INTRODUCTION
Maternal mortality (MM) is a healthcare problem which also serves as a measure of the health status in a community. In the world, the maternal mortality ratio (MMR) has dropped from 385 deaths for every 100,000 live births (1990) to 216 for every 100, 000 live births 1; in developing countries, this ratio is 239, while it is 12 for every 100,000 live births in developed countries 2. In Perú, MMR dropped from 298 deaths for every 100,000 live births in 1990, to 68 for every 100,000 in 2015 3, pointing to some degree of improvement in maternal mortality; nonetheless, the MMR continues to be high when compared to maternal mortality reported in developed countries 4.
The fifth Millenium Development Goal referred to maternal health and established the goal of reducing maternal mortality by three-fourths between 1990 and 2015, a goal that was met 5. The majority of these deaths are due to preventable complications. There are several social determinants of health 6 associated with maternal mortality (MM), including economic, education, geographic, and cultural factors, as well as the healthcare system in charge of providing care before, during and after childbirth 7. It is reasonable to take into account the importance of access to health services and their quality, as well as their resolution capability for women at risk of MM, in order to ensure recognition of the signs and symptoms of alarm during pregnancy 8.
The World Health Organization (WHO) stated that women living in poverty have a lower probability of receiving adequate healthcare from qualified professionals, and that only close to one-third of pregnant women attend four or more prenatal visits, receive professional healthcare during delivery, or receive postnatal care, circumstances that contribute to the increase in maternal mortality ratios 2. Over the past decade, the percentage of prenatal care received by Peruvian women at a national level has increased to 97.5%, while institutional delivery has increased to 93.0% 9. Of pregnant women in urban areas, 97.7% delivered in an institution, although the MMR continues to be higher than reported in developed countries 2.
The General Epidemiology Directorate of the Peruvian Ministry of Health reports that the regions with the highest MM are Lima, La Libertad, Loreto, Piura and Cajamarca 10, the main direct causes being hemorrhage, pregnancy-induced hypertension and abortion. The majority of maternal deaths occur in remote and poor rural areas, reflecting, among other things, the social inequities and exclusions of a country. However, many maternal deaths are found to occur in the cities and in healthcare institutions with specialized centers for childbirth, greater resolution capability and high prenatal care coverage 11.
The region of Callao, adjacent to Lima, the Peruvian capital, is essentially urban. Callao is one of the Regional Health Directorates (Diresas) with well-implemented epidemiological surveillance of maternal mortality. It uses an epidemiological record that includes several personal, obstetric, gestational, prenatal, delivery and postpartum aspects, apart from data on the healthcare institution; it also quantifies Maine time delays and conducts verbal autopsy of MM cases. Maternal mortality cases in Callao continue to be reported in public and private hospitals and maternal care centers that provide care 24 hours a day; most of the cases are related to a direct cause 10. Given proximity to Lima, the capital, these healthcare institutions have state-of-the-art technology for diagnosis, as well as healthcare staff with the necessary qualifications to solve obstetric emergencies and provide perinatal maternal care.
Several activities have been implemented with the aim of reducing maternal mortality, including the reduction of undesired pregnancy by strengthening family planning promotion activities 12; increase in the number of prenatal visits both in the urban as well as the rural areas 9, thus contributing to an improved identification of pregnant women at a higher risk and with signs of alarm, in order to improvement management of pregnancy, delivery and postpartum complications; implementation of vertical childbirth in healthcare institutions, allowing the woman to choose the birthing position with the support of the couple or another family member 13, which has increased the number of women seeking institutional delivery 9; and education intervention, enhancing women’s empowerment to ascertain their rights 14. However, maternal deaths are still reported in the rural and urban areas alike, as is the case even in Callao, where hospitals and specialized personnel are available 10. This outlook requires a more indepth analysis of the causes of MM in the urban areas, including some of the characteristics of prenatal care, childbirth, estimated time delays described by Deborah Maine 15, and the causes of maternal death 16, in order to propose focused strategies and actions aimed at reducing MM, taking into consideration the context or setting in which these deaths occur. Therefore, the objective of the study was to identify the causes of maternal mortality in the Callao region between 2000 and 2015.
MATERIALS AND METHODS
Design and population
Case series study based on a review of the clinical and epidemiological records on MM in the region of Callao. MM cases were reported by the hospitals and maternal care centers of the public sector (Ministry of Health) that serve pregnant women who are not affiliated to the Social Security System in Health (Essalud), as well as by the Essalud hospitals that serve pregnant women insured under the worker’s contributive system. MM cases occurring in the region between 2000 and 2015 were included. The cases of non-obstetric MM and those for which a clinical record was not available were excluded. Consecutive sampling was used.
