At present, carcinosarcoma (CS) is considered by the World Health Organisation (WHO) as a mixed tumour with an epithelial histologic component (carcinomatous) and a mesenchymal component (sarcomatous), although at first it was considered a sarcoma1. Carcinosarcomas mostly arise in the corpus of the uterus, less frequently in the ovaries, and exceptionally in the cervix2,3. Preliminary studies suggest that this neoplasm is a subtype of metaplastic carcinoma, based on biological behaviour, lymph node spread pattern and clonality testing4. It has been proposed that, when located in the cervix, these tumouts should be classified, according to their origin, as malignant mixed mesonephric tumours or malignant mixed Müllerian tumours2. Therefore, cervical carcinosarcoma is considered to be a different entity from carcinosarcoma of the uterine corpus.
Despite screening programs, cervical cancer is the fourth most frequent form of cancer worldwide, with close to 528,000 new cases every year5. However, it is the primary cause of cancer-associated mortality in Colombia, and the second in frequency, with an incidence of approximately 18.7 cases for every 100,000 women, continuing to be a public health problem6. The predominant histological type is squamous cell carcinoma, followed by adenocarcinoma5,6, much more predominant than primary sarcomas and carcinosarcomas, which account for only 1 and 0.4% of cases, respectively7.
Multiple risk factors for the development of carcinosarcoma have been documented, including obesity, advanced age, exposure to exogenous oestrogens or radiation, prior chemotherapy, risky sexual behaviour, the presence of other sexually transmitted infections and, of course, human papilloma virus (HPV) infection8,9. Mean age of onset of these tumours is 65 years.
Regarding clinical manifestations of cervical carcinosarcoma, the most frequent signs and symptoms are abnormal uterine haemorrhage, pelvic pain, dyspareunia, polypoid or papillary cervical mass, or large mass replacing the cervix. In advanced stages, patients present with weight loss and symptoms associated with the obstructive effect of the tumour on the gastrointestinal or urinary tracts10.
In terms of the pathology of the carcinosarcoma, the surface of the section is usually fleshy with haemorrhagic areas, necrosis and cystic changes; microscopically, it has epithelial and sarcomatous components11. In the corpus uteri, the epithelial component may be Müllerian, with squamous cell or basaloid elements or elements that mimic basal adenoid carcinoma, or mesonephric elements such as mesonephric adenocarcinoma; mesenchymal components may be homologous (of the uterus itself) such as stromal sarcoma or leiomyosarcoma; or heterologous (not of the uterus) such as chondrosarcoma, osteosarcoma and rabdomyosarcoma12. Differential diagnosis includes differentiated and undifferentiated carcinomas and metaplastic squamous cell or sarcomatoid carcinoma. Immunohistochemistry studies help with the identification of the two components and of heterologous mesenchymal elements12. This tumour spreads through the lymphatics and metastases are usually of the epithelial component. The most common sites for metastasis are the pelvic and para-aortic lymph nodes, peritoneum and the lungs13. Unfortunately, at the time of diagnosis and onset of symptoms, this neoplasm has usually already involved the lymphatic system, which might explain in part its worse prognosis when compared to the squamous cell subtype or adenocarcinomas(7). There is no consensus at the present time regarding the best therapeutic option for the treatment of this entity4,10.
Because of its aggressive behaviour and the low frequency of the disease, it is critical that gynaecology experts as well as gynaecologic oncologists recognise this variety of carcinosarcoma as a cervical neoplasia and follow an appropriate workup based on a high index of suspicion, instituting timely treatment of this condition in order to reduce associated morbidity and mortality.
The objective of this case report presentation of a patient with cervical CS is to review the available literature, emphasising treatment and prognosis of this disease condition.
CASE REPORT
Female patient, 84 years old, widow and housewife of mestizo ethnicity, living in Bogota, referred to the National University Hospital, a high complexity referral centre in Bogotá, Capital District, serving patients affiliated to the contributive regime of the Colombian social security system. The patient had a clinical picture lasting 15 days of dysuria, pollakiuria and vesical tenesmus which progressed to urinary obstruction requiring catheterisation. The patient did not report any relevant medical history. Surgical history included cystopexy and cholecystectomy eight years before. Obstetric and gynaeological history: gravida 4, para 4, cesarean section 1, menopause at 35 years of age, no family planning. On admission to the hospital, she reported involuntary weight loss over the previous 6 months, no genital bleeding or other symptoms.
