INTRODUCTION
Hypertensive pregnancy disorders are a group of diseases occurring during pregnancy with a relatively high frequency, involving an imminent risk of maternal health impairment and inadequate fetal development and vitality. These disorders are classified into gestational hypertension, preeclampsia (PE), chronic hypertension and chronic hypertension with superimposed preeclampsia. The incidence of hypertensive disorders ranges between 5 and 10%1. Preeclampsia is the most frequent condition with an incidence of around 2 to 8 %2. It is subdivided into non-severe preeclampsia (NSPE) representing around 60 to 70 % of the cases; severe preeclampsia (SPE) and eclampsia3. Preeclampsia increases maternal and perinatal morbidity and mortality1,2.
The diagnosis of preeclampsia is based on the following criteria: 1) occurrence in women with over 20 weeks of pregnancy, with previously normal blood pressure values and systolic blood pressure levels 140 mm/Hg, or a diastolic blood pressure 90 mm/Hg, measured on two occasions at least 4 hours apart; 2) proteinuria 300 mg in 24 hours, or a protein/creatinine ratio in a urine sample 0.3 mg/dL, or at least one cross present in protein levels measured with reagent strip test. Severe preeclampsia is diagnosed when the systolic blood pressure levels are above or equal to 160 mm/Hg and the diastolic blood pressure levels are above or equal to 110 mm/Hg in two measurements taken at least 4 hours apart, with the patient at rest (except when the hypertensive therapy was initiated before this period of time); or, in the presence of target organ involvement evidenced by: thrombocytopenia (platelets <100.000/mL); renal dysfunction (creatinine >1,1 md/dL or twice the normal serum concentration in the absence of other causes); liver injury (elevated liver enzymes to twice the normal concentration); pulmonary edema or the presence of visual symptoms or brain injury(3). The diagnosis of non-severe PE is established pursuant to the criteria for preeclampsia and in the absence of severity conditions.
The management of preeclampsia depends on the gestational age at the time of diagnosis, on the presence of severity signs and symptoms, and on the health status of the mother and the fetus. In non-severe PE the management may be expectant, which involves: acceptance by the mother after the treating physician explains the risks and benefits of this approach, hospitalization, strict maternal-fetal clinical monitoring, laboratory tests and regular fetal wellbeing tests, and ending of pregnancy at 37 weeks. Discontinuation of expectant management of non-severe preeclampsia is indicated when signs of severe preeclampsia are identified, in the presence of spontaneous labor or premature rupture of membranes, development of placental abruption, oligohydramnios, severe intrauterine growth restriction (IUGR), and altered fetal tests4,5. The identification of SPE is an indication to immediately terminate pregnancy.
Different trials have evaluated the obstetric and perinatal results in pregnant women using expectant management of non-severe PE in order to shed some light on the most appropriate approach to these patients. The HYPITAT I trial compared induction of labor versus expectant management in close to term and term pregnancies, showing no difference in the neonatal results between the two groups6. The HYPITAT II trial compared groups of patients with non-severe hypertensive disorders from week 34 until week 37 of gestation; in the first group, labor was induced, while in the second group, expectant management was used. In the former, the rates of neonatal complications were higher, evidencing the potential advantages of expectant management. Likewise, the trial concluded that the expectant management strategy could be beneficial until a maternal or fetal complication is established7.
When analyzing the maternal complications in expectant management of preeclampsia, the occurrence of severe hypertension has been described in 10-15 % of the cases, eclampsia in 0.2-0.5 %, HELLP syndrome in 1-2 %, placental abruption in 0.5-2 %, and pulmonary edema in less than 1 % of the population4,8. Since PE is the primary cause of maternal morbidity and mortality in Colombia, it is important to describe the clinical course and the prognosis of non-severe preeclampsia at the local level. Therefore, the objective of this study is to describe the incidence of maternal and perinatal complications in pregnant mothers with NSPE subject to expectant management as the initial approach.
MATERIALS AND METHODS
Design and population. Historical cohort of pregnant women with a diagnosis of non-severe PE with single pregnancies between weeks 20 1/7 days and 36 6/7 days, receiving care at the obstetrics unit of the “Hernando Moncaleano Perdomo” University Hospital of Neiva, a referral public institution serving patients in the contributory insurance and in the government subsidized insurance coverage of the Colombian social security system, from June 1st, 2015 to May 31st, 2016. The patients received hospitalized expectant management and the patients remained hospitalized until the end of pregnancy.
