INTRODUCTION
Acute mesenteric thrombosis (AMT) occurs after occlusion of the mesenteric artery or vein. AMT is difficult to diagnose and often fatal 1. The goal of treatment is early detection, but diagnosing it is difficult, especially in the early stages when intervention is most beneficial. Most patients present sudden onset abdominal pain. It may be characterized by an initial discrepancy between the severity of abdominal pain and the findings of a physical examination 2. Patients may also present nausea and vomiting in the early stages of the disease 3. Diagnosis is performed by visualizing the vascular thrombus through imaging methods 1,4. Mesenteric venous thrombosis (MVT) is a rare insidious condition with an incidence of 2.7 per 100,000 people-years 2.
Physiological changes affecting coagulation factors and stasis due to uterine vena cava compression cause hypercoagulation in pregnant women. Heit JA et al. reported that the overall incidence of venous thromboembolism among pregnant or postpartum women was 199.7 per 100,000 women-years during the 30-year study period, 1966 to 1995 5.
In this study, the aim was to contribute to the literature on this condition, which requires rapid diagnosis and treatment. This was done by presenting a case of a woman who became pregnant after in vitro fertilization and embryo transfer (IVF-ET), who developed acute MVT on the 7th week of pregnancy. Although there are some cases reported on this subject, they are still insufficient. More studies are required to evaluate the factors associated with the development of this condition during pregnancy.
CASE REPORT
The female patient with a 7-week pregnancy achieved by IVF-ET resorted to our emergency services with abdominal pain, nausea, vomiting and diarrhea that had continued the last 3 days and gradually exacerbated. No abnormality was detected in the ultrasonographic examination, including embryonic cardiac activity, and conservative medical treatment was provided because the patient's complaints were related to pregnancy. However, the patient, whose complaints worsened, turned to our emergency services a second time.
The consultation was held in September 2021 at the General Surgery Unit of the Katip Çelebi University Faculty of Medicine, Atatürk Education and Research Hospital. There was no special condition in the patient's family history. There was a median incision scar above and below the umbilicus due to urological intervention m childhood. Body mass index was 24.6 kg/m2.
The patient was ordered to be administered oral estrogen therapy (2 mg/day Estradiol), intravaginal progesterone (4x200 mg/day) and acetylsalicylic acid (ASA, 100 mg/day) in the context of the IVF-ET protocol. She had tachycardia (110 bnp) at the time of admission, and her blood pressure and fever values were normal. At the time of baseline examination, signs of severe acute abdomen were observed. The laboratory findings were as follows; white blood cells: 24,800/µL, platelet count: 290,000/µL, C-Reactive Protein (CRP): 154 mg/L, INR:0.98 and beta-human chorionic gonadotropin (β-HCG): 54,335 mU/ml.
Abdominal ultrasonography revealed dilatations in the intestinal anses, free fluid in the pelvis, a left ovarian cystic lesion and 7-week pregnancy sac, but no embryonic cardiac activity. Additionally, the gynecological consultation also confirmed the embryonic heartbeat was absent. The patient refused to undergo a computed abdominal tomography and other radiological tests.
After the patient's abdominal pain and fever increased, blood tests were performed again and an increase in inflammation markers was observed. The patient accepted to undergo surgery after peritonitis findings exacerbated and her general condition started to deteriorate. We obtained informed consent from the patient. Surgical exploration encountered slightly serohemorrhagic fluid of 200 cc, as well as circulatory impairment and necrosis intermittently located at the two separate sections of the small intestine, beginning from the 90th cm after the Treitz ligament in the abdomen (Figure 1). A necrotic small bowel resection of approximately 150 cm was performed at two separate sections. The other findings observed during the surgery were as follows: 1) thrombi in the moderate and small-sized veins of the small bowel mesentery despite the presence of pulses in the arteries feeding the small intestines, 2) thickening of small bowel mesentery, 3) small and moderate-sized venous vein dilatation observed in the right halves of the right colon and transverse colon, and 4) left ovarian cystic lesion. Towards the end of the surgery, regeneration of ischemic fields was encountered in the small bowel segments close to the anastomosis. A second-look laparotomy was decided upon to control the presence of new ischemia in the small intestines.

