INTRODUCTION
In the past decade, suicide, defined as the act of ending one’s own life, has been declared as a public health problem. According to the World Health Organisation (WHO), one death due to this cause occurs every 40 seconds in the world1. In Colombia, attempted suicide rates increased progressively between 2009 and 20152, and 2016 was the year with the highest suicide rate of the past decade, at 5.2 for every 100,000 inhabitants, and 85.1% of the women who committed suicide were of childbearing age3. The latest report shows a rate of 6.47 for Antioquia, higher than the rate for the rest of the country, and for the women, a rate of 2.44 for every 100,000 inhabitants. However, there are not data regarding pregnancy-related suicide. The majority of suicide deaths are avoidable, considering that many of the suicidal individuals mention their desire to die4. If this happens during pregnancy or the postpartum period, it may be considered as another potentially preventable cause of maternal mortality.
The United Kingdom report on maternal mortality, “Saving Lives, Improving Mothers’ Care“, reported 101 suicide deaths during pregnancy and up to 1 year after childbirth between 2009 and 20135, while the figure reported for 2006-2008 was 29 suicide deaths during pregnancy and up to 6 months after childbirth6. As key points, the report highlighted the high risk of severe mental disorders during the postpartum period, failure to recognise the symptoms, and the rapid onset and progression of the symptoms. In 2012, the maternal mortality review committee of New Zealand reported that, between 2006 and 2010, suicide accounted for 25% of all maternal deaths (13 cases), 54% of them during pregnancy and 46% during the postpartum period, and 46% were classified as preventable7. In 2016, the Colombian Maternal Mortality Surveillance and Control Protocol reported that suicide was the fourth cause of mortality in pregnant women in 20058. These findings have meant that pregnancy-related suicide is no longer an invisible issue. There is a greater association between pregnancy-related homicide and suicide than with many obstetric complications, placing violent death among the main causes of pregnancy-related mortality9.
Not much is known about mortality due to suicide during pregnancy and the postpartum period. Few articles are retrieved as a result of the search in the literature, and they offer conflicting information, with very little consolidated statistics. An example of this is the lack of consensus regarding the classification: the WHO classifies it as direct maternal death10, the United Kingdom includes it among psychiatric causes of death, classifying it as indirect maternal death(5). In Colombia there are some figures regarding the size of the problem, but little is known about its characterisation and determining factors. This knowledge is required as input for decision-making and for designing public policies and interventions, as set forth in the Public Health Surveillance Protocol for maternal mortality8.
Consequently, the objective of this study was to characterise the population of women who died due to pregnancy-related suicide in Antioquia between 2004 and 2014, in order to help position suicide as a relevant cause of maternal mortality and estimate the proportion of suicide deaths.
MATERIALS AND METHODS
Design and population. Descriptive study of suicide deaths during pregnancy, delivery and up to 6 months after childbirth in women living in Antioquia, identified between 2004 and 2014. Cases of suicide death entered in the Public Health Surveillance System (SIVIGILA) were included. Also included were those cases which, after having been identified in the database of deaths of women between 10 and 54 years of age as suspected maternal deaths occurring during pregnancy or up to 6 months after childbirth, were confirmed as suicide based on the information taken from the clinical records and in-hospital care documentation. Consecutive sampling of all the deaths with the described characteristics was made.
Antioquia is the sixth largest department in Colombia, with an estimated population of 6.5 million inhabitants. During the time period between 2004 and 2014 there were 476 maternal deaths, 309 direct (64.9%), 142 indirect (29.8%), and 25 due to unknown cause (5.3%)11; the mortality ratio during those years varied between 67.9 and 30.4 for every 100,000 live births.
Procedure. The process of identifying the cases and collecting the data was part of the official maternal mortality surveillance carried out by the Health and Social Protection Secretariat of the Department as part of the work of public health surveillance, following the guidelines established by the National Health Institute (INS). The NACER research group of Antioquia University acted as the operator during the entire study period, working with a multidisciplinary team consisting of professionals in information systems, specialists in obstetrics, several of them epidemiologists and public health specialists, always under the oversight of the Health Secretariat and the National Health Institute.