On physical examination, the patient was found to be alert, oriented, haemodinamically stable, free from abdominal pain, and with evidence of a large solid hypogastric mass, approximately 12 cm in size, over the pubic area. Genital examination found evidence of atrophic external genitalia, and the vaginal examination revealed a large mass causing important bulging of the anterior and left-lateral cul-de-sac, hindering identification of the cervix and the performance of speculoscopy.
On admission, complete blood count results were the following: haemoglobin, 12.3 g/L; leukocytes, 7200/mm3; neutrophils, 64%; platelets, 252,000/mm3; creatinine, 1.24 mg/dL; BUN, 22 mg/dL; sodium, 142 mEq/L; potassium, 4.19 mEq/L; chlorine, 108 mEq/L; glucose, 94 mg/dL; prothrombin time, 19 sec; partial thromboplastin time, 28.6 sec. Glomerular filtration rate was 30 ml/min/1.73 m2.
Ultrasound performed in an other institution showed a pelvic mass probably arising from the left ovary. CA125, alpha fetoprotein and carcinoembryonic antigen tumour markers were all negative. Non-contrast magnetic resonance was performed because of the finding of renal failure, with the following results: grade III bilateral, pelvic mass 13 x 10 cm in size apparently arising from the cervix, with areas of cystic degeneration, bleeding foci and diffusion restriction areas given the presence of a linear capsule, apparently sparing neighbouring visceral structures, which might correspond to a benign lesion. However, the finding of bleeding foci inside the tumour and diffusion restricted areas, as well as the presence of hydronephrosis, preclude the possibility of ruling out an underlying malignant lesion invading the pelvic wall. It was initially interpreted as probable myoma with degeneration vs. cervical malignant tumour (Figure 1).
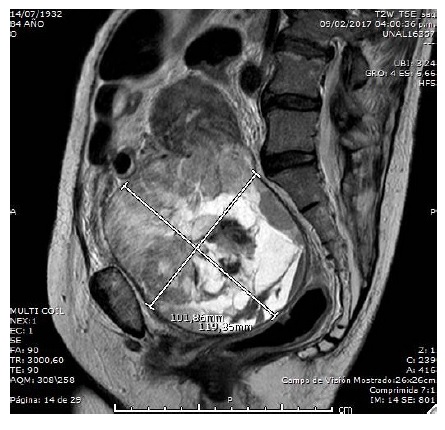
Figure 1 Abdominopelvic nuclear magnetic resonance in a patient with cervical carcinosarcoma; 11 cm, round-shaped mass with well-defined edges, arising from the uterine cervix
Forty-eight hours after admission, the patient presented anuria with significant secondary elevation of nitrogen compounds, hyperkalemia and severe anaemia, and a drop of 6 g in haemoglobin in relation to the baseline test. On examination, the patient was alert, with unaltered vital signs, distended abdomen, mild abdominal pain, without peritoneal irritation. Laboratory tests showed creatinine at 3.13 mg/dL and BUN 61 mg/dL, and it was considered that the patient was in acute renal failure secondary to obstruction. Two units of red blood cells were transfused, fluid resuscitation was initiated and the patient was taken to interventional radiology for urinary tract diversion. The patient responded poorly to the management instituted, leading to the suspicion of intra-abdominal bleeding from the tumour and the decision to perform emergency laparotomy, with the finding of 1500 of haemoperitoneum, a 6 cm corpus uteri, ovaries and tubes of usual appearance and a large irregular mass arising from the posterior and lateral wall of the cervix and occupying the entire pelvic cavity with extension into the middle and upper thirds of the vagina, of cerebroid appearance, haemorrhagic, approximately 13 cm in diameter, and adherent to the deep planes. No evidence of adenomegaly was found. Total abdominal hysterectomy was performed together with salpyngoophorectomy and bilateral ligation of the hypogastric arteries due to poor control of bleeding requiring pelvic floor packing, which was achieve by means of inflation of a Foley catheter balloon with 100 cc of saline solution, pulled through the dome of the vagina with a 1000 cc fluid bag for final intraoperative control of bleeding. Transfusion with 6 units of packed red blood cells was administered and the patient was transferred to the ICU for postoperative care. In the first 12 hours, bleeding (300 cc) persisted through the vaginal dome, requiring an interventional radiology procedure. Embolisation of the hypogastric arteries was possible through the ligation of the left hypogastric artery which had 2 mm of patent lumen. Bleeding was controlled and the Foley catheter was removed from the vaginal dome 24 hours later.
