INTRODUCTION
Episiotomy is a surgical procedure performed in order to widen the lower portion of the vagina, the vulvar annulus and the perineal tissue during the expulsion stage of childbirth1. It is one of the most common procedures in obstetrics despite the fact that the current scientific evidence does not support its routine use2-4. There are four techniques for performing episiotomy: midline, mediolateral, lateral and “J” incision5. Historically, it has been used to avoid spontaneous vaginal tears6,7, and to reduce neonatal morbidity and mortality2,8,9. It has also been argued that a controlled surgical incision is generally easier to repair6.
Internationally, there is a trend towards reducing the use of episiotomy and limiting its performance to specific indications10. The restricted use of this procedure in uncomplicated vaginal deliveries compared to the routine use of episiotomy has been associated with a lower risk of perineal trauma and the need for suturing11,12. Performance of episiotomy varies from country to country, with reported figures ranging from 8% to 95%, varying in relation to instrumented delivery, preterm delivery, breach presentation, suspected foetal macrosomy, or impending perineal tear5,11-14. Given the absence of reliable evidence for routine use or beneficial effects, the World Health Organisation (WHO) recommends that frequency of use should not exceed 10%13.
There is a paucity of information regarding the frequency of episiotomy and associated factors at a national4 and regional level15,16. Institutions should be aware of this frequency in order to determine if the procedure is being performed within the standards suggested internationally and to plan quality improvement actions in obstetric services in an attempt at rationalising the use of the procedure. Consequently, the main objective of this research is to determine the frequency with which episiotomy in performed and the associated complications. A second objective is to explore factors associated with episiotomy and describe maternal and neonatal outcomes in the obstetrics service of San Jose University Hospital (HUSJ) in the city of Popayán (Colombia), during the first semester of 2016.
MATERIALS AND METHODS
Design and Population: Descriptive cross-sectional study conducted in pregnant women with vaginal delivery and a gestational age of 37 or more weeks who were seen at HUSJ in the city of Popayán during the first semester of 2016. This general institution provides Level III services and is a referral centre in the Department of Cauca in southwestern Colombia for a population affiliated either to the contributive or the state-subsidised social security system in Colombia. Patients with incomplete clinical record and doctor’s notes, or with a loss of information of more than 10% were excluded. A sample size of 197 patients was calculated using the formula n = P x Q/ (E/Z)², taking into consideration the number of live births delivered in previous years at the institution (1800 deliveries, 900 cesarean sections and 900 vaginal deliveries in 2015), with an expected frequency of episiotomy of 20% (close to the 10% proposed by the WHO)13, and the tolerated margin of error was 5%, with a 95% confidence level.
Procedure. Patients with vaginal delivery and a gestational age of 37 weeks or more determined by early ultrasound of the reliable date of the last menstruation were identified, and simple sampling was performed using a random number list in Microsoft Excel (2013); the investigators obtained the informed consent before starting data collection. The form was then completed based on the institutional clinical record. An Excel database was created using validation rules for entry control in order to ensure data reliability and quality; the analysis was performed using the Stata v.9 software package and this was followed by data encryption.
Measured variables: Maternal age, origin, weight (kg), height (cm) (to estimate body mass index in kg/m2), parity, adequate prenatal care (four or more prenatal visits initiated during the first trimester), gestational age, obstetric maternal pathology (hypertensive disorders of pregnancy, premature membrane rupture, chorioamnionitis, gestational diabetes). Characteristics of the delivery: duration of the expulsion phase and labour in minutes, labour induction, instrumented delivery, presentation, shoulder dystocia, weight of the neonate. Maternal outcome variables included episiotomy, presence of tear, classification of the tear in grades I-IV17, postpartum infection and postpartum bleeding. Neonatal outcome variables included Apgar score at 1, 5 and 10 minutes, meconium-stained amniotic fluid, need for neonatal intensive care unit (NICU) or step-down unit, and presence or absence of acute respiratory distress syndrome (ARDS).