The diagnostic criteria for NSPE are: pregnancy beyond 20 weeks with previously normal blood pressure values and systolic blood pressure between 140 and 159 mm/Hg or diastolic blood pressure between 90 to 109 mm/Hg, measured on two separate occasions at least 4 hours apart; proteinuria³ 300 mg in 24 hours or protein/creatinine in a urine sample³ 0.3 mg/dL, or at least one cross of proteins in urinalysis reagent strips; no target organ involvement.
Patients with a diagnosis of multiple pregnancy, congenital anomalies, and medical comorbidities such as chronic high blood pressure, diabetes and autoimmune diseases were excluded. A convenient non-probabilistic sampling was conducted in all patients presenting with non-severe PE.
Procedure. A search was conducted of all patients admitted to the institution with one of the ICD-10 diagnosis associated with hypertensive disorders (O120, O121, O122, O13X, O140, O141, O149, O150, O151, O159 y O16X). Subsequently, we looked for the medical records of patients with these diagnoses and the inclusion and exclusion criteria were verified. Then, the socio-demographic and the clinical information was collected in a suitable instrument. The information was collected at the time of admission to the institution and according to the variables evaluated with regards to the search of potential maternal and fetal adverse outcomes until the end of pregnancy. Likewise, the medical records of the neonates until discharge or for the first seven days in the case of hospitalized newborns were reviewed. To estimate the incidence ratio, the information on live births at the institution during the observation period was considered; this information was provided by the department of epidemiology of the “Hernando Moncaleano Perdomo” University Hospital of Neiva, based upon the institutional records (RUAF-ND) (Sole registry of affiliates - births and deaths) of live birth certificates.
The following variables were considered: sociodemographic: mother’s age, place of origin, race and social security system; clinical maternal data: body mass index (BMI), blood pressure (BP) at the time of diagnosing the non-severe preeclampsia and at the end of gestation, gestational age at the time of diagnosis of the NSPE; laboratory tests: proteinuria, creatinine, platelets, lactic dehydrogenase, transaminases (at the time of diagnosis of the NSPE and at the end of gestation). The time elapsed between the initial NSPE diagnosis and the end of pregnancy.
The maternal outcomes measured included: development of severe preeclampsia, eclampsia, HELLP syndrome, placental abruption, posterior, reversible encephalopathy syndrome, cerebrovascular accident, and maternal death; these variables were followed until hospital discharge. The perinatal results to consider were: Neonatal Intensive Care Unit admission (NICU), low birth weight, IUGR, low Apgar score at 5 minutes and perinatal death (death between 22 weeks of gestation or 500 g of weight, and death during the first 7 days after birth).
Statistical Analysis. The absolute and relative frequencies were analyzed for the qualitative variables and calculation of the central tendency and dispersion measurements for quantitative variables.
The general cumulative incidence ratio of NSPE was estimated for the observation period and according to the gestational age at term (37 to 40 weeks 6 days) and pre-term (less than 37 weeks), based on the following formulas:
- General accrued incidence ratio of non-severe PE = Total number of non-severe PE cases / Total number of live births over the period.
- Specific accrued incidence of NSPE in term pregnancies = Total number of cases of NSPE with end of pregnancy at term / total number of live births in full-term pregnancies.
- Specific accrued incidence of NSPE in preterm gestations = Total number of NSPE cases with pre-term delivery / Total number of live births in preterm gestations.
The frequency of maternal, fetal, and perinatal complications in the cohort of women with NSPE was also measured. The information was analyzed using Excel 2010 software and Epidat 3.1.
Ethical considerations. The study was approved by the Committee of Medical Ethics of the University Hospital “Hernando Moncaleano Perdomo” of Neiva, Colombia.