For the identification of the cases, a search was conducted in the SIVIGILA database of all cases reported by the local health directorates, the state social enterprises and the health institutions of the different municipalities, INS Code 550 for “maternal mortality” which includes reports of late and pregnancy-related maternal deaths. The search was also conducted in the database of deaths of women between 10 and 54 years of age to look for suspected unreported cases of maternal deaths, identifying cases that had a “YES” in boxes 37 to 39 of Chapter III of the death certificate which refer to deaths of women in childbearing age, or cases with absent information for those same variables.
Suicide cases were identified mainly from pregnancy-related deaths and in the death certificate databases, given that the ICD-10 definition of maternal death, which excludes accidental or incidental deaths such as suicide, was the definition in place throughout the study period. Although it was only in 2012 that the WHO recognized suicide until postpartum day 42 as a cause of direct maternal death12, the Health Secretariat of Antioquia actively searches and analyses these events since that time, even if they were not included in the maternal mortality ratio13.
After checking for compliance with the definition of the event or suspected event, the institutions where the deceased women received care were asked to provide the clinical record. Family members were interviewed whenever possible. Clinical records, autopsy reports, death certificates and interviews with family members were included as sources of information. The latter were the only sources of information in those cases in which the women had not received medical care. Data were entered in a form especially designed for that purpose, including the case number and the sociodemographic and clinical information of each of the women, and they were lated tabulated in a database for anonymous analysis.
Measured Variables. Sociodemographic: ethnicity was assigned based on the information entered in box 18 of the Death Certificate of the Ministry of Social Protection/National Statistics Department (DANE); the level of education was categorised as complete or incomplete primary, incomplete or complete secondary, technical/technological and higher education; the place of residence was categorised as the subregion of the Department where the town of residence over the past 6 months was located; the area of residence as rural or urban; the affiliation regime was categorised as contributive, subsidised or not insured; occupation included being a student. Clinical variables: maternal age in years at the time of death by age groups (10 to 19, 20 to 29 and 30 to 39); time of death was categorised according to the trimester of gestation (first trimester up to 13 weeks + 6 days, second trimester from 14 to 27 weeks + 6 days, and third trimester from 28 weeks until the end of pregnancy); postpartum, immediate postpartum to day 42, and 43 days to 6 months after childbirth; the number of previous pregnancies and living children; the number of prenatal visits until the time of death. The methods for committing suicide were considered: hanging, fall, poisoning, firearm and drowning, according to the entry in the clinical record or the information gathered during the visit to the home; the place of death depending on whether it occurred in a healthcare institution or at home.
Personal or family history related to the risk of suicide most frequently found in the relevant publications was taken into consideration: mental disorder, use of psychoactive substances, attempted suicide, family history of suicide, family violence and intimate partner violence. The clinical record was used to determine if there was a history of personal mental disorder diagnosed by a healthcare professional, corresponding to cases identified by the International Classification of Diseases (ICD - 10) as organic mental disorders (codes F00-F09), mental and behavioural disorders due to psychotropic substance abuse (F10-F19), schizophrenia, schizotypical disorders and delirium disorders (F20-F29), mood disorders (F30-F39), neurotic disorders secondary to stressful situations and somatoform disorders (F40-F49), behaviour disorders associated with physiological dysfunction and somatic factors (F50-F59), adult personality and behaviour disorders (F60-F69), mental retardation mental (F70-F79), psychological development disorders (F80-F89), behavioural and emotional disorders usually originating in childhood and adolescence (F90-F98)14.
Statistical analysis. Categorical variables were grouped according to their frequency in terms of percentages; medians and inter-quartile ranges were calculated for continuous variables. The proportion of suicide deaths was calculated over the total number of maternal deaths that occurred in the Department during the study period. The specific mortality ratio was calculated by age groups, taking into consideration the number of deaths identified as part of the identification by age group and the total number of live births reported by DANE for the 11-year period, expressed as number of maternal deaths/1000 live births.
Ethical considerations. The research study was approved by the Bioethics Committee of the School of Medicine of Universidad de Antioquia, and the Health and Social Protection Secretariat of Antioquia approved the use of the data and the publication. Privacy and confidentiality of all the information were guaranteed
RESULTS
During the period described, 24 confirmed suicide deaths were identified in women during pregnancy and during the first 6 months after childbirth, for a proportion of 4.8%. No sociodemographic or clinical information was available for the description of 6 cases and some information was available for the 18 remaining cases, although not all the exact same data were obtained for all of them. Verbal autopsy reports were available for 10 cases and in the remaining cases, the information was taken only from the clinical records.