Statistical analysis. In order to determine frequency, the numerator used was the total number of patients in whom episiotomy had been performed, and the denominator was the total number of patients with vaginal delivery who met the inclusion criteria. Baseline sociodemographic and clinical variables are presented comparing the women that underwent episiotomy versus women who did not. Continuous variables are summarised by means of central trend and scatter measurements, and categorical values are presented as proportions. The Shapiro Wilk normality test was used for normality evaluation of continuous variables. Normal distribution variables were compared using Student’s t test, while the Mann-Whitney test was used for variables with a non-normal distribution; categorical variables were compared using the chi square test or Fisher’s test. A bivariate analysis was performed with the established variables. Association was established by means of the prevalence ratio and its respective 95% confidence interval (95% CI). Finally, a logistic regression multivariate analysis was performed in order to determine the association between episiotomy and primiparity, adjusting for potential confounding factors. The stepwise procedure was used with entry and exit probability of 0.20 and 0.05, respectively; moreover, the clinical criterion was also considered besides the statistical criterion for the selection of variables. The analysis of the data obtained was performed using the Stata v. 9 software package.
Ethical considerations. The study as well as the analysis were conducted using the HUSJ database, endorsed by approval minutes No. 10 of November 21, 2015. The women who participated were asked to sign the informed consent, and data confidentiality was guaranteed.
RESULTS
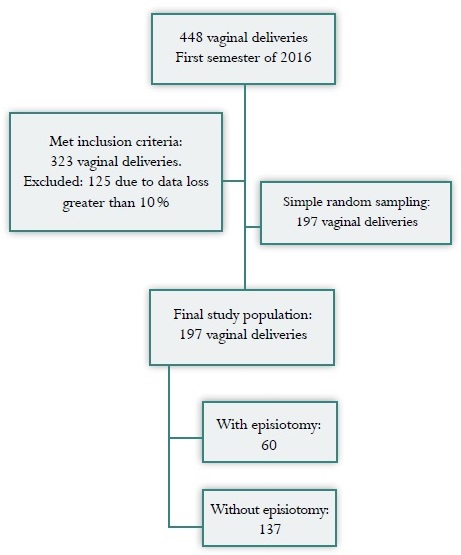
There were 448 patients with vaginal delivery in the time period between January and June 2016; of them, 323 met the inclusion criteria, 125 (39%) were excluded because of data loss of more tan 10% and incomplete documentation in the clinical record. A simple random sample of 197 patients was obtained (Figure 1). Episiotomy was performed in 60 pregnant women, with a frequency of 30.45% (95% CI: 24.1-37.3).
When comparing the patients with and without episiotomy in terms of baseline sociodemographic and clinical characteristics, clinically and statistically significant differences were found for maternal age and parity. Although there were statistical differences in body mass index (BMI), they were not clinically relevant. There were no differences in existing maternal pathology at the time of second stage, or in neonatal birth weight (Table 1). The bivariate analysis of factors associated with the use of episiotomy showed that in nulliparus patients (PR = 8.81; 95% CI: 4.22-18.4) and in patients under 19 years of age (PR = 1.76; 95% CI: 1.14-2.63) the frequency of episiotomy performed by the treating physician was higher. Protective factors were BMI > 25 (PR = 0.51; 95% CI: 0.34-0.77) and age over 34 years (PR = 0.12; 95% CI: 0.01-0.83), with no differences in terms of whether the delivery was induced or spontaneous, instrumented, or the foetal weight was greater than 3999 g (Table 2).