RESULTS
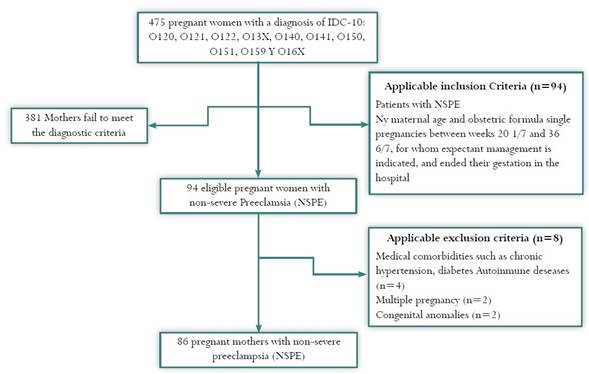
475 pregnant women were identified with IDC-10 diagnoses associated with hypertensive disorders of pregnancy. The review of the medical records identified 86 patients that met the inclusion/exclusion criteria (figure 1), 42 were preterm pregnancies and 44 were term pregnancies.
The total number of live births at the University Hospital over the study period was 2,932, of which 2,568 (8.6 %) were term gestations and 364 (12.4 %) were pre-term infants. The overall accrued incidence (pregnant women with NSPE/live births) was 3.03 % (89/2932), the term incidence was 1.7 % (44/2568), and the pre-term incidence was 11.5 % (42/364).
The pregnant women with identified with NSPE had a mean age of 27 years, (standard deviation SD ± 8.1 years). Most of the patients studied (39.5 %) were in their first pregnancy, while 16.3 % were multiparous (4 or more pregnancies). In terms of personal history of the disease, 60.5 % of the patients had no history of preeclampsia. The mean gestational age at the time of diagnosis was 33.6 weeks (SD ± 3.1 weeks). 62.8 % of the patients were beyond 34 weeks at the time of diagnosis, and considered as late onset preeclampsia. One patient (1.2 %) in our study group was from an indigenous ethnic group and came from the Municipality of Iquira; she presented with a crisis of hypertension, was admitted to the obstetric ICU and the baby had to be admitted to the NICU (table 1). The clinical variables at admission and discharge of the patients studied are shown on Table 2.
Table 1 Socio-demographic characteristics at admission of pregnant women with non-severe preeclampsia at the “Hernando Moncaleano Perdomo” University Hospital of Neiva, Colombia, 2015-2016

Table 2 Clinical and paraclinical variables at time of admission to the hospital and at the end of gestation in women diagnosed with non-severe preeclampsia at the “Hernando Moncaleano Perdomo” University Hospital, Neiva, Colombia, 2015-2016.
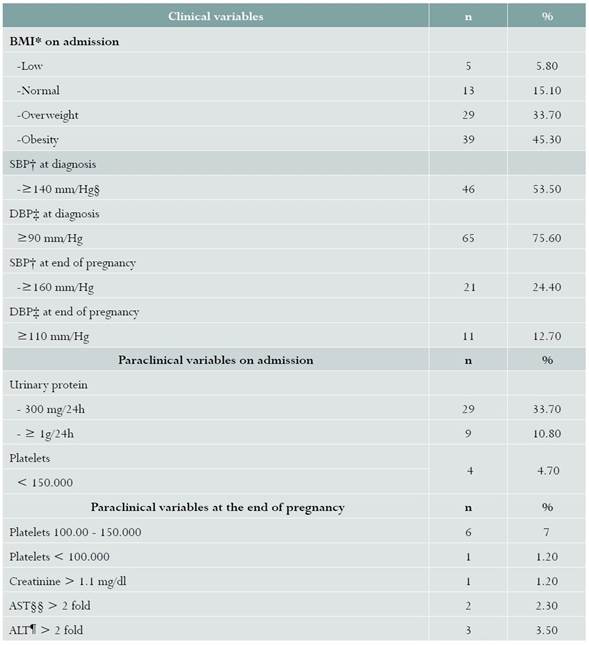
* Body Mass Index; † Systolic blood pressure; ‡ Diastolic blood pressure; § Mm of mercury; §§ aspartate aminotransferase; ¶ alanine aminotransferase.
44 patients (51.2%) were delivered at term (37 weeks or more of gestation); in 34 patients (39.5 %) the pregnancy ended between 34 and 36.6 weeks, and in 8 patients (9.3 %) the pregnancies ended before 34 weeks. The mean gestational age at the end of pregnancy was 36.1 weeks (SD ± 12 days).
