Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Colombiana de Psiquiatría
Print version ISSN 0034-7450
rev.colomb.psiquiatr. vol.36 no.4 Bogotá Oct./Dec. 2007
Psychometric Properties of the CES-D Scale Among Colombian Adults from the General Population
Propiedades psicométricas de la escala CES-D en la población adulta colombiana
Adalberto Campo-Arias1, Luis Alfonso Díaz-Martínez2, Germán Eduardo Rueda-Jaimes2, Laura del Pilar Cadena-Afanador2, Nubia Leonor Hernández3
1 Human Behavioral Research Institute. Associate professor, Medicine School, Autonomous University of Bucaramanga; Nursing School, University of Cartagena; and Psychology School, University of Sinu, Cartagena, Colombia. campoarias@comportamientohumano.org y acampoar@unab.edu.co.
2 UNAB Neuropsychiatry Research Group, School of Medicine, Autonomous University of Bucaramanga, Bucaramanga, Colombia.
3 Assistant professor, Medicine and Psychology School, Autonomous University of Bucaramanga. Bucaramanga, Colombia.
Abstract
Background: Around the world, the Center for Epidemiologic Studies Depression Scale (CES-D) is the most popular instrument to identify depressive disorders in the community. However, this scale has not been validated in Colombia. Objective: To validate the CES-D in the general population of Bucaramanga, Colombia. Method: A random sample of adults (N=266) was evaluated. After the participants completed the CES-D, a psychiatrist interviewed them to detect a current major depressive episode (MDE) using the Structured Clinical Interview for a DSM-IV diagnosis. Results: The psychiatric clinical interview identifi ed 44 (16.5%) people with MDE. The ROC suggested 20 as the best cut-off point. With this cut-off point, 102 (38.3%) people reported clinically meaningful depressive symptoms, with an observed concordance of 0.77 (95%CI 0.71-0.82); sensitivity for a MDE, 0.96 (95%CI 0.83-0.99); specifi city, 0.73 (95%CI 0.67-0.79); positive predictive value, 0.41 (95%CI 0.32-0.51); negative predictive value, 0.99 (95%CI 0.95-1.0); positive likelihood ratio, 3.53; negative likelihood ratio, 0.06; and Cohen’s kappa test, 0.45 (95%CI 0.35-0.55). The Cronbach’s alpha was 0.87, and four factors explained 50.3% of the variance. Conclusions: The CES-D with a cut-off point of 20 may be a useful tool for MDE screening in Colombian adults.
Key words: Scales, CES-D, validation studies, population surveillance, major depressive disorder, psychometrics, Colombia.
Resumen
Antecedentes: La escala del Centro para Estudios Epidemiológicos de la Depresión (CES-D) es el instrumento más conocido para identifi car trastornos depresivos en población general. Sin embargo, no ha sido validada en población colombiana. Objetivo: Validar la CES-D en adultos de Bucaramanga, Colombia. Método: 266 adultos (muestra aleatoria) completaron la CES-D. Luego, los participantes fueron entrevistados por un psiquiatra para identifi car un episodio depresivo mayor mediante la aplicación de la entrevista estructurada para diagnósticos del eje I (SCID-I). Resultados: Con la entrevista clínica se identifi caron 44 personas (16.5%) con episodio depresivo mayor (EDM). La curva ROC sugirió que 20 es el mejor punto de corte. Con este punto de corte, 102 participantes (38.3%) informaron síntomas depresivos con importancia clínica; la concordancia observada fue 0.77 (IC95% 0.71-0.82); la sensibilidad para un EDM, 0.96 (IC95% 0.83-0.99); la especifi cidad, 0.73 (IC95% 0.67-0.79); el valor predictivo positivo, 0.41 (IC95% 0.32-0.51); el valor predictivo negativo, 0.99 (IC95% 0.95-1.0); la razón de verosimilitud positiva, 3.53; la razón de verosimilitud negativa, 0.06; y la kappa de Cohen, 0.45 (IC95% 0.35-0.55). Se observó un coefi ciente de alfa de Cronbach de 0.86 y cuatro factores que explicaban el 50.3% de la varianza. Conclusiones: La CESD con un punto de corte de 20 puede ser un instrumento útil para identifi car EDM en adultos de Bucaramanga.
Palabras clave: escalas, CES-D, estudios de validación, población general, episodio depresivo mayor, psicometría, Colombia.
