INTRODUCTION
Among the causes of abdominal pain in pregnant women found in the literature, the most common is appendiceal inflammation secondary to infection or acute appendicitis1, with a frequency of 0.4 to 1.4 for every 1000 pregnancies2, accounting for 25% of non-obstetric surgeries during gestation3.
Timely diagnosis is critical to avoid appendiceal perforation; however, pregnancy poses a special challenge in this condition. Although symptoms are similar as in non-pregnant women, characterised by acute abdominal pain arising from the epigastrium or the periumbilical area radiating to the right iliac fossa, usually associated with fever, vomiting and tachycardia, classical clinical signs have been described to be less precise in pregnant women. This is so due to anatomical changes such as uterine growth in the advanced stages of pregnancy, which results in displacement of the omentum, the small intestine and the abdominal wall away from the cecal appendix4. The location of the appendix varies as gestation advances, with a cephalad displacement over McBurney’s point during the first trimester, continuing through to the eighth month of pregnancy when it will be found in the right subcostal region in 80% of the cases5. This displacement may result in delayed diagnosis and increased perforation frequency6.
Appendiceal perforation during pregnancy has been described to be associated with higher maternal morbidity (52% vs. 17% without perforation), and mortality of up to 4%7. On the other hand, it has been found that acute perforated apendicitis induces increased pre-term uterine activity and pre-term delivery8, and foetal mortality occurs in 24% when the appendix is perforated, comared with 7% when there is no perforation9,10 and foetal mortality occurs in 24% of cases in the presence of perforation, compared to 7% when there is no perforation(10).
As mentioned above, the diagnosis of apendicitis during pregnancy poses a challenge for obstetricians, general surgeons and general practitioners. Diagnostic tools such as Magnetic Resonance Imagine (MRI) and ultrasound are now available to help with early diagnosis, but it is important to know the quality of the evidence supporting their use in this population in order to select the best diagnostic aid. The objective of presenting this case of appendicitis during the second half of pregnancy is to review the literature on the diagnostic approach to acute appendicitis in advanced pregnancy, with emphasis on the usefulness of ultrasound and magnetic resonance imaging.
CASE PRESENTATION
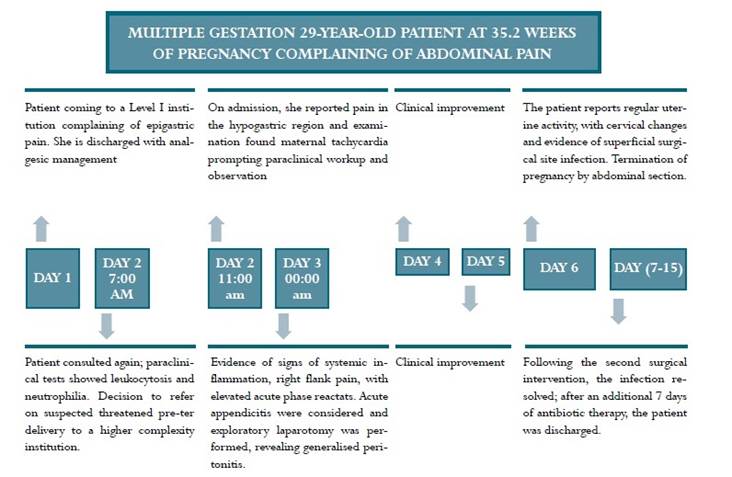
A 29-year-old, single, mestizo race pregnant woman in her 35.2 weeks of gestation based on the date of the last menstruation, was referred to a Level IV hospital in the city of Bogotá (Colombia) from a primary care institution due to a 24-hour clinical picture characterised by epigastric pain which did not respond to the administration of a histamine receptor antagonist. Whole blood count showed leukocytosis and neutrophilia, while urinalysis results were normal. Impending pre-term delivery was considered, prompting the decision to refer the patient (Figure 1). On admission, the patient reported pain in the hypogastric region with no other associated symptoms; the only significant medical history. Obstetric history included two prior uncomplicated pregnancies. Current pregnancy was negative for STORCH (syphilis, toxoplasma, rubella, cytomegalovirus, herpes, hepatitis B), first and second trimester ultrasound scans consistent with the gestational age, the only relevant information being primipaternity.
