PURPOSE
This summary provides an overview of priority actions recommended in the WHO Global STI Strategy. These recommendations can be used to build sustainable national and institutional STI capacity and ensure that the most important and cost-effective STI interventions reach the greatest number of people in need. Observations related to the Global STI Strategy and the findings from a national STI burden estimation workshop are described here for stakeholders in Colombia to consider as they identify opportunities to improve STI services and surveillance. A country -level strategy is needed in Colombia to develop and guide effective service delivery strategies within the current health system. Implementing interventions to control STIs will require multi-sectoral collaboration with other relevant health programmes, including maternal and child health, HIV prevention and treatment, adolescent health, and sexual and reproductive health. This broad, collaborative approach can significantly cut costs while amplifying the impact of the STI response.
BACKGROUND: THE STI STRATEGY AND THE IMPORTANCE OF STI CONTROL
Every day around the world, more than one million people acquire a sexually transmitted infection (STI). Some viral STIs, like Human Papillomavirus (HPV) and HIV, are still incurable and can be deadly, but some bacterial STIs - like chlamydia, gonorrhoea, syphilis and trichomoniasis are curable. Sequelae of untreated STIs include: adverse birth outcomes (stillbirth, neonatal death, low birth weight, congenital anomalies), infertility, pelvic inflammatory disease, and ectopic pregnancy. Syphilis outbreaks as well as antimicrobial resistance in gonorrhoea infections are additional emerging STI threats. Besides these burdens, STIs also increase the risk of HIV transmission. Much can be done to control the spread of STIs, alleviate harmful consequences and vastly improve quality of life. To address this critical health need and enable countries to reach health targets set by the Sustainable Development Goals (SDGs), the World Health Organization (WHO) developed the Global Health Sector Strategy on Sexually Transmitted Infections 2016-2021 1.
The WHO Global STI Strategy is one of three global health sector strategies developed alongside- the other two strategies address the control of HIV 2 and viral hepatitis 3. These three strategies support an integrated approach using the following common strategic directions: (a) information for focused action; (b) interventions for impact; (c) delivering for equity; (d) financing for stability; and (e) innovation for acceleration. All three strategies contribute to the 2030 Agenda for Sustainable Development and its SDGs 4 as well as the Secretary-General's Global Strategy for Women's Children's and Adolescents' Health (GSWCAH) 5. The WHO Global STI strategy establishes general guidance for countries to tailor STI prevention activities.
The WHO Global STI Strategy describes priority actions for countries for a stronger and more effective STI response that will help save millions of lives and improve the health of millions more. The range of actions for countries includes: (a) strengthening surveillance, program monitoring and progress evaluation, (b) STI prevention, (c) early diagnosis, (d) patient and partner management, as well as (e) approaches to reach the most vulnerable populations. Use or application of the WHO STI strategy can also support countries to prevent a range of other negative health outcomes resulting from undiagnosed and untreated STIs including adverse birth outcomes, infertility and other long term sequelae, and cervical cancer. The STI Strategy proposes the continuum of quality services - prevention, diagnosis, treatment and cure - to strengthen responses and ensure all populations in need are reached.