Background
The Center for Epidemiologic Studies Depression Scale (CES-D) is a self-report depression rating tool designed to identify depressive disorders among community dwelling people (1). After its publication, the CES-D has shown to have a good sensitivity and specifi city for identifying depressive disorders in community samples (2). However, the CES-D has also been used and validated in other populations, especially primary care and general inpatients (3-5). The validation of a scale, particularly in the general population, is a complex and expensive task. This may explain the delayed validation of the CES-D in the Colombian population (6).
Depressive disorders are very common among Colombian people (7). Recent studies show inconsistent prevalences of major depressive episodes (MDE) during the last-month among Colombian community people. One investigation reported a last-month MDE prevalence of 2% using the Composite International Diagnostic Interview (CIDI), which is a structured interview applied by lay interviewers (8). Another survey found a prevalence of 9% applying the Structured Clinical Interview for DSM-IV axis I diagnosis (SCID-I). This is a semi-structured questionnaire applied by psychiatrists (9). It is apparent that MDE prevalences change across the different instruments used. The discrepancy between lay and psychiatrist interviews, like the CIDI and SCID-I is well-known (10). The prevalence established by psychiatric interview is more accurate. The CIDI has a high reliability, although it also exhibits a modest sensitivity that compromises diagnosis validity (11).
Additionally, similar to observations made in other countries, MDE prevalences vary across Colombian regions. In Bucaramanga, a northeastern city at Colombia, the prevalence reaches 15% of the population, the highest in Colombia (9). However, any explanation is unknown at this point. MDE and other depressive disorders decrease the quality of life of people and have a signifi cant impact on country economies causing many daily labor loss (12,13).
The CES-D has never been validated formally as an MDE screening scale among the Colombian community people and used in any Colombian study. The CES-D has exhibited a good content, criterion and discriminant validity (3). However, the four-factor structure proposed by Radloff (1) has not been replicated in several populations (14-16).
The validation of a scale is required for any population with special or particular sociocultural characteristics or background (17); for instance, it was found that the CES-D may measure different constructs across ethnic and cultural groups (14). Moreover, the cut-off point must be adjusted for any population. The prevalence of a mental disorders in a population affects the scale performance (18). The cut-off point should be a higher point among populations with a low prevalence, like usually among people are dwelling in community, and a lower one in populations with a high prevalence, like clinical settings (19).
Validating the CES-D in the Colombian general population has various advantages: it may be a cheap, easy and quick way to recognize people with clinically meaningful depressive symptoms (20); it might facilitate the comparison of similar surveys in different countries; it might increase the possibility of people speaking about depressive symptoms in primary care settings (the number of times that people ask for professional help for these symptoms when they are surveyed in general community); and it may assist physicians in detecting depressive disorders among outpatients (21). The objective of this research was to validate the CES-D among people living in the urban area of Bucaramanga, Colombia.
Method
Research design
This article describes a validation study of a diagnostic test in the general population from Bucaramanga, Colombia, during 2004.
Ethical considerations
Review Board from the School of Medicine of the Universidad Autónoma de Bucaramanga, Colombia, approved this project. After knowing the objectives and minimum risks for participating, all participants signed a written informed consent.
Participants
A random sample of adults from the general population was selected and asked to participate in this research. In Bucaramanga, the prevalence of a current major depressive may reach 15%. The sample selection was multistage. First, blocks were randomly chosen from all blocks in Bucaramanga, then a house was randomly chosen from within blocks, and fi nally one person was randomly chosen per home. Selections were done using a random number list for each stage. The random number list was taken from Epi-info (22). We included 18-65 year-old people. Illiterate people were excluded.
Two hundred ninety-nine persons were contacted to take part of this research. Thirty-three people refused to participate (11%). Thus, we interviewed a total of two hundred sixty-six persons. The sample’s mean age and formal education were 37.48 (SD = 12.92; Min = 18, Max = 65) and 9.85 (SD = 4.71; Min = 0, Max = 25) years. The gender composition of this sample was 57% females and 43% males. Fifty-two percent were employees, 24% housewives, 12% students, 7% unemployed and 5% retired. Fifty-six percent were married and 44% single, widow or widower. The socioeconomic status was low 34%, middle 51% and high 15%, according to the residential neighborhood (Offi cial information).
Procedure
Initially, participants reported depressive symptoms using the CES-D scale. The CES-D is a 20- item Likert-type scale that explores symptoms frequency during the last week. Each answer is scored from zero to three points, and the total score ranges from 0 to 60. Usually, 16 is taken as a cut-off point for clinically important depressive symptoms (1). The process of traduction and re-traduction was done for the English original version of the CES-D. A psychiatrist performed a clinical interview using the module for a current major depressive episode from the Spanish Structured Clinical Interview for DSM-IV Axis I disorders, Clinical Version (23).
