INTRODUCTION
Vaginal cuff dehiscence is defined as cuff separation or rupture of of the vaginal or peritoneal incision following a hysterectomy procedure. 1 It may or may not be accompanied by evisceration, where the intraperitoneal content is expelled through the defect until it protrudes through the vaginal introitus. 2 It constitutes one of the surgical emergencies in gynecology due to the risk of bowel perforation, necrosis and secondary sepsis. 3
The reported incidence of vaginal cuff dehiscence ranges between 0.03 and 4.1% in women taken to hysterectomy. 1,4,5 This variability could be due to under-reporting or to technologies that increase risk. 6
Transvaginal evisceration due to vaginal cuff dehiscence was reported for the first time in 1864 by Hyernaux. 7 Its incidence ranges between 0.32 8 and 1.2%. This higher frequency has been associated with robotic hysterectomy. 9
Several factors associated with the risk of vaginal cuff dehiscence have been identified, mainly those related to advanced age, increased abdominal pressure and impaired healing secondary to malignant conditions, radiotherapy, chronic steroid use, malnutrition, anemia and immunosuppression. 6,10 Obese patients have more complications and they also have other comorbidities such as arterial hypertension and diabetes, further increasing the risk. 11 Other factors found to be associated with vaginal cuff compromise are multiparity, menopause, smoking, constipation, chronic cough, hypothyroidism and surgical site infection or hematoma. 1-3
Vaginal cuff dehiscence may occur spontaneously with no triggering factor. However, in premenopausal women, the most frequent trigger is resumption of intercourse before the cuff is fully healed. 1-3 In postmenopausal women, the triggering event is increased intra-abdominal pressure, 3,10 associated with pelvic prolapse or previous vaginal surgery. 8 Post-hysterectomy dehiscence has been fund to be associated with a poor surgical technique, cuff hematoma or infection. 12 In terms of risk factors for evisceration, the most important of all is cuff dehiscence. 12
Transvaginal evisceration is considered a surgical emergency requiring management by a gynecologist as soon as possible after making a prompt diagnosis. The objective of this article is to report the case of a patient presenting with acute abdomen due to small bowel evisceration secondary to vaginal vault dehiscence following total abdominal hysterectomy, and to review the literature on diagnosis and treatment of this condition.
CASE PRESENTATION
A clinical case is presented of a 48-year-old patient who came to the emergency service at Hospital Universitario de Santander (Santander University Hospital) located in the city of Bucaramanga, a high-complexity public referral center in northeastern Colombia that serves population under state-subsidized healthcare coverage provided by the General Social Security system. The patient complained of a painful mass protruding through the vagina and concomitant generalized abdominal pain, predominantly of hypogastric location, and multiple episodes of gastric content vomiting.
The patient reported a surgical history of total abdominal hysterectomy and cystopexy 11 months before due to a benign condition, followed by anterior and posterior vaginal repair 5 months later. Regarding gynecological history, the patient reported menarche at 15 years of age with regular cycles and the date of the last menstruation 2 years before the event; 2 pregnancies, 2 eutocic deliveries of babies weighing 3000 and 2700 grams; last delivery 15 years before; never used contraception and had not had intercourse during the past 6 years; had never been screened for cervical cancer.
On physical examination at the time of admission, the patient was found to be in poor general condition, in pain and diaphoretic; blood pressure 115/70 mm/Hg, heart rate 80 beats per minute, respiratory rate 80 breaths per minute, 95% saturation in ambient air and temperature 36°C. Clinical findings included dry oral mucosa, distended abdomen, absent bowel sounds, hypogastric tenderness on palpation, with no signs of peritoneal irritation. Vaginal inspection revealed evisceration consisting of a loop of bowel with no haustra or taeniae, or apparent signs of ischemia, that cannot be reduced spontaneously or manually (Figure 1). No paraclinical tests were performed on admission and immediate surgical management was indicated due to suspected bowel obstruction secondary to transvaginal evisceration through a vaginal cuff defect.
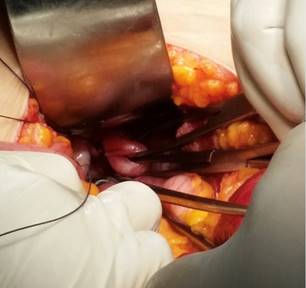
The patient was intervened by the general surgeon and the gynecologist through an initial median infraumbilical laparotomy approach. Evisceration of a portion of terminal ileum through a vaginal cuff defect approximately 3 cm in diameter was identified (Figure 2). The loops were reduced into the abdominal compartment and were not resected given that they had not sustained irreversible ischemia; the cuff defect was corrected using a 10-0 vycril crossed running suture and a Moschowitz technique in the cul-de-sac. Antibiotic therapy with first generation cephalosporins was initiated. Oral intake of clear fluids was initiated on the second postoperative day. Later, outpatient follow-up showed adequate correction of the defect.
MATERIALS AND METHODS
To answer the question “Which is the treatment for patients presenting with transvaginal evisceration secondary to vaginal cuff dehiscence following hysterectomy?” a search of the literature was conducted in the Medline via PubMed, Embase, Elsevier, and Wolters Kluwer Health databases and in the Medigraphic, National Institutes of Health (NIH), American College of Obstetricians and Gynecologists (ACOG), European Journal of Obstetrics and Gynecology (EJOG) websites, using the terms in English “vaginal cuff dehiscence,” “intestinal transvaginal evisceration,” “dehiscence after a hysterectomy,” and “hysterectomy complications”. Reports pertaining to robotic surgery were excluded given that this operation is seldom performed in our setting. The “snowball” method was used to conduct a search based on the bibliographic references retrieved, filtering for publications of the last ten years. Studies on vaginal cuff dehiscence and transvaginal evisceration were included as the study population. Assessment variables included age, type of hysterectomy, time elapsed between the surgery and the complication, prolapsed organ, approach to the correction, surgical technique used for the repair of the vaginal cuff and peritoneal defects, and postoperative measures.