Most of the patients underwent cesarean section (79.1 %) and 18 patients (20.9 %) had normal vaginal deliveries, none requiring instrumentation. The average time from admission to delivery was 17 days (SD ± 21 days); in 39/86 (45.4 %) the latency period was less than 7 days; in 22/86 (25.6 %) from 8 to 14 days; in 5/86 (5.8 %) from 15 to 21; from 22 to 28 days in 4.7 %, and in 16/86 (18.6 %) patients the pregnancy was extended for more than 28 days.
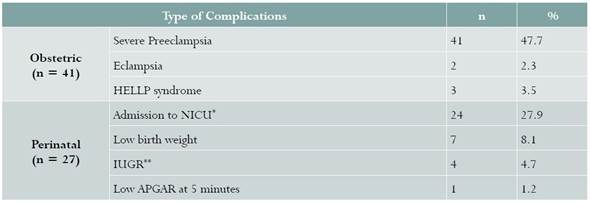
With regards to maternal complications, SPE was present in 41 pregnant women (48 %); in 24 (58.5%) of them during the first 7 days, in 19.5 % (8/41) between 8 to 21 days, and more than 3 weeks in 9 of the 41 patients (22%). The major causes of SPE were: hypertensive crisis in 27 of 41 patients (65.9 %), eclampsia in 2 (2.4 %), premonitory symptoms of eclampsia in 13 patients (31 %), HELLP syndrome in 3 (3.5 %), liver involvement in 5 patients (14.6 %), renal involvement and thrombocytopenia in 2 patients (2,4 %). There were no cases of placental abruption, reversible posterior encephalopathy syndrome, cerebrovascular accident or maternal death.
Perinatal results were characterized by a high percentage of normal weight for gestational age neonates (90.7 %), Apgar > 7 at 5 minutes (98.8 %).
Adverse results were observed in 27 pregnant women (31 %); 24 neonates required ICU admission, and the majority - 17 patients - were due to weight below 2,500 g. 4 patients (4.8%) were diagnosed with IUGR, and 3 of them (3.5 %) were diagnosed before 34 weeks. There were no fetal or perinatal deaths.
Two of the patients with IUGR and the patient with an Apgar score below 7 at 5 minutes, required ICU admission; one patient with low birth weight and two patients with IUGR were not admitted to the ICU (table 3).
DISCUSSION
Our study found a 3% incidence of NSPE, which is consistent with the literature2, with progression to severe preeclampsia in almost half of the patients (47.7 %); development of severe hypertension in 22.1 %, other complications such as eclampsia in 2.3 %, and HELLP syndrome in 3.5 %. These last results on complications differ from those reported by Briones et al.9 and Muñoz et al.10 that reported HELLP syndrome or renal injury as the most frequent complication in preeclampsia in general.
In contrast, Sibai found even lower frequencies of severe hypertension (10 to 15 %), eclampsia (0.2 to 0.5 %), and HELLP syndrome (1 a 2 %)8.
The absence of maternal and perinatal mortality was also described in the Netherlands trial HYPITAT6. Our perinatal results were similar to those reported by Pauli4, and exhibited lower rates of severe neonatal complications as compared to the figures reported by Carmona11.
The absolute number of cases with NSPE in term and pre-term gestations was similar; however, the specific accumulated incidence of NSPE for preterm gestations was almost 7-fold higher than the accumulated incidence specifically for term gestations; this highlights the importance of preeclampsia, and in this case of non-severe PE as a factor associated with an increased probability of a pre-term delivery, as described in previous studies10,12.
Among the limitations of the trial, it is important to note its retrospective nature and the sample selection based on IDC-10 codes, that could lead to selection and information biases. Furthermore, based on the characteristics of preeclampsia, an initial misclassification of the NSPE diagnosis may have occurred, considering that 51% of the patients that presented SPE developed the condition over the first week.
CONCLUSIONS
A 3% incidence of no-severe preeclampsia was observed and a frequency of maternal complications in about 50% or the pregnant mothers, all associated with the development of severe preeclampsia and, to a lesser extent, perinatal complications in about one third of the mothers. In average, patients diagnosed with NSPE at our institution, deliver two weeks after being diagnosed. A strict control of the patients presenting with NSPE and expectant management is required.











 text in
text in