One of the women was of indigenous ethnicity, none of the others belonged to special groups, or there was no information in that regard. In terms of education, 93.4% of the women had less than complete secondary education. For 77.8% of cases there was no information about religion. Table 1 shows other sociodemographic characteristics. Of the 18 women with information, the time of death was unknown in 1 case. Of the remaining 17, four died in the first trimester (23.6%), five during the second trimester (29.4%), three in the third trimester (17.6%) and five after postpartum day 42 (29.4%). There were no cases in the immediate or near postpartum period.
Table 1 Sociodemographic characteristics, suicide-related maternal mortality, Antioquia, 2004-2014
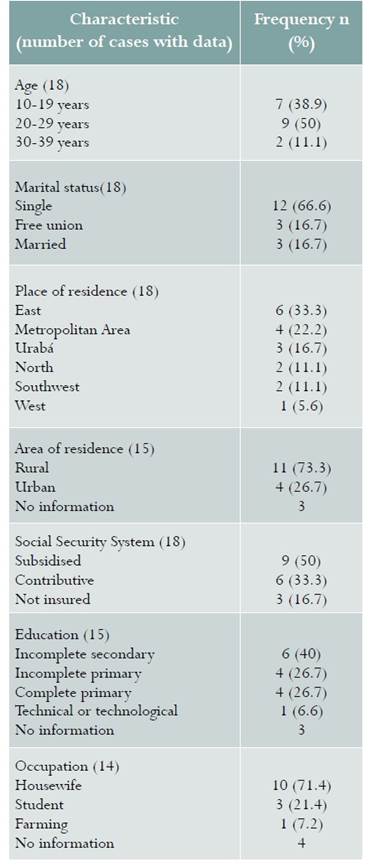
Note. Percentages are presented over the total number of cases for which information was obtained (in parenthesis after the characteristic)
Medians for previous pregnancies and living children were 2 and 1, respectively. At least 1 prenatal visit had been attended in 50% of cases (8/16), and there was no information in 2 cases. In the age group of women between 10 and 19 years there were 7 cases of pregnancy-related suicides and 237,547 live births, for a risk of 1 out of every 33,935 births; in the group between 20 and 29 years of age there were 9 suicides and 469,158 births, for a risk of 1 out of every 52,129; and in the group between 30 and 39 years of age, there were 2 cases of suicide out of 201,427 births, for a risk of 1 out of every 100,714.
The method used for committing suicide was poisoning in 70.6% (12/17) and hanging in 29.4% (5/17); there were no data available in one case; 61.1% died in a healthcare institution (11/18) and 38.9% died at home (7/18).
No information was found on risk factors for suicide, personal in 44.4% (8/18) or family in 72.2% (13/18). Of the 10 women for whom personal or family risk factors were obtained, five had at least one. One woman had a personal history of attempted suicide and a family history of mental disorder; the second woman had a personal history of mental disorder, attempted suicide, family violence, intimate partner violence and a family history of attempted suicides; the third had a personal history of mental disorder, drug abuse and attempted suicide; and the last two only had a personal history of mental disorder. Three of the four women with a mental disorder had a mood disorder; in two of them, the family and the healthcare institution had knowledge of the diagnosis, and the patients had received treatment (pharmacological in one of them and pharmacological plus psychotherapy in the second woman), but none of the three was under treatment at the time of death, and two of them had attended 6 and 8 prenatal visits.
DISCUSSION
Over the 11 years of the study, the cumulative number of pregnancy-related suicide deaths (n=24) was greater than the number of deaths due to obstetric sepsis (n=11), which was classified as the fifth cause of direct maternal death15. It has been previously described that suicide-related maternal mortality is greater than mortality due to other direct obstetric causes9. Authors who claim that the frequency of pregnancy-related suicide is not different16, or that it is lower than in the general female population17,18, recognise that it is a common pregnancy-related death and may play a more significant role than some direct obstetric causes, something that has been confirmed by our findings.