The initial physical examination found the following values: blood pressure 115/66 mm/Hg, heart rate 97 beats per minute, respiratory rate 18 breaths per minute, temperature 36.5°C, arterial oxygen saturation 95%, as well as pain on palpation over the lower hemiabdomen and evidence of irregular uterine activity. Ligamentous distensión was considered and the patient was placed under observation. Whole blood count showed a result of 15,900 leukocytes/mm3), at the expense of neutrophils, elevated CRP (C-reactive protein), normal liver function, and urinalysis not indicative of infection. After a period of 20 hours, the patient showed clinical signs of systemic inflammatory response with a febrile peak and tachycardia, right flank pain and voluntary abdominal defense. Foetal monitoring showed foetal tachycardia, attributed to maternal fever. Follow-up laboratory tests showed elevated acute phase reactants with persistent CRP elevation and increased leukocytosis. Because of suspected appendicitis the patient was assessed by the general surgery service and exploratory median laparotomy was performed given the possibility of abdominal surgical pathology, with the finding of acute, middle-third perforated appendicitis in gangrenous phase and generalised peritonitis. Appendectomy plus peritoneal lavage were performed, and antibiotic treatment with piperacillin/tazobactam 4.5 mg IV every 6 hours plus metronidazole 500 mg IV every 8 hours was initiated.
Post-operatively there was evidence of increased surgical site erythema and, additionally, the patient reported uterine activity. The gynaecological examination revealed cervical changes, 3 cm dilation with 70% effacement, and foetal monitoring with irregular uterine activity. Reassessment by general surgery found superficial complicated surgical site infection and reintervention was indicated for open surgical wound management; during the procedure, evidence was found of fascial dehiscense, prompting intra-operative assessment by the ObGyn service. Based on the finding of active infection in the abdominal cavity and the risk of maternal sepsis with foetal compromise, it was decided to deliver the foetus during the same surgical time by means of a cesarean section. Both procedures were carried out uneventfully with the result of a live newborn weighing 3340 g, and measuring 48 cm, with a low APGAR score that recovered later. The mother and the baby remained in the hospital until the completion of a 7-day course of antibiotics.
MATERIALS AND METHODS
A search was conducted in the literature in Up to date, Medline via PubMed and Science Direct databases using the MeSH terms “Pregnancy”, “Peritonitis”, “Appendicitis”, “Perforated Appendicitis”, “Ultrasonic Diagnosis”, “Magnetic Resonance Imaging” and “Computed Tomography”. The search included case reports, review of the literature, descriptive retrospective studies, cohorts, and case-control studies published in English or Spanish over the past 20 years focusing on the topic of appendicitis in advanced pregnancy, and those that dealt with the approach to diagnosis. Letters to the editor were excluded.
Ethical considerations. The patient signed the informed consent and gave permission for her case to be published. Information confidentiality and patient privacy were guaranteed.
RESULTS
Overall, 10 titles pertaining to the use of imaging for diagnosis of appendicitis during pregnancy were identified. They included three retrospective cohort studies11-13, five cross-sectional studies14-18, one prospective cohort19, and one review of the literatura20. The studies had been conducted in the United States12-15, Canada17,18, Brazil20, Turkey11, Iran19, and South Korea16.
Ultrasound. In their review of the literature, Franca et al. argue that the diagnostic approach to appendicitis during its initial stages is challenging in pregnant women, particularly during the second and third trimesters. Moreover, they indicate that the first diagnostic test should be ultrasound, and recommend nuclear magnetic resonance when ultrasound results are inconclusive, and they propose the use of computed axial tomography (CT) as a last resort20.
In a retrospective cohort of pregnant and non-pregnant women taken to appendectomy, Aras et al. report that sensitivity and specificity of ultrasound for the diagnosis of appendicitis in a pregnant woman are 61% and 80%, respectively. They suggest a careful assessment in patients with suspected appendicitis in whom ultrasound is reported as inconclusive or normal because, in women in the third trimester of pregnancy, pain may be localised to the right upper quadrant and there is usually a slight leukocyte elevation during this stage of gestation, creating a diagnostic limitation11.
In a prospective cohort study, Kazemini et al. assessed the accuracy of ultrasonography in the diagnosis of acute appendicitis in pregnancy. They studied 58 pregnant women with a mean age of 29.1 years ± 4.94 diagnosed with acute appendicitis histologically confirmed, between January 2014 and January 2016. They report that the greater the gestational age the lower the sensitivity but the higher the specificity, and they report a sensitivity of 63% in the second trimester and 50% in the third trimester, and a specificity of 75% and 100%, respectively, with a positive odds ratio of 2.52 and a negative odds ratio of 0.49 for the second trimester. These authors recommend the use of other imaging studies such as computed tomography or magnetic resonance following an inconclusive ultrasound result19.
Shetty et al. conducted a retrospective cross-sectional study of clinical records over a 5-year period, focusing on diagnostic imaging in patients with clinical suspicion of appendicitis; they correlated imaging findings with patient management and final outcome. A total of 39 patients were referred for diagnostic imaging studies; of them, 35 were assessed with ultrasound and 23 of them were later taken to computed axial tomography, while 4 were taken to CT scan directly without having an ultrasound first. These authors conclude that the method most widely used for diagnosis is ultrasound, with 46.1% sensitivity and 95.4% specificity. Low specificity could be explained because it is often impossible to visualise the appendix14.