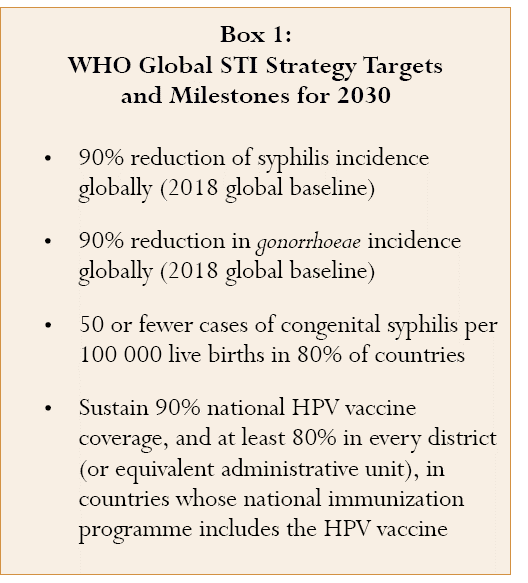
The WHO Global STI Strategy's public health approach focuses on three causative organisms of STIs that need immediate action and for which cost-effective interventions exist: (a) Neisseria gonorrhoeae as a cause of infertility, a risk factor for coinfection with other STIs and because of increasing bacterial resistance to antibiotic treatment, a; (b) Treponema pallidum given the impact of syphilis on pregnancy outcomes causing more than 350,000 adverse pregnancy outcomes each year (over half of which occur as stillbirths or neonatal deaths) and (c) Human papillomavirus due to its link to cervical cancer with 291 million prevalent cases of HPV, 530,000 new infections and 264,000 deaths each year from cervical cancer. The strategy sets global targets for these three STIs (Box 1).
IMPLEMENTING THE WHO GLOBAL STI STRATEGY
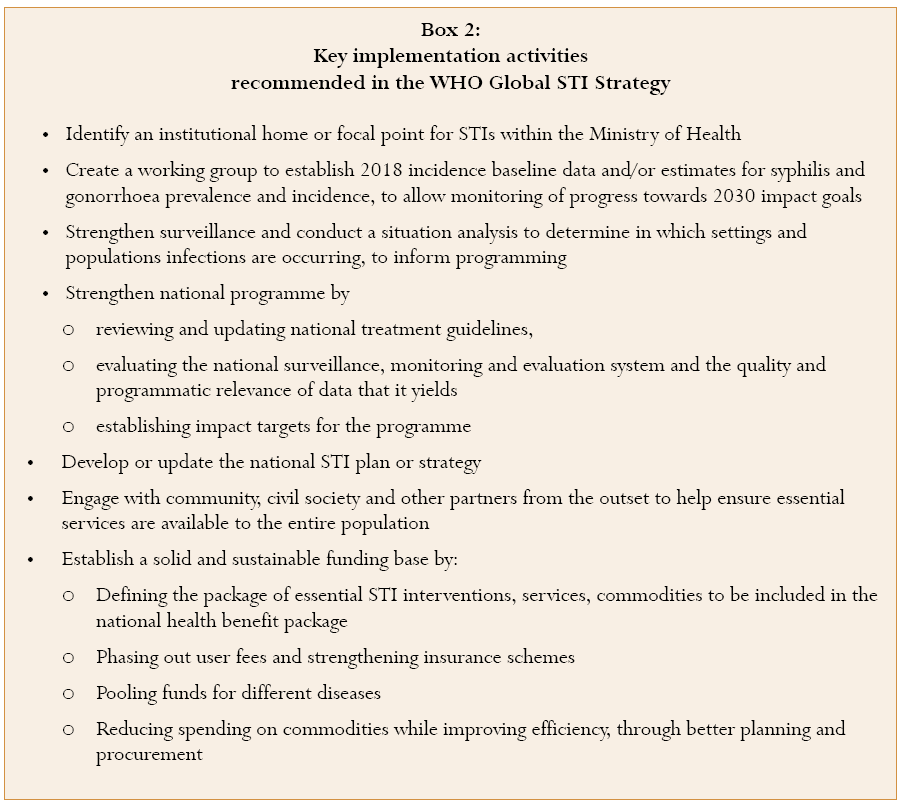
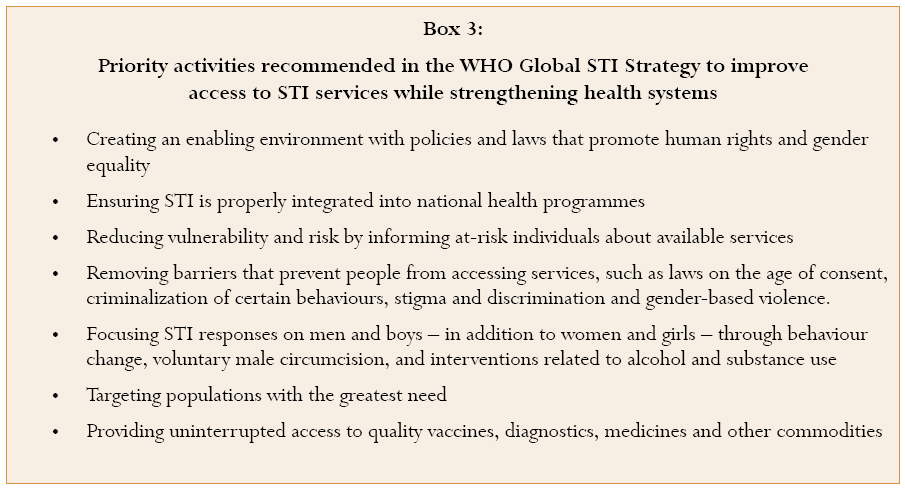
Understanding national STI epidemics is essential to developing a national strategic action plan. The Global STI Strategy urges countries to define a national strategic plan to control STIs that includes key actions (Box 2). These actions help to build a strong case for STI prevention and care that can rally political commitment and encourage much-needed government and stakeholder investment in STIs. Countries can thereby prioritise and tailor their program strategies and interventions for greatest impact in an STI programme that is feasible, cost-effective, equitable and sustainably financed while strengthening the overall health system (Box 3).
Assessing national progress through STI surveillance, monitoring, and evaluation
Surveillance, monitoring, and evaluation are instrumental in understanding STI trends and guiding program improvements. This includes assessing in which settings and populations STI infections occur, how transmission is facilitated, how effective service access and delivery can succeed in reducing STI spread and/or its health consequences, and what barriers stand in the way of access and use of STI services. A robust surveillance monitoring and evaluation system will help to ensure that programme implementation is on track to achieve service delivery and impact targets as envisioned in the national strategy and plan. STI surveillance programming includes: (a) integration of STI surveillance into the national health information system; (b) increasing the granularity of data by collecting information on risk factors and determinants; (c)