Procedure
Maternal mortality cases were identified in the maternal mortality surveillance registry kept by the Epidemiology Office of the Callao Health Regional Directorate. Once the cases were identified, clinical records and Maternal Death Epidemiological Investigation records of the cases occurring during the study time period were reviewed. It is important to note that the Callao Diresa Epidemiology Office is the custodian of the MM files, which consist of the clinical record, the MM epidemiological record, the analyses of the Maternal and Perinatal Death Prevention Committees at a local and department level, and the qualitative MM report carried out pursuant to the Peruvian regulations 14. An ad hoc record validated by expert judgement and tested in a pilot study was used. Information regarding delays in care was estimated by the Callao Diresa staff who conducted the epidemiological investigation of MM cases, which were entered in the MM Surveillance Epidemiological Investigation. Data processing was performed after data collection from the clinical/ epidemiological records and following completion of the quality control process.
Definition of variables
In accordance with the WHO, maternal mortality was classified as the death of a woman during pregnancy, childbirth or within 42 days of delivery, due to a cause related or aggravated by pregnancy or pregnancy care, but not due to accidental or incidental causes 9. Direct obstetric MM was defined as the result of an obstetric complication of the gravid condition (pregnancy, childbirth or puerperium), interventions, omissions, incorrect treatments, or a chain of events originating from these circumstances 2. Indirect obstetric MM is defined as the result of a pre-existing condition or a disease arising during pregnancy, childbirth or puerperium and not due to direct obstetric causes, but which was aggravated by the physiological effects of pregnancy 17. Maternal deaths were grouped in accordance with the International Classification of Diseases (ICD-10) 17.
Moreover, measurements included sociodemographic characteristics (age, occupation, level of education, marital status, prenatal care information (prenatal care, number of prenatal visits, person doing the follow-up), childbirth plan, home visit and signs of alarm written in the perinatal card. The cause of MM was taken from the clinical/epidemiological record which states the basic cause of death, month, year and classification in accordance with the Epidemiological Surveillance protocols of the Peruvian Ministry of Health 14. Mean time delays described by Deborah Maine were estimated (delay in recognizing the problem, delay in deciding to seek help, and delay in receiving adequate treatment) 15.
Statistical analysis
A database was built in SPSS v.22, and the relevant quality control was carried out. Data normality was assessed using the Kolmogorov Smirnov test, the age variable was recategorized as adolescent (10 to 19 years), young (20 to 29 years) and adult (30 to 49 yers), and percent frequencies and means were then calculated.
RESULTS
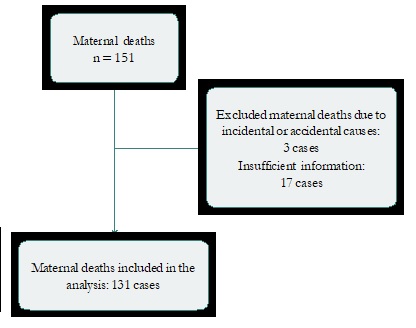
Out of a total of 151 records of deaths during pregnancy, childbirth or puerperium, 131 MM cases which met the inclusion criteria were included, while 3 cases of incidental deaths (asphyxia, motor vehicle accidents) were excluded, as well as 17 cases of MM because of the absence of clinical/ epidemiological records (Figure 1).
In terms of the main sociodemographic characteristics, it was found that, of the 131 study cases, 49.6% [65/131] of the women who died were adults, 19.1% (25/131) had a low level of schooling, 51.9% [68/131] were housewives, and 68.7% [90/131] were married or in a de facto relationship. Table 1 illustrates the sociodemographic characteristics in detail.
Table 1 Distribution of sociodemographic variables of maternal deaths, Callao Diresa*, Perú, 2000-2015
| Characteristics | n = 131 | % |
|---|---|---|
| Age | ||
| Adolescent | 12 | 9,2 |
| Young adult | 52 | 39,7 |
| Adult | 65 | 49,6 |
| No data | 2 | 1,5 |
| Education level | ||
| Illiterate | 1 | 0,8 |
| Primary | 24 | 18,3 |
| Secondary | 60 | 45,8 |
| Higher | 31 | 23,7 |
| No data | 15 | 11,5 |
| Occupation | ||
| Student | 10 | 7,6 |
| Housewife | 68 | 51,9 |
| Employed | 19 | 14,5 |
| Self-employed | 7 | 5,3 |
| House maid | 2 | 1,5 |
| No data | 25 | 19,1 |
| Marital status | ||
| Single | 31 | 23,7 |
| Married/de facto relationship | 90 | 68,7 |
| Widow/divorced/separated | 2 | 1,5 |
| No data | 8 | 6,1 |
* Diresa: Dirección Regional de Salud.