Figure 1 Small bowel resection material. There are areas of ischemia and necrosis in two different parts of the small intestine.
The administration of intravenous total parenteral nutrition (40 cc/h), intravenous antibiotics and full anticoagulation with low molecular weight Heparin (2*6000 anti-Xa IU) was postoperatively initiated and continued until discharge from the hospital. The embryo was removed after confirmation of stillbirth by the postoperative gynecological examination. The contrast-enhanced computed tomography (CT) performed on the 1st postoperative day revealed a long segment thrombus in the superior mesenteric vein (SMV) and pulmonary embolism (Figure 2). A second-look laparotomy was carried out 48 hours after the first surgery. The exploration showed that blood supply and feeding of all the intestinal anses were intact, while no anastomotic complication was present. The histopathological examination of the section resected in the first surgery demonstrated sporadic necrotic fields in the small bowel wall (Figure 3).
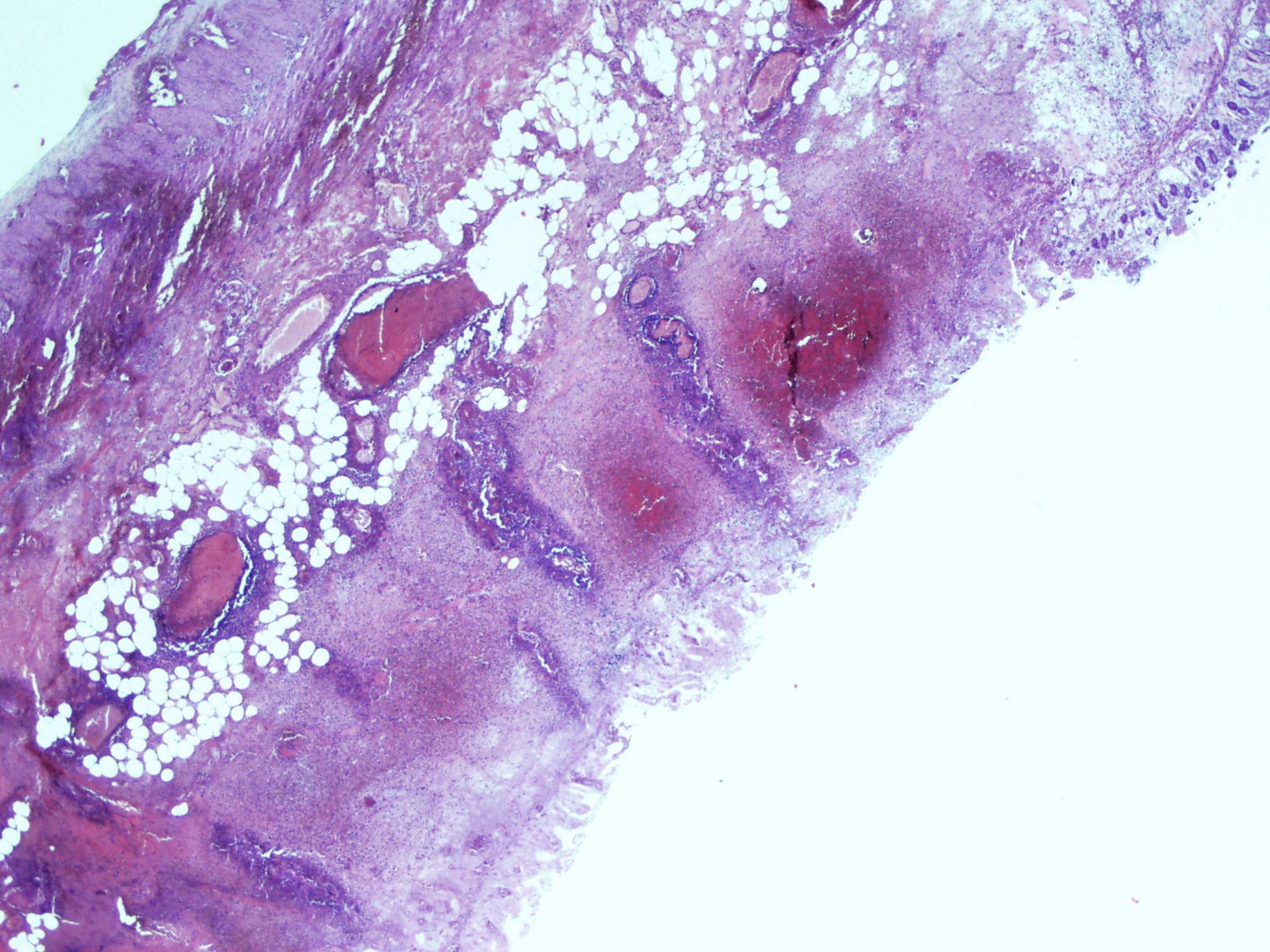
Figure 3 Histopathologically, ischemic cell groups, congestion, and edema. Thrombosed vascular vein branch. H&E, x40.
The thrombophilia panel of the patient showed Factor V Leiden (FVL) (homozygous), Methylenetetrahydrofolate reductase (MTHFR) (heterozygous) and Plasminogen Activator Inhibitor 1 (PAI-1) 4G/5G (homozygous) gene mutations. The levels of Protein S (49 % [reference: 60-130 %]) and Protein C (62 % [reference:70-140 %]) were lower than normal limits. The patient was discharged without any complication. The patient has been monitored by the polyclinic without any complication since the 6th postoperative month.
MATERIALS AND METHODS
The PubMed/Medline and LILACS online searchengines were navigated using the words "mesenteric venous thrombosis, pregnancy." The questions for our research were: What are the risk factors in the etiology in these patients? What are the treatment methods? The search was limited to English and Spanish language articles reporting on human subjects and published between 2000 and 2022. The search was extended to other sources of information based on the "snowball" strategy from retrieved studies. Studies included case reports and case series that address risk factors associated with the development of thrombosis and intestinal ischemia in pregnant women. Studies were excluded in which mesenteric thrombosis was not diagnosed outside of pregnancy or in which a thrombotic event of a different location to the location of interest was documented.
All retrieved titles and abstracts were screened by three authors who, applying the inclusion and exclusion criteria, defined those to be analyzed. Discrepancies were resolved by consensus. A narrative synthesis of the included studies has been presented.
Ethical aspects: Ethical competence was maintained by obtaining the patient's consent during the preparation phase of the study. Written informed consent was obtained from the patient for publishing this case report.
RESULTS
A literature review was performed including pregnant patients between the ages of 18-55 and women with additional risk factors. As a result of the bibliographic search, "mesenteric ischemia, pregnancy" 73 titles were retrieved, of which 18 studies met the inclusion criteria. Two studies were excluded because they are related to portal vein thrombosis. All the remaining studies were case reports or case series from different countries. The included studies were published in English, but not Spanish. In total, 17 cases of mesenteric thrombosis associated with pregnancy were reported. There was no pathology accompanying pregnancy in 8 patients 2,6-12. Two patients had protein S deficiency during pregnancy 13,14. One patient had antithrombin deficiency and one patient had a factor 5 leiden mutation 15,16. One patient presented estrogen use 17. One patient received IVF-ET treatment 18. Pregnancy was accompanied by mesocolic and infectious pathologies in the remaining 3 patients 19-21. Surgical treatment was applied to 14 of 17 patients in the literature. Inoperable follow-up and low molecular weight heparin were given to 2 patients 8,16. The treatment for 1 patient was unclear. Segmentary small bowel resection and enteroenterostomy were performed on 6 patients 2,6,12,14,17,20. Termination of pregnancy was performed by uterine curettage, in addition to small bowel resection and anastomosis in 3 patients 11,13,18. Small bowel resection and curettage were applied to one of the patients, but there was no data on bowel continuity 7. One patient had normal labor with small bowel resection and anastomosis 10. Sigmoid colon resection and Hartman colostomy were performed on 2 patients 9,21. Diagnostic laparotomy was applied to 1 patient, and then labor was normal 19.
DISCUSION
MVT is a rare disorder accounting for only 1 in 5,00015,000 hospital admissions, and it has a mortality rate of 20-50 % 3. Clinically, non-specificsymptoms, such as abdominal pain, flatulence, nausea and vomiting emerge at the beginning 11. In pregnant women, these symptoms are considered normal changes, especially due to pregnancy. In addition, early and accurate MVT diagnoses are difficult, since using abdominal CT scans as the most effective diagnostic method is being debated and can be disadvantageous for the pregnant women 1-4. As a matter of fact, the definite diagnosis for this case could only be established by a laparotomy and postoperative CT. On the other hand, magnetic resonance imaging (MRI) is always kept in mind as one of the most important imaging methods for pregnant patients with acute abdominal pain, since it is performed without using any ionizing radiation. Some studies have shown that Doppler ultrasounds can be used with sensitivity (100 %) and specificity (93 %) in detecting portal and mesenteric vein thrombosis 22-24. Both imaging techniques could not be performed in the presented case because of the admission time of the patient, clinical picture and technical difficulties.
Despite the increased tendency of pregnant women to develop thrombosis, isolated MVT is very rare 2,5,11,25. On the other hand, it has been also noted that the risk for VTE in the first trimester of pregnancies achieved by IVF-ET is 10 times higher than for the normal pregnant population 26. Although pregnant patients with MVT carry various additional risk factors, they remain idiopathic in most of the cases because of MVT 2. Only one patient who achieved pregnancy after IVF-ET and developed acute MVT has been reported in the literature 11. It has been accepted as idiopathic because no additional risk factor has been detected in the patients 11. Even though our patient was reported to be the second patient who developed acute MVT after IVF-ET, she presented it differently because of FVL mutation. Additionally, it has been reported that pregnancies after IVF occur due to ovarian hyperstimulation syndrome (OHSS) at a 6-7 % rate. Therefore, they have a 1.7 % risk of venous thromboembolism (VTE) in the first trimester that is 100 times higher than the general population 18. Likewise, left ovarian cystic lesions due to hyperstimulation were also identified in our patient.
Genetic thrombophilia screening is recommended for young patients with detected thromboembolisms in the presence of recurring episodes and thrombosis in unexpected locations 4. The frequency of the FVL mutation was determined to be as high as 17 % in patients with MVT, which is higher than the normal population 4. Similarly, with the presented case, performing genetic thrombophilia screening is extremely important when thrombosis has been detected in a very rare location. We conclude that the development of acute SMV thrombosis after IVF-ET was caused by factors, such as pregnancy, gene mutations and medications administered in the IVF-ET process.
Treatment for mesenteric ischemia due to acute SMV thrombosis is urgent. It requires early surgical exploration, anticoagulant therapy and elimination of the factor that causes thrombosis 1-5. The other issue to be discussed on this point is decision-making related to the fetus. Hospital admission due to acute SMV thrombosis is a very rare condition in the process of pregnancy achieved after IVF-ET. The main problem is how extremely important the pregnancy is for the family while the mother's life is at risk due to a serious life-threatening pathology. It has been reported in the gynecological/obstetric consultation of our patient that the fetus was exitus and it could be removed at any time, since there was no emergency. However, as with the first case reported in the literature, the pregnancy in our case was terminated on the first postoperative day because we agreed with the opinion that necrotic materials of fetal origin could make the clinical picture more challenging and complicated via pro-coagulatory and pro-inflammatory effects 11. We conclude that terminating pregnancy might be one of the many effective factors in the improvement of the clinical picture in the following days. However, our conclusion is completely based on individual clinical observation and is naturally debatable. The death of the fetus facilitated our decision-making process. We consider that making this decision could not be as easy if the fetus was alive.
CONCLUSIONS
SMV thrombosis is a life-threatening and very rarely seen condition that emerges in pregnancies. The literature suggests that, during gestation, the factors associated with the development of acute mesenteric thrombosis are hypercoagulability induced by pregnancy, the administration of oral estrogen during IVF-ET, and other precipitating factors. More studies are required to better understand the possible additional factors and build better optimal treatment algorithms.