Our results (4.8%) are similar to those described for suicide as a cause of death during pregnancy and the first postpartum year, which have been reported to account for 5-20% of maternal deaths in low and intermediate income countries19. Now, if only the 12 cases that occurred during pregnancy and up to 42 postpartum days are considered, it could be said that at least 2.5% of maternal deaths in the Department during the study period would be associated with suicide. In 2014, a systematic review found that Latin America was the region with the highest incidence of suicide-related maternal deaths, with an estimated proportion of 1% for low and medium income countries. However, the authors recognise that this figure might not represent the true proportion, arguing that with appropriate classification and reporting, the proportion would turn out to be higher20. Multiple barriers may contribute to this under-recording, including differences in study methodologies, non-inclusion in official statistics, variability in the definition, and a tendency to combine suicide deaths with deaths from unknown cause17,18. On the other hand, there is a lack of documentation and follow-up of events: in our study, we failed to find the minimum necessary records for 6 out of the 24 cases identified, and in the remaining ones, information was not uniformly recorded, resulting in the absence of the same type of data for all cases.
In our study, a greater number of suicide deaths were identified in women between 20 and 29 years of age, with less than complete secondary education, single, students or housewives, living in rural areas and belonging to the subsidised regime in the social security system. In Colombia, in 2016, the highest number of suicide deaths in women occurred in the age group between 15 and 17 years, followed by the group between 20 and 24 years, with rates of 5.6 and 2.7 suicides for every 100,000 inhabitants, respectively, predominantly in women with less than complete secondary education (75.4%), the majority with no partner (63.8%) and asphyxia generators as the main causal mechanism, followed by poisoning3. According to the most recent data of maternal mortality in the United Kingdom, the mean age of women who died due to suicide was 29 years5, and in contrast with our finding, the majority were married (76%) or had a stable partner6, similar to what other studies have found(19). In a different study in Colombia, Palladino et al., had already reported a similar finding to ours regarding marital status9.
In this research, 70% of the cases assessed were death due to poisoning and 30% death by hanging. Several studies have found that poisoning is the most common method employed by women, even during pregnancy21,22, a finding that has been associated with ease of access. There were no cases during the postpartum period before 42 days, unlike what has been reported by other authors23. In our study, only half of the patients had attended prenatal visits and in those cases which had received prenatal care, an important lack of timeliness for appropriate care was identified. As highlighted by multiple studies on maternal mortality in the world, the presence of a psychiatric disorder is the main risk factor for suicide24 and it is an indicator of high postpartum risk, even more so if it is a mood, bipolar or schizophrenic disorder5,25. The limitations detected in our study have also been reported by other authors in that mental disease is seldom detected during the perinatal period in women who commit suicide and, when it is, it is usually treated suboptimally19,26.
This is the first study focused on the identification and analysis of pregnancy-related suicide deaths in Colombia. A thorough search and review of the literature were conducted trying to include grey literature that would allow to gain adequate insight into the current situation of this event. One of the weaknesses of our study is that, given that it was only after the implementation of the Maternal Mortality Surveillance Protocol of the National Health Institute in 2011 that mandatory reporting of suicide deaths was included, a thorough search of cases was not conducted before that year and, consequently, it is not possible to claim that all the cases that occurred during the period were actually included. Interviews (verbal autopsies) were available only for 10 cases, although they were not specific for suicide deaths but generic for maternal mortality. Regarding information on risk factors in the clinical records, it is not possible to determine whether the questions were asked but the information was not documented, or if the information was simply not gathered. However, this finding reinforces the invisibility of the problem.
Based on the findings in the literature and the information that confirms them, there is a need to actively look for the symptoms, signs and related risk factors in order to identify vulnerable patients and implement prevention or active treatment measures. Compliance with the guidelines needs to be improved in order to reinforce care for these women and ensure adequate follow-up even up to one year after childbirth. Collaborative work with the maternal mortality surveillance committee is required in order to obtain more reliable information, and instruments designed to collect standardised and truly relevant information need to be developed.
CONCLUSION
Pregnancy-related suicide death is an important and potentially preventable cause of maternal mortality, even more frequent than other direct causes. Greater knowledge of the issue is required, as well as greater commitment in terms of documentation, notification, follow-up and analysis of the events.











 text in
text in 