Of the total number of women who died, 58.8% [77/131] attended at least one prenatal visit. In terms of prenatal care, 63.6% [49/77] attended 4 or more visits, 26.0% [20/77] had a prenatal card with written information on the signs of alarm that occurred during pregnancy (inadequate weight gain, anemia, short inter-pregnancy interval, excess pregnancy-related vomiting, etc.). Home visits did not take place for 93.5% of the pregnant women. Table 2 shows the distribution of other characteristics of prenatal care. Of the total number of pregnant women studied, 57.3% [75/131] recognized the risk. In 23.7% [31/131] of cases, the women themselves decided to seek help, in 16.8% [22/131] the search for help was initiated by the family, in 9.2% [12/131] it the partner made the decision; no data are available for the remaining percentage of women. Median time between the onset of discomfort and the decision to seek care was 20 minutes; median time between the decision to seek care and arrival at the health-care institution was 20 minutes; and median time between arrival at the institution and receiving care was 7 minutes. Of the women who died, 69.4% [93/131] were admitted to the hospital.
Table 2 Distribution of prenatal care characteristics of maternal death cases. Callao Diresa*, Perú, 2000-2015
| Prenatal care characteristics | n = 77 | % |
|---|---|---|
| Number of prenatal visits | ||
| < 1 to 3 | 28 | 36,4 |
| 4 and more | 49 | 63,6 |
| Prenatal care site | ||
| Level I | 37 | 48,1 |
| Level II | 11 | 14,3 |
| Level III | 17 | 22,1 |
| Clinic | 1 | 1,3 |
| Other | 2 | 2,6 |
| No data | 9 | 11,7 |
| Home visit | ||
| Yes | 8 | 10,4 |
| No | 69 | 89,6 |
| Humber of home visits | ||
| None | 72 | 93,5 |
| One | 3 | 3,9 |
| Two | 1 | 1,3 |
| Three | 1 | 1,3 |
| Signs of alarm written in card | ||
| Yes | 20 | 26,0 |
| No | 57 | 74,0 |
* Diresa: Dirección Regional de Salud.
According to the type of obstetric cause of MM, 61.1% [80/131] were direct causes and 38.9% [51/131] were indirect. Among maternal deaths due to direct causes, 32.8% [43/131] were due to hypertensive disorders of pregnancy, 12.2% [16/131] to obstetric bleeding, and 10.7% [16/131] were associated with abortion. Of the total number of abortions, 38.9% received care in a Level II healthcare institution, while 38.9% received care in a Level III institution; 50.0% of the abortion cases were managed by gynecologists, one-third presented with bleeding, and 27.8% had infection. Among indirect causes, 16.8% were due to other conditions (systemic lupus erythematosus, fatty liver, aneurysm, thromboembolism, hemolytic anemia, intestinal bleeding, acute pancreatitis, among others), 15.3% were due to infectious diseases (tuberculosis, HIV, pneumonia, bronchopneumonia, AH1N1, brucellosis, disseminated strongyloidiasis, among others), and 6.9% were tumor processes. Table 3 illustrates all cause MM.
Table 3 Distribution of obstetric causes of maternal death. Callao Diresa*, Perú, 2000-2015
| Cause of maternal death | Nº = 131 | % |
|---|---|---|
| Hypertensive disorders of pregnancy | 43 | 32,8 |
| Obstetric hemorrhage | 16 | 12,2 |
| Abortion | 14 | 10,7 |
| Pregnancy-related infection | 2 | 1,5 |
| Ectopic pregnancy | 2 | 1,5 |
| Molar pregnancy | 2 | 1,5 |
| Other obstetric complications | 1 | 0,8 |
| Indirect | ||
| Other conditions | 22 | 16,8 |
| Infectious diseases | 20 | 15,3 |
| Tumors | 9 | 6,9 |
* Diresa: Dirección Regional de Salud.
Of the total number of deaths, 48.1% [63/131] occurred in healthcare institutions of the Ministry of Health, 43.5% [57/131] in Essalud institutions and 0.8% [1/131] in Armed Forces institutions. The majority of maternal deaths occurred in Level III care institutions [86.1%], followed by Level II [6.9%], and Level I [3.1%]. According to the timing of death, the vast majority of MM cases occurred during the postpartum period [68.7%], followed by gestation [24.4%], abortion [3.8%], childbirth [2.3%], and the time was unknown in 0.8% of cases. Two cases of MM [1.5%] occurred in the home. No autopsy data were found in any of the clinical records for the total number of MM cases.