Identifying specific populations who are at greatest risk of STIs (d) periodic collection of prevalence data for gonorrhea, chlamydia and syphilis through representative sample surveys (both in known key risk populations, as well as in general low-risk populations), (e) capture of routine screening data (e.g. syphilis screening in ANC and in blood donors) and (f) STI case reporting with monitoring of overall trends, key populations with greatest risk of STIs, and program impact. WHO has developed simplified guidance on the core components of STI surveillance and core indicators for monitoring of STI prevalence (figures 1 and 2)6.
Prevention of STI transmission and acquisition
Combination prevention is the most effective way to prevent the transmission of STIs. Countries can therefore consider prioritizing prevention interventions through effective combination strategies that include: (a) comprehensive health information, education and promotion programmes for adolescents (b) male and female condom programming for protection against both STIs and unintended pregnancies, especially for adolescents (c) use of maternal and child health and family planning clinics to provide additional care and distribute condoms to women at risk of STIs (d) greater use of social marketing to improve supply and demand for STI services and condoms (e) promotion of voluntary male circumcision where appropriate and (f) ensuring access to HPV and hepatitis B vaccination.
Managing symptomatic patients and reaching sex partners
Primary point-of-care outlets - including primary health care clinics, sexual and reproductive health services and services that provide care and management for persons living with HIV - should follow updated management guidelines for symptomatic patients and their sexual partners. This includes: updating implementation plans for symptomatic STI management based on the latest evidence, encouraging the use of single-dose treatment, delivered if possible at a health facility to strengthen patient adherence, and integrating STI testing and treatment into health services for specific populations such as persons with HIV infection. Partner notification plays an essential role in STI treatment and care. Activities to strengthen sexual partner management should include: (a) adopting strategies for partner notification and evaluating their implementation (b) safeguarding patient confidentiality and (c) ensuring counselling and treatment of partners.