One assistant gave instructions to participants for completing properly the CES-D, and a psychiatrist made the clinical interview blinded to the CES-D results; this interview was taken as the gold standard. People who met criteria for a major depressive disorder or other depressive disorder according to the clinical interview were counseled and remitted to their own medical or psychological services.
Statistical analysis
Sensitivity, specifi city, predictive values and likelihood ratios were also computed. In addition, Cohen’s kappa was computed to examine concordance (24). Ninetyfive percent confidence intervals (95%CI) were computed. In order to identify convenient cut-off points, a Receiver Operating Characteristic (ROC) curve analysis was performed (25). Cronbach’s alpha coeffi cientwas used to establish internal consistency of the CES-D (26). A maximum likelihood confi rmatory factor analysis was performed to fi nd out the CES-D dimensionality (27, 28). The number of factors was determined using a combination of criteria: a minimum eigenvalue of 1.0, item loading higher 0.35, and at least three items per factors. The solution was then subjected to a promax rotation with Kaiser normalization, in order to identify the correlated factors that building the construct of a major depressive episode. STATA 9.0 was used for all statistical tests (29).
Results
The CED-S scores ranged from zero to fi fty-two points, with a mean of 17.16 (SD = 9.88) and median of 16 (interquartile range 9-24). The psychiatric structured interview identifi ed 44 (16.5%) people with a current major depressive episode (MDE).
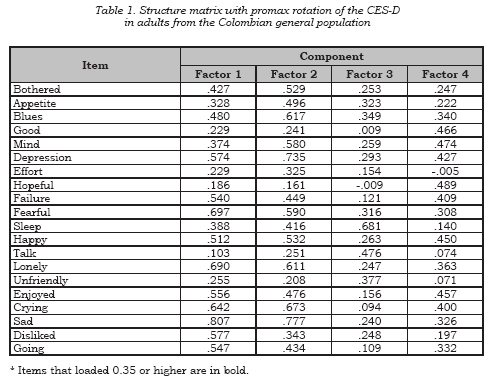
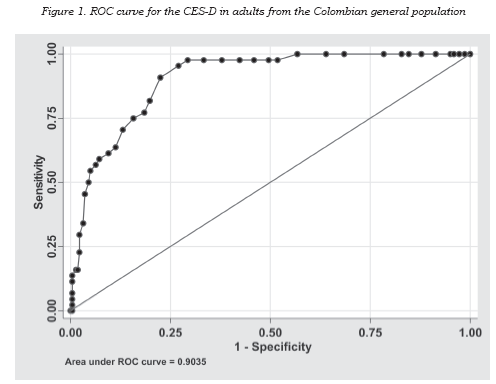
Cronbach´s internal consistency was 0.87. Four factors were identifi ed, the fi rst (depressed mood) showed an eigenvalue of 6.239 that explained 31.2% of the variance; the second (principally positive mood) exhibited an eigenvalue of 1.497 that accounted for 7.5% of the variance; the third (especially interpersonal problems) presented an eigenvalue of 1.183 that explained 5.9% of the variance; and the fourth (principally somatic) exhibited a eigenvalue of 1.149 that account for 5.7% of the variance. The factor matrix appears in Table 1. The area under the ROC curve was 0.90 (95%CI 0.86-0.94, see Figure 1).
Using the usual cut-off point of 16, a group of 137 (51.5%) people reported clinically important depressive symptoms; the observed concordance was 0.64 (95%CI 0.58- 0.70); sensitivity for a MDE, 0.98 (95%CI 0.87-1.0); specifi city, 0.58 (95%CI 0.51-0.64); positive predictive value, 0.31 (95%CI 0.24-0.40); negative predictive value, 0.99 (95%CI 0.96-1.0); positive likelihood ratio, 2.31; negative likelihood ratio, 0.04; and Cohen’ kappa test, 0.30 (95%CI 0.21-0.39).
The ROC suggested 20 as the best cut-off point. With this cut-off point, 102 (38.3%) people reported clinically meaningful depressive symptoms, with an observed concordance of 0.77 (95%CI 0.71-0.82); sensitivity for a MDE, 0.96 (95%CI 0.83-0.99); specifi city, 0.73 (95% CI 0.67-0.79); positive predictive value, 0.41 (95%CI 0.32-0.51); negative predictive value, 0.99 (95%CI 0.95-1.0); positive likelihood ratio, 3.532; negative likelihood ratio, 0.06; and Cohen’s kappa test, 0.45 (95%CI 0.35-0.55).