DISCUSSION
This study reports that direct MM is the most important in the Callao region of Peru, with pregnancy-associated hypertension and bleeding being the primary causes. In terms of indirect mortality, morbidity prior to pregnancy and non-obstetric infections were the most frequent causes. The delays analysis showed that time intervals were 20 minutes at the most.
Our results show that the causes of MM are consistent with the national distribution of maternal deaths 18, pointing to a higher percentage of MM from direct causes and a lower percentage due to indirect causes 8. However, the percentage of MM due to direct causes is much lower than the one reported at a national level and in La Libertad region in northern Peru, where 81.9% of the cases of maternal deaths were due to direct causes 19,20. Compared to other international reports of direct MM, our result was higher than the figure of 57% reported for Baja California (Mexico) 21, lower than 82.5% reported in Puebla (Mexico), and similar to the figures of the Mexican Social Security which ranged between 50% and 63% 22.
The distribution of the most frequently reported direct causes in our study is similar to that reported for La Libertad in northern Peru 20 and for the entire country 19, and even for cases of MM in Mexican women in the Social Security 22, a situation which is not dissimilar to the rest of the world 23. Abortion is the third most frequent direct cause in Callao, lower than observed in Ica 24 and Tacna 19, similar to the report for all of Peru 19, and lower than the finding in Chile 25. Our results are consistent with the world landscape, where abortion ranges between 7% and 9% 23 in the developed world 23, developing countries 23 and Latin America and the Caribbean 23. The conditions in which abortion is performed, and the people who perform it, in particular unsafe abortion, could influence the occurrence of maternal deaths in the Ica and Tacna regions 26. It is worth mentioning that abortion in Peru is penalized and this results in a paucity of hospital records because most of the cases are documented as bleeding or infection 8. Women who decide to interrupt their pregnancy seek clandestine places where care is provided under precarious conditions by people who may not be specialized, increasing the risk of maternal death. Tarqui-Mamani 26 reported a prevalence of approximately 15% of attempted pregnancy interruption in Callao.
The level of indirect causes found in the study is higher than the national level reported in 2012 and 2015 18,19 and much higher than the one reported in Argentina 27, where a marked increase in MM was reported in 2009 due to respiratory infections, in particular the H1N1 influenza pandemic 27. Additionally, MM due to influenza virus was also higher on that same year in Mexico 28. Close to 9% of maternal deaths occurred in adolescents, only somewhat lower than the figure of MM reported in Chile 29.
It comes as a reason for concern that little more than 40% of the pregnant women did not receive prenatal care, resulting in a risk factor for MM. Our figure of prenatal care is lower than the one reported for Peru 19, but higher than the one reported in a national hospital in Puebla 30 and in Baja California in Mexico 21. It would be convenient to analyze prenatal care quality and content. Some studies show that pregnant women who develop any complication during pregnancy arrive at the healthcare institution already in a critical condition 31, or seek help in low complexity Level I health services which are unprepared for addressing obstetric emergencies 32.
Our results pertaining to delays are different from those reported for La Libertad (northern Peru) which reflect a big delay in the decision to seek help, and between the decision and arrival at the healthcare institution (ranging between 1 and more than 10 hours), with time to receiving care being less than 10 minutes 20. This situation could be explained by the fact that Callao is fully urban area with good accessibility to maternal centers with 24-hour service, referral hospitals with the necessary capabilities and specialized human resources. Mortality could be explained by the fact that pregnant women arrive at the healthcare institution in a critical condition and, even though there are no delays, the management of the obstetric emergency may be insufficient despite care being provided within 10 minutes. In Peru, regulations require that high-risk pregnant women receive care from specialists in obstetrics and gynecology, and be referred on timely basis and to adequate care institutions in the event they present with complications 14. The limitations of the study include potential selection bias due to non-inclusion of 11.6% of maternal deaths, as well as measurement bias given that the source of information consisted of clinical and epidemiological records of the cases available at Callao Diresa. On the other hand, the time of residence in the Callao region was not considered, which means that some pregnant women coming from other places in Lima or the provinces may have been included as MM recorded and notified by the Callao Diresa, resulting in frequency overestimation; however, it is important to consider that MM under-recording in Callao is 24.2%, discretely higher than the figure for national under-recording 19. The study design does not permit generalization of the results at a national level, but it provides information to identify the causes of MM in the region of Callao, and may be useful to guide public policy for MM reduction in the region.











 text in
text in