Table 1 Baseline characteristics of patients with vaginal delivery at the San José University Hospital in Popayán (Colombia). 2016
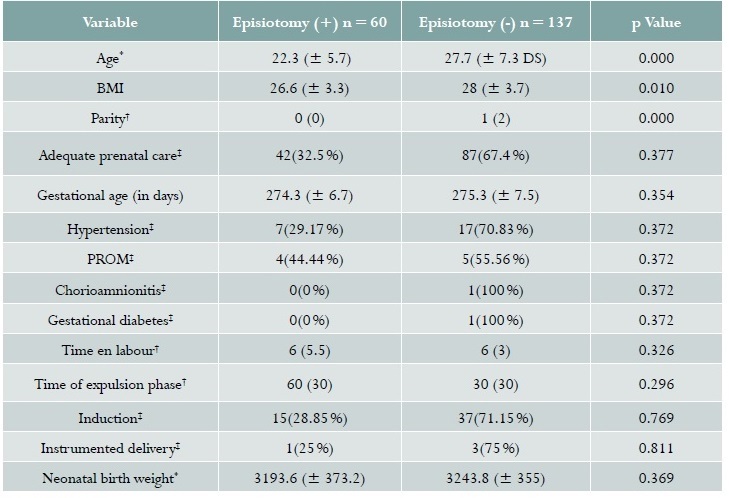
Source: study data. *Student t, †Range test, ‡Chi square
Table 2 Bivariate analysis assessing factors associated with the use of episiotomy at San Jose University Hospital in Popayán (Colombia). 2016
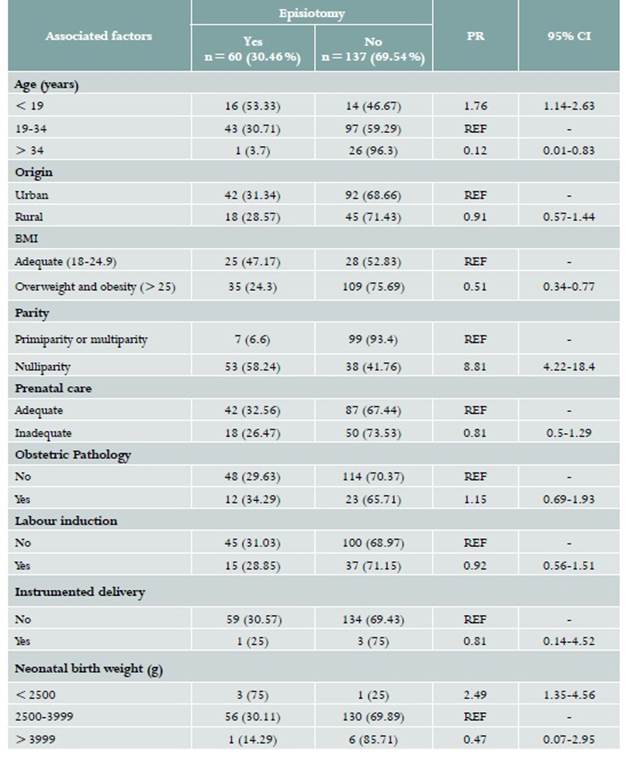
Source: Study data. PR: Prevalence ratio; CI: Conficence interval; REF: Reference; BMI: Body Mass Index
In terms of maternal and perinatal outcomes, it was found that patients with episiotomy had a lower frequency of tears: 3 (5.26%) vs. 54 (39.42%) in patients without episiotomy (PR = 0.12; 95% CI: 0.04-0.39). Of the cases delivered, 28.93% (n = 57) had perineal tears of which 16.75% (n = 33) were Grade I, 11.68% (n = 23) Grade II, 0.51% (n = 1) Grade III, with no cases of Grade IV perineal tears. There were no cases of postpartum infection or haemorrhage. In terms of neonatal outcomes, there were no differences in terms of the presence of meconium-stained amniotic fluid (PR = 0.68; 95% CI: 0.19-2.4), admission to the NICU (PR = 1.59; 95% CI: 0.63-3.99) or respiratory distress syndrome (Table 3).