Magnetic resonance imaging. In a retrospective study, Theilen et al. assessed the accuracy of magnetic resonance imaging in the diagnosis of appendicitis in 171 pregnant women suspected of having this condition. They report that it was not possible to visualise the appendix in 53, but none of them had appendicitis in the end. Of those patients in whom the diagnosis was a normal appendix, only 1 had appendicitis, and in 18 with a diagnosis of abnormal appendix, 6 had false positive results. Consequently, sensitivity and specificity of NMR were 91% and 95.3%, respectively. The authors also mention that the more advanced the pregnancy is, the lower the rate of visualisation but that, nonetheless, it is better than ultrasound, which did not allow visualisation in 43 out of 46 pregnant women in whom it was performed. Of the three women in whom visualisation was possible, an abnormal appendix was diagnosed in 2 and confirmed only in 1 as well as in the patient considered to have a normal appendix. Of the 43 patients in whom the appendix was not visualised, the diagnosis was made later in 28 using NMR12.
Israel et al., conducted a retrospective cohort study with 33 patients with suspected appendicitis. In 5 patients, appendicitis was confirmed; NMR identified an abnormal appendix in the 4 cases of acute appendicitis; in 13, a normal appendix was diagnosed; in no cases was the diagnosis of appendicitis found in the clinical record; and in 16 cases it was not possible to identify the appendix and one of those cases resulted in chronic appendicitis. Consequently, sensitivity was 80% and specificity was 100%. These authors reported that the appendix could not be identified with ultrasound in 29 patients, a normal appendix was reported in 3 cases, 1 of which was diagnosed as having acute appendicitis in the end. These authors do not report the gestational age at which imaging studies were performed13.
Tsai et al. conducted a retrospective cross-sectional study aimed at determining the degree of inter-radiologist agreement regarding the features of magnetic resonance imaging of the appendix during pregnancy, together with the results associated with an indeterminate interpretation. They studied 233 women with suspected apendicitis during pregnancy between 2003 and 2015, taken to magnetic resonance imaging during that period. Overall, there were 14 patients (6%) positive for acute appendicitis during pregnancy; in 13 of them, NMR was interpreted as abnormal and in 1 patient, it was interpreted as normal. The kappa value for inter-observer agreement was 0.85 - 1; appendicitis was not the final outcome in 73 patients in whom the appendix was not visualised15.
Jung et al. conducted a retrospective cross-sectional study to assess the diagnostic accuracy of NMR in appendicitis. The study included 46 pregnant women who were taken to magnetic resonance imaging because of suspected acute appendicitis, between 2010 and 2016; NMR was shown to have 100% sensitivity and 91% specificity; this imaging modality allowed to categorise appendicitis as probable appendicitis alone, appendicitis associated with another pelvic pathology, and definitive diagnosis of appendicitis. Two of the three cases of false positive results with NMR occurred with the probable diagnosis of appendicitis associated with another pathology16.
In another retrospective cross-sectional study in 42 pregnant patients with suspected appendicitis taken first to ultrasound and then to magnetic resonance between August 2008 and 2015, Patel et al. set out to determine the diagnostic accuracy of the 42 magnetic resonance imaging studies. Overall, 5 patients were diagnosed with acute appendicitis, and 7 appendectomies were performed. Ultrasound did not identify the appendix in any of the patients, whereas it was identified in 22 patients when NMR was used, classifying 6 cases as appendicitis and 16 as normal appendices. There were 20 cases in which the appendix was not visualised and in none of them was appendicitis diagnosed within the next 6 months. Finally, using nuclear magnetic resonance, 3 cases of acute appendicitis were adequately identified, 3 cases were considered false positive, and in 36 appendices classified as normal, 34 were true negative and 2 were false positive, for 60% sensitivity and 92% specificity17.
Burns et al., in a retrospective cross-sectional study, assessed the performance of NMR for the diagnosis of appendicitis during pregnancy in a Canadian institution. The authors reviewed all magnetic resonance images performed between 2006 and 2012 in order to assess pregnant women for suspected appendicitis. A total of 71 magnetic resonance images were reviewed and the appendix was identified in 40 patients (56.3%), for 75% sensitivity and 100% specificity of NMR for the diagnosis of appendicitis in pregnant women18.
CONCLUSIONS
Diagnosing appendicitis during pregnancy is challenging, in particular during the second and third trimesters, because of the cephalad displacement of the appendix. Despite the fact that ultrasound is considered the first choice because of ease and low cost, its sensitivity ranges between 46% and 63%, while its specificity ranges between 85% and 100%. Sensitivity diminishes as gestational age increases, when the appendix is seldom identified. Nuclear magnetic resonance is more expensive and less readily available, and has a sensitivity ranging between 60% and 100%, and a specificity of 91% to 100%. This diagnostic modality would be more useful during the second and the third trimesters of gestation. In the studies included in this review, there were no cases of appendicitis when the appendix was not visualised.











 text in
text in