INTERVENTIONS FOR SUSTAINABILITY AND IMPACT
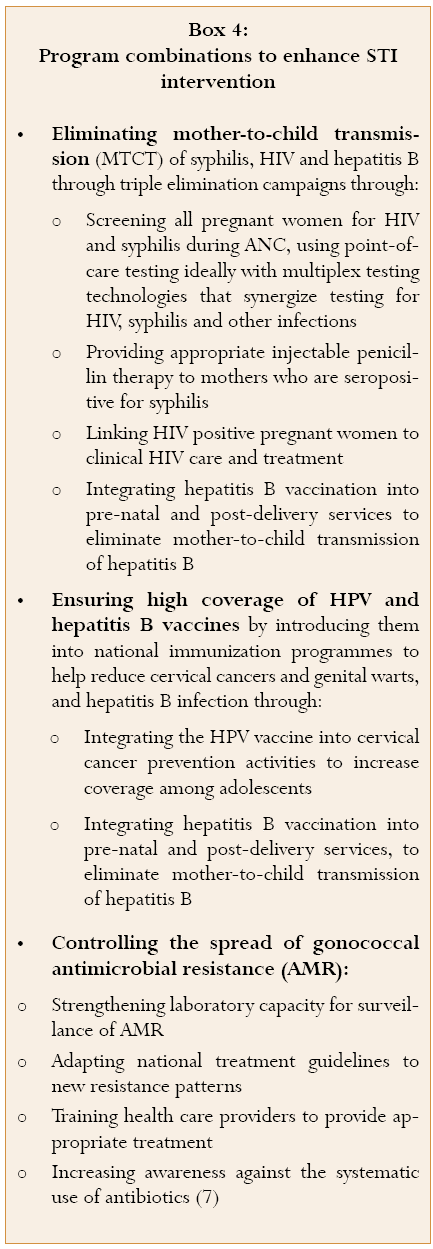
The impact of these interventions and of an STI programme as a whole can be enhanced by combining STI interventions with other relevant initiatives and programmes such as HIV education, mother and child health, cancer, immunization or sexual and reproductive health. The packaging of interventions for maximum impact can include ANC screening and treatment of syphilis and HIV, delivery of HPV and hepatitis B vaccines, and controlling the spread of gonococcal antimicrobial resistance (AMR) (Box 4). Strong linkages can significantly improve coverage of interventions and quality of care. The cost of STI interventions can also be reduced when these are delivered in combination with other services.
Focus on Colombia
In May of 2017, WHO conducted an STI surveillance workshop in Bogota with the Ministry of Health, to estimate the current and historic STI burden trends using the Spectrum STI estimation model 8-10. Colombia was the first South American country to implement this new surveillance tool, developed by Avenir Health within its broader suite of health planning software tools that is available for free through online download. Participants included ministry of health officials, National Health Institute, representatives of the national laboratory, and selected national STI care providers and academic researchers, as well as country and regional level WHO staff. Input from attendees and findings from the implementation of the Spectrum STI surveillance tool were used to evaluate the quality and utility of STI surveillance, and program progress and impact in Colombia. Priority actions for improving surveillance and program implementation were developed during the workshop, and these are summarized below.