Following the intervention, the patient evolved satisfactorily, renal failure resolved by the fourth day, nephrostomies were closed, and the patient was discharged on postoperative day 10 with a management plan and follow-up by oncology.
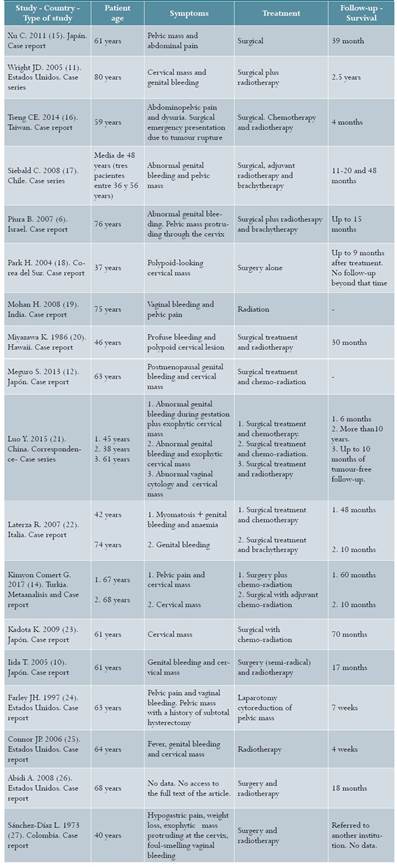
Anatomic pathology revealed a 8 x 7 x 4.5 cm mass located in the cervix associated with great deformity of the posterior wall, with parametrial and marginal involvement (Figure 2). Histologically, it was consistent with a biphasic malignant tumour composed of a small-cell epithelial component with areas of glandular and squamous differentiation and some areas of basaloid appearance and others with corneal bead formations; and an undifferentiated mesenchymal component consisting of fusiform cells with inconspicuous cytoplasm in a mixoidlooking matrix. Immunohistochemistry showed immunoreactivity for AE1-AE3 and cytokeratin 7 in the epithelial component, and no reactivity for synaptophysin or chromogranin, with neuroendocrine differentiation exclusion. Cell proliferation index determination with Ki67 was close to 100% in the epithelial component and close to 80% in the mesenchymal component, with p63 and cytokeratin 5/6 in the epithelial component (Figure 3). These findings were interpreted as cervical CS with a poorly differentiated high grade carcinoma component and a homologous undifferentiated mesenchymal component, with extension to the intramural portion of the isthmus through the entire cervical thickness, parametria and section margins. Endometrium, myometrium and adnexal organs were negative for the tumour. Stage IIIB.

Figure 2 Gross appearance of cervical carcinosarcoma. Tumour localised to the posterolateral region of the cervix, with parametrial extension and large necrotic areas and areas of mixoid appearance
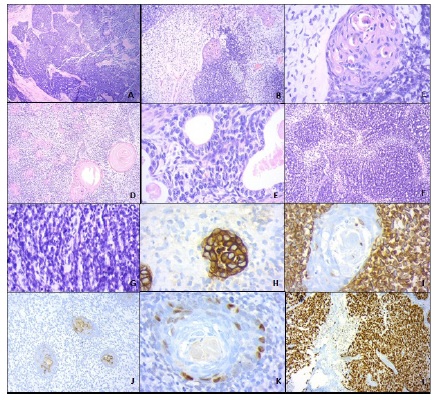
Figure 3 A: H&E 4X, small-cell component of the cervical carcinosarcoma; B: H&E 10X, mesenchymal component with mixoid matrix and epithelial component with transition from undifferentiated area to small squamous differentiation nodule, enhanced in C (H&E 40X); D (H&E,4X): squamous beads in a background of undifferentiated mesenchymal component; E (H&E40x): epithelial component with glandular differentiation; F and G (H&E, 4x and 10x, respectively): undifferentiated mesenchymal component with great mitotic activity; H (cytokeratin AE1-AE3, 40x): membrane marking in the epithelial component; I (vimentin, 40X), reactivity in the mensenchymal component; J and K (cytokeratin 5/6, 10x and p63, 40x): showing marking in the squamous cell component; L (ki 67, 10x): showing nearly 100% immunoreactivity in the undifferentiated epithelial component.