Table 3 Bivariate analysis assessing maternal and perinatal outcomes associated with the used of episiotomy at San Jose University Hospital in Popayán (Colombia). 2016
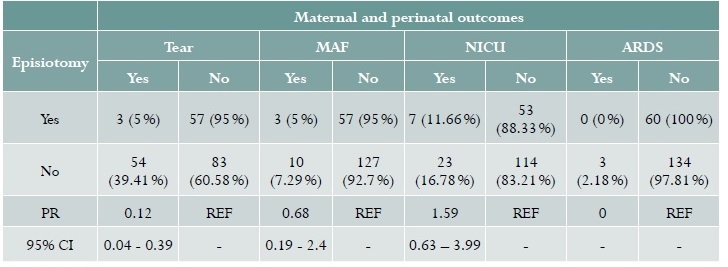
Source: study data. PR: Prevalence ratio; CI: Conficence interval; REF: Reference; MAF: Meconium-stained amniotic fluid. NICU: Neonatal intensive care unit; ARDS: Acute respiratory distress syndrome
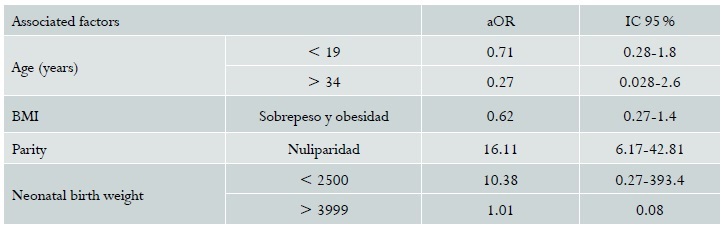
The multivariate analysis was adjusted on the basis of variables considered clinically important from the point of view of obstetrics: foetal weight, maternal age, parity, BMI. Statistical significance was found only for parity (aOR = 16.11; 95% CI: 6.17-42.81) (Table 4). Analysis of the duration of the second stage was not possible because there were no prolonged expulsions.
DISCUSSION
The frequency of episiotomy between the months of January and June 2016 was found to be 30.45%, nulliparity being the main associated factor. The frequency of tears was lower when this procedure was performed.
Regarding the frequency of episiotomy, our results are similar to what was reported by authors like Pérez Valero et al. in a study that found a frequency of 33.5%18, as well as other studies that show frequencies of 29.9% and 29.1% in similar populations and similar restrictive policies15-18; however, other Latin-American studies conducted in similar populations report frequencies ranging between 49% and 61% between 2005 and 2009, at the time in which restrictive policies started to be implemented in order to improve maternal care19-21.
Similar to the findings in our study, Campos Braga et al. found primiparity to be a risk factor (OR = 3.08; 95% CI: 2.16-4.41)20, as was also the case in the study by Trinh et al. (OR = 2.22; 95% CI: 1.48-3.32)17. There was no association with prior maternal pathology, similar to the findings of Trinh et al. that studied hypertensive disorders of pregnancy (OR = 1.04; 95% CI: 0.77-1.36) and diabetes mellitus (OR = 1.04; 95% CI: 0.77-1.36)17. In terms of labour induction, our study did not find an association with episiotomy, contrary to what is described in other studies like the one by Campos Braga et al. where it was reported as a risk factor (OR = 1.92; 95% CI: 1.31-2.79). No association was found with instrumented delivery, in contrast with the latter study which reported a higher risk in patients undergoing instrumented delivery (OR = 18.91; 95% CI: 7.86-45.48). Also, that same study found no association with birth weight > 3999 g (OR = 1.12; 95% CI: 0.37-3.41) similar to the finding in our population20.
Like in our study, Santos Oliveira et al. Reported a higher frequency of tears when episiotomy was not performed (OR = 26.03; 95% CI: 18.13-37.37)21.
The strengths of this study include the representative sample, the range of associated factors analysed, and the management of confounding factors using a multivariate analysis. Limitations include the number of subjects excluded due to incomplete information (39%), the fact that it was carried out in a single Level III institution and cannot be extrapolated to the region, and the fact that obstetrician practices, knowledge and attitude were not evaluated, because these are variables that may influence the decision regarding episiotomy.











 text in
text in