For syphilis, the Spectrum estimations for congenital syphilis showed that recent improvements in ANC-based syphilis screening and treatment coverage since 2009 have resulted in decreasing annual numbers of congenital syphilis cases, but further improvements in both ANC services and in overall control of syphilis in the broader population are needed to accelerate progress towards congenital syphilis elimination 9. Monitoring of syphilis screening in pregnant women, the proportion diagnosed with syphilis, and the coverage and timeliness of treatment among those found syphilis-infected can inform program improvements and reduce negative birth outcomes due to congenital syphilis. In addition, monitoring pregnant women diagnosed with syphilis and tracking birth outcomes should include assessment of stillbirths and neonatal deaths for evidence of missed maternal syphilis infection. Follow-up and treatment of sexual contacts of pregnant women with syphilis can be strengthened, to reduce chances of re-infection after initial treatment early in the pregnancy and as a strategy to reduce the overall population-level burden of adult syphilis. Continued improvements in syphilis testing and treatment coverage among pregnant women can result in rapid declines in estimates of congenital syphilis. Elimination of congenital syphilis will require not only universal coverage of high-quality ANC-based-screening, but also reducing levels of syphilis in the overall adult population. In Colombia, case reporting and epidemiologic analysis of syphilis cases occurring in non-pregnant adults could inform syphilis prevalence and incidence assessments and could guide identification of "outbreaks" in at-risk populations such as men who have sex with men (MSM), youth, sex workers (SW), prisoners and high risk heterosexual populations. In addition, Laboratory reporting of numbers of syphilis tests performed, persons tested, positive syphilis results and the resulting test positivity rates could improve surveillance of adult syphilis.
For gonorrhoea and chlamydia, a Spectrum-based estimation of completeness of case reporting identified a large number of unreported cases of urethral discharge (a symptom of gonorrhoea and chlamydia). The WHO strategy recommends case reporting of urethral discharge in regions where etiologic diagnosis is not routinely available (figure 2). In addition to syndromic case reporting, WHO recommends systematic case reporting for gonorrhoea and chlamydia cases, and case reporting trends should be analysed alongside statistics of numbers of etiological tests conducted and the resulting test positivity rates. Periodic etiologic evaluation of a sample subset of patients with STI syndromes are also recommended (figure 1), to support interpretation of syndromic case reports, inform syndromic treatment guidelines, and monitor evolution of antimicrobial resistance. In Colombia, this will require expanded laboratory capacity to perform routine diagnostic testing for gonorrhoea and chlamydia.
WHO recommends as part of the Global STI strategy the performance of prevalence assessments of gonorrhoea and chlamydia in general populations (such as pregnant women) (figure 1) These surveys, when conducted periodically (e.g. every 2 years) are ideal to assess national STI burden. Colombia has not had any nationally representative gonorrhoea and chlamydia prevalence surveys and national surveys may remain beyond the scope of surveillance capacity. As a feasible option Colombia may consider periodic screening for gonorrhoea and chlamydia within existing health activities, such as in samples of pregnant women in ANC, or in blood donors.
Early and correct diagnosis of STIs is the best way to ensure effective medical treatment and prevent further STI transmission. An evaluation of patient access to, and quality of, diagnosis and treatment for symptoms of STIs in Colombia is needed. The current medical setting may present barriers to the use of structured STI care, with patients resorting to self- treatment through pharmacies without medical evaluation. Expanded laboratory capacity to diagnose gonorrhoea, chlamydia and other STIs that is accessible by general medical providers can reduce inadequate or inappropriate treatment of STI symptoms. Scale-up and use of WHO prequalified rapid point-of-care diagnostics for syphilis screening in pregnant women and high risk populations can expand screening and treatment coverage and reduce treatment delays. Reducing delays and loss-to-follow-up between collecting specimens, laboratory testing, and access to treatment can reduce the risk of transmission and disease sequelae.
These activities can be considered alongside efforts to ensure wide acceptance of prevention interventions, elimination of stigma and discrimination in health care settings, and early availability of prevention and treatment services. Provider interventions including clinical training in STI diagnosis and management as well as interactive supervision of compliance with diagnosis and treatment guidelines should be included to expand clinical personnel capacity to address STIs. Taken together, the above actions and those recommended in the WHO Global STI Strategy will intensify the national STI response in Colombia and ensure progress towards ending sexually trasnsmitted infections while improving health and well-being.