The patient was contacted 6 months after surgery and the family reported that she was receiving radiotherapy treatment and was scheduled for chemotherapy.
MATERIALS AND METHODS
A search of the literature was conducted in the Medline via PubMed, SciELO and Ovid databases, using the terms “uterine carcinosarcoma”, “cancer treatment”, “treatment-review” and “outcomes” in Spanish and “uterine carcinosarcoma”, “treatment”, “cancer treatment”, “treatment review” and “treatment outcome” in English. The search was limited to articles published in English and Spanish on the topic of treatment and prognosis of uterine cervix carcinosarcoma. Reports, case series, meta- analysis, topic reviews, clinical practice guidelines and reference books were included. Studies for which no access to the full text were excluded.
Selection was done by title and abstract. Data taken from the selected articles included study or article identification, age, symptoms, treatment and follow-up.
Ethical considerations. Informed consent in writing was obtained from the patient for the publication of the clinical case, the photograph of the tumour, and the pathology slides. The necessary precautions were taken to guarantee information confidentiality and patient anonymity.
RESULTS
Once duplicate literature was eliminated, 706 references were reviewed by title and abstract and, of them, 19 met the inclusion and exclusion criteria. Most of the references were case reports and only one was a systematic review of cervical carcinosarcoma14. A systematic review was also found about treatment of carcinosarcoma of the uterine corpus13; however, there are histologic differences between these two entities and it is not known whether treatment may be the same. Table 1 shows the studies included in this review.
Table 1 Review of the literature. Summary of articles of clinical cases of patients diagnosed with cervical carcinosarcoma, 2017
Treatment. In the case reports reviewed, 24 patients ranging between 36 and 80 years of age were identified6,10,14-27. The treatment used in those cases were surgery followed by radiotherapy in 11 patients6,10,11,17,20-22,26,27; surgery plus chemotherapy and radiotherapy in 6 cases12,14,16,21,23; surgery plus chemotherapy in 2 cases21,22; surgery alone in 3 cases15,18,24; and radiotherapy in 2 cases19,25. Kimyon Comert et al. conducted a review of case series and case reports, rated as low quality by Amstar (only one database included, no removal of duplicate data, and no consideration of the risk of bias). It included 81 subjects with carcinosarcoma and reported that in patients with advanced disease, the authors recommend cytoreduction surgery to remove all macroscopic disease14. Kadota23 and Laterza22 report on the use of radiotherapy because they consider that it can reduce locoregional recurrences. In a narrative review on the treatment of carcinosarcoma of the uterine corpus, Menczer presents several combined chemotherapy regimens that are affective as adjuvant treatment, such as cisplatin/ifosfamide, ifosfamide/placlitaxel and paclitaxel/carboplatin13; however, it is worth restating that it is not clear whether cervical carcinosarcoma is the same as uterine CS, and this management might not be appropriate for cervical neoplasia.
Prognosis. Survival in women with cervical sarcoma is lower than in women with squamous cell carcinoma or adenocarcinoma, compared by stages.
In patients with stage IB tumours, 5-year survival is only 67%7. It has been found that, in average, 2-year survival is 50%, although it varies depending on stage, age and cell differentiation3. Surgery followed by adjuvant radiotherapy, with or without chemotherapy, is associated with improved disease free survival and overall survival14. The studies included in this review found that survival varied between 4 weeks and 10 years. However, survival in the majority of cases was less than three years (Table 1). Pathological factors associated with survival and disease recurrence include depth of myometrial invasion, lymph node involvement, adnexal and serosal extension, positive tumour cityology, and residual tumour volume13,28,29.
CONCLUSION
Cervical carcinosarcoma is an infrequent entity whose most common clinical manifestation is genital bleeding accompanied by a pelvic mass. Surgery, radiotherapy and chemotherapy are among the therapeutic options for the treatment of this disease condition. However, regardless of the treatment provided, survival and freedom of disease appear to be short. Studies of high methodological quality are needed in order to assess the safety and effectiveness of the different interventions for the therapeutic approach to this disease.











 texto em
texto em 