In the other hand, the cutoff point of 30 classifi ed the most correctly people with or without a MDE; at this point, 35 (13.2%) persons reported clinically important depressive symptoms, with a observed concordance 0.88 (CI95% 0.84-0.92), sensitivity 0.55 (CI95% 0.39-0.69); specifi city, 0.95 (95%CI 0.91-0.97); positive predictive value, 0.69 (95%CI 0.51-0.83); negative predictive value, 0.91 (95%CI 0.87- 0.95); positive likelihood ratio, 11.0; negative likelihood ratio, 0.48; and Cohen’s kappa test, 0.54 (95%CI 0.42-0.66).
Discussion
This study found that the CESD scale is a useful tool to identify current major depressive episodes in Colombian adults from the general population. This scale showed high sensitivity, good specifi city, excellent discrimination, and acceptable concordance with the Structured Psychiatric Clinical Interview. Moreover, the CES-D exhibited an acceptable internal consistency and a four-factor structure that explained 50% of the variance.
Consistently with prior validation studies among community-dwelling people, the CES-D scale may detect clinically important depressive symptoms with high accuracy. In the general population, older studies concluded that the CES-D is a successful indicator of depressive episodes (2, 30). However, in contrast with community samples, CES-D scores predicted accurately major depressive episodes and other mental disorders such as anxiety and substance abuse disorders in a sample of primary medical care patients (31). Breslau reported similar fi ndings; the CES-D did not measure exclusively depressive symptoms because the CES-D detected equally major depression and generalized anxiety (32). Likewise, the cut-off point should be adjusted for screening a particular population (19). It was observed that in the Colombian people the best cut-off point was 20. This point is near the ideal properties for a screening scale: sensitivity of 0.95 and specifi city of 0.80. These tools always presented “false positives” o “false negatives”. Although, the CES-D exhibited an area under ROC curve that it is considered excellent discrimination between subject who experience MDE versus those who do not (33); it is necessary to keep in mind that screening scales are only a rough measure of clinical depressive disorders; so, a further psychiatric clinical evaluation is required in order to know the accurate diagnosis (9, 34).
The chance adjusted agreement or concordance between the CES-D and the psychiatric clinical structured interview (kappa) was relatively modest. It is important to consider that the prevalence of a condition affected strongly the kappa. The concordance is poor when the prevalence is low (35). Although, for screening scales the most wanted property is to have a high sensitivity. The prevalence of any condition does not affect the sensitivity of a scale (36).
The Cronbach’s alpha coeffi - cient (internal consistency) of the CES-D scale indicates that its items present a high degree of interrelatedness and points out a strong common factor (28, 37). The four extracted factors that explained the half of the variance. This factor solution does not corroborate the unidimensionality or homogeneity of the CES-D among Colombian adults from the general population (27). However, the four high-correlated factors could represent the current global construct of a major depressive episode. Comparison is diffi cult, investigators commonly use different criteria for determining the number of factor. If Gorsuch’s recommendations are considered this four-factor solution can be rejected (38). The eigenvalue of 1.0 overestimates the number of factors when items of a scale have low correlations (39), then salient factors must be just left out. A salient factor loads greater than 1.40 (40). So, possibly the two-factor solution could be better, if it is kept in mind that the fi rst principal factor accounted for 31% of the variance and the second factors just explained 7% of the variance. But, this perspective has a big problem. Streiner suggests that the extracted factors should be responsible at least of 50% of the variance (27).
As it is expected, factor solution of the CES-D changes according to population. Schroevers, Sanderman, van Sonderen, and Ranchor identifi ed two factors (depressed and positive affect) in cancer patients and healthy controls (4). Guarnaccia, Angel, and Worebey found different factor structures for the CES-D in Mexican-American, Cuban-American and Puerto Rican samples (41). Besides, Nguyen, Kitner- Triolo, Evans, and Zonderman did support a four-factor structure for the CES-D in a representative sample of African Americans and Caucasians (42). It is well accepted that social, economic, and cultural backgrounds affect the answer pattern of a scale (17). For instance, Brown, Schulberg, and Madonia (43) and Iwata, Turner, & Lloyd observed that depressed African Americans, compared with Caucasians, reported more frequently somatic symptoms than affective and cognitive symptoms (44). Similarly, depressed Latino Americans are more likely than North Americans to complain of somatic symptoms (45).
