean section 21. Conversely, in a retrospective analysis of almost 30,000 births in the United States, the incidence of persistent pulmonary hypertension was 3.7/1000 live births among neonates born by elective cesarean section, but only 0.8/1000 live births among neonates born vaginally 22. Part of the contradiction among results from different studies may stem from the role of gestational age as a confounding factor. This is illustrated by the fact that, when elective cesarean sections are performed after week 39, indices of neonatal respiratory morbidity are not increased relative to vaginal birth 23.
The main strengths of our study include its prospective nature, the careful and extensive documentation of outcomes and covariates and the use of homogeneous high-quality care protocols that allow to better tease out the advantages and disadvantages of each mode of delivery.
Study limitations. On the other hand, our main methodological limitation lies in the short postpartum follow-up, which does not allow us to examine long-term consequences of what in most women was a first delivery through CDMR. CDMR can be associated with multiple potential risks, which can be classified as immediate, late and long-term. We did not find an increased incidence of short-term risks (infection, hemorrhage, intra-operative genital/urinary lesions, other intra-abdominal complications, anesthetic risks or death), but we cannot rule out late (thromboembolic disease, prolonged recovery, hospital readmission, adhesions and incisional hernias) or long-term (abnormal placental implantation, uterine scar dehiscence/rupture, hysterectomy, infertility, early fetal loss, ectopic pregnancy and intrauterine growth retardation) complications in these patients 17. Longer prospective studies are needed in order to complement this short-term evidence with evidence of what happens in subsequent pregnancies.
There may be a self-selection phenomenon, whereby patients who voluntarily decide to have a CDMR bear other characteristics that make them less prone to perinatal complications. Comparison of baseline characteristics between groups does not suggest that this is the case, but residual confounding can never be discounted in an observational study. In addition, this was a single-center study in the context of our local reality, so our findings may not be relevant for other local or international contexts. These findings should not be used as the basis for general recommendations regarding cesarean sections. The demographics of our study participants showed healthy, actively working women, mostly in their early 30s, married, with private health insurance coverage, who presented for delivery with a term, low-risk pregnancy. It is only for patients with a similar condition, that these results may be applicable.
CONCLUSION
In summary, in this prospective study of term, low-risk pregnancies among women with a particular demography and chosen with strict inclusion criteria, CDMR was associated with a lower rate of adverse perinatal outcomes for both mother and newborn, compared to vaginal delivery. While these results may look encouraging, this evidence must not be used to propose CDMR as a first line alternative for childbirth. Multiple considerations limit the generalizability of our findings. However, they do suggest that when performed to the right women, in the proper context and with the right tools, CDMR may be a safe alternative to vaginal delivery for term, low-risk pregnancies.