RESULTS
Overall, 14 references were included: four cohort studies, 1,3,4,13 two of them multi-center cohorts, 1,4 one cross-sectional study, 11 three literature reviews, 2,6,10 two case series, 5,14 and four case reports 8,12,15,16 (Table 1).
Table 1 Systematic review of the literature of transvaginal evisceration during the period between 2006 and 2017
| Author | Country | Publication year | Design | Extracted variables |
|---|---|---|---|---|
| Agdi M, et al. (1) | Canada | 2009 | Multi-center cohort | Risk factors |
| Hur HC, et al. (2) | USA | 2016 | Review of the literature | Risk factors, prevention and management |
| Iaco PD, et al. (3) | Ireland | 2006 | Cohort | Prevention |
| Ceccaroni M, et al. (4) | Italy | 2011 | Multi-center cohort | Diagnosis and management |
| Hur HC, et al. (5) | USA | 2007 | Case series | Epidemiology and risk factors |
| Hur HC,et al. (6) | USA | 2016 | Review of the literature | Epidemiology, risk factors, prevention, diagnosis and management |
| Croak A, et al. (8) | USA | 2004 | Case series | Diagnosis |
| Cronin B, et al. (10) | USA | 2012 | Review of the literature | Risk factors and management |
| Hollman JP, et al. (11) | Mexico | 2014 | Cross-sectional | Epidemiology |
| Rajesh S, et al. (12) | England | 2008 | Case report | Management |
| Uccella S, et al. (13) | USA | 2012 | Cohort | Risk factors and management |
| Matthews CA, et al. (14) | USA | 2014 | Case series | Management |
| Pumar P, et al. (15) | Spain | 2016 | Case report | Management |
| Lobato JL, et al. (16) | Spain | 2016 | Case report | Management |
The literature is inconsistent as regards the association with the type of hysterectomy. Some authors have not found differences in incidence, 3 while others have reported that there is a higher association between the event and the laparoscopic technique, followed by the abdominal and vaginal approaches. 4,5,11. In a series of 54 cases, Agdi et al. reported that 51.9% of the cases occurred following laparoscopic surgery, while 33.3 and 14.8% occurred after abdominal and vaginal hysterectomy, respectively. 1 More recent studies suggest that the risk of dehiscence for laparoscopic procedures is 9 times higher, 15 including robotic surgery. 6
The time interval between hysterectomy and evisceration varies considerably and depends on the type of hysterectomy. 10 Agdi et al. described that in patients taken to laparoscopic surgery, the interval ranged between 4 and 7 weeks, while for the abdominal and vaginal approaches, the time period was longer, ranging between 13-22 weeks and 52-116 weeks, respectively. 1 Two cohort studies reported an inversely proportional relationship between patient age and the occurrence of the complication; early occurrence was more frequent among younger women (less than 6 months). 3,4 Some studies report longer intervals, ranging between 6 months and 5 years. 3,4,12,16
Regarding the laparoscopic surgical technique, a cross-sectional study reported that the use of hemostatic and cutting current results in more necrosis and altered vascularization. 6 In another study, this was associated with weakening of the suture due to the type of knot device used in this approach. 5 These authors suggest that eyepiece magnification results in the suture being supported in an insufficient amount of tissue. 5,6 Additionally, it could expose patients to shorter recovery time, prompting them to resume sexual activity earlier than is recommended. 15 Hollman and Rodríguez propose performing transvaginal cuff suture through laparoscopy after hysterectomy in order to reduce the risk of dehiscence. 11
The small bowel is usually the eviscerated organ, the distal ileum being the portion most often involved; 4,12,13 however, omentum, sigmoid, appendix and Fallopian tube prolapses have been described. 3,6
As for initial management, Hur et al.2 recommend a careful attempt at reducing the evisceration and then place a urinary catheter in order to avoid urine retention and package the vagina. If the transvaginal content cannot be reduced, they describe the need to cover the prolapsed organ with damp sponges and transfer the patient to the operating room right away. 2 Additionally, Iaco et al. mention support measures such as intravenous fluid replacement and intravenous prophylactic broad spectrum antibiotics. 3
Regarding the closure of the vaginal cuff defect, Matthews et al., in a case series, propose the use of single monofilament absorbable suture after margin debridement. 14 The inclusion of vaginal mucosa together with pubocervical and rectovaginal fascia has also been described. 2
In a case report published in England, Rajesh et al. propose suturing the uterosacral and cardinal ligamentous pedicles to the vagina and obliterating the cul-de-sac by joining the cuff and the anterior surface of the sigmoid colon. As a therapeutic option, they propose performing procedures described for the repair of vesicovaginal fistulae using omentum flaps (Bastiaanse procedure), with interposition of cavernous bulb muscle and labial skin (Martius), gracilis muscle-skin flap (Ingelman-Sundberg) and gluteus maximums or anterior rectus muscle-skin flap. 12
Lobato et al. suggest that the repair may be performed through the abdominal or vaginal approach or through a combination of the two; 16 however, Hur et al. recommend individualizing the decision based on patient stability and the skills of the surgeon performing the correction. 2
CONCLUSIONS
Transvaginal evisceration is a surgical emergency. Initial management should be based on vaginal packing and prophylactic antibiotics. Different surgical alternatives can be used to correct the vaginal cuff defect through which the evisceration occurs. Further studies are required to assess the safety and effectiveness of the different interventions for the management of this condition.











 text in
text in