In different populations or settings, using a self-reporting depressive symptom scale is an excellent option for identifying possible cases of MDE (46). General and primary care practitioners have some diffi - culty to diagnose depressed patients (47). Data suggests that depression screening improves the possibility of seeking treatment, that is to say, depressed people living in community who complete a self-report scale ask for the professional help more frequently (48). Also, it is very important to provide education for enhancing diagnostic and treatment skills of physicians in primary care and other contexts (49, 50).
In conclusion, the CES-D with a cut-off point of 20 can be used for screening a current major depressive disorder in adults from the general population of Bucaramanga, Colombia. Investigations are needed to replicate this CES-D validity in different care settings and other Colombian cities.
Acknowledgements
We are grateful with Ms. Liliana Fabiola Ruiz, Ms. Claudia Liset Oviedo and all of the medical students who collaborated in this study. This research was completely supported by a grant from the Dirección de Investigaciones of the Universidad Autónoma de Bucaramanga (code 2105).
References
1. Radloff LS. The CES-D scale: a selfreport depression scale for research in the general population. Appl Psychol Measur. 1977;1(3):385-401. [ Links ]
2. Boyd JH, Weissman MM, Thompson WD, Myers JK. Screening for depression in a community sample. Understanding the discrepancies between depression symptom and diagnostic scales. Arch Gen Psychiatry. 1982;39(10):1195-200. [ Links ]
3. Weissman MM, Schlomskas D, Pottenger M, Prussoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol. 1997;106(3): 203-14. [ Links ]
4. Schroevers MJ, Sanderman R, van Sonderen E, Ranchor AV. The evaluation of the Center for Epidemiologic Studies Depression (CES-D) scale: depressed and positive affect in cancer patients and healthy reference subjects. Qual Life Res. 2000;9(9):1015- 29. [ Links ]
5. Caracciolo B, Giaquinto S. Criterion validity of the center for epidemiologic studies depression (CES-D) scale in a sample of rehabilitation inpatients. J Rehabil Med. 2002; 34(5): 221-225. [ Links ]
6. Dewey ME. Designs for studies evaluating tests. Int J Geriatr Psychiatry. 1997;12(4):492-494. [ Links ]
7. Demyttenaere K, Bruffaerts R, Posada- Villa J, Gasquet I, Kovess V, Lepine JP, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291(21):2581-90. [ Links ]
8. Posada-Villa JA, Aguilar-Gaxiola SA, Magaña CG, Gómez LC. Prevalence of mental Disorders and use service: preliminary results from National Study of Mental Health, Colombia, 2003 (In Spanish). Rev Colomb Psiquiatr 2004; 33: 241-262. [ Links ]
9. Gómez-Restrepo C, Bohórquez A, Pinto Masis D, Gil Laverde JF, Rondon Sepúlveda M, Díaz-Granados N. The prevalence of and factors associated with depression in Colombia. Rev Panam Salud Pública. 2004;16(6):378-86. [ Links ]
10. Wittchen HU, Ustün TB, Kessler RC. Diagnosing mental disorders in the community. A difference that matters? Psychol Med. 1999;29(5): 1021-7. [ Links ]
11. Andrews G, Peters L. The psychometric properties of the Composite International Diagnostic Interview. Soc Psychiatry Psychiatr Epidemiol. 1998;33(2):80-8. [ Links ]
12. Battaglia A, Dubini A, Mannheimer R, Pancheri P. Depression in the Italian community: epidemiology and socioeconomic implications. Int Clin Psychopharmacol. 2004;19(3):135-42. [ Links ]
13. Ustün TB, Ayuso-Mateos JL, Chatterji S, Mathers C, Murray CJ. Global burden of depressive disorders in the year 2000. Br J Psychiatry. 2004;184:386-92. [ Links ]
14. Golding JM, Aneshensel CS. Factor structure of the center for epidemiologic studies depression scale among mexican americans and non-hispanic whites. J Consult Clin Psychol. 1989;1(3):163-168. [ Links ]
15. Stroup-Benham CA, Lawrence RH, Treviño FM. CES-D factor structure among Mexican American and Puerto Rican women from single-and coupled-headed households. Hispanic J Behav Sci. 1992;14(3): 310-326. [ Links ]
16. Posner SF, Stewart AL, Marín G, Pérez- Stable EJ. Factor variability of the Center for Epidemiological Studies Depression Scale (CES-D) scale among urban latinos. Ethn Health. 2001;6(2):137-144. [ Links ]
17. Rubio-Stipec M, Hicks MHR, Tsuang MT. Cultural factors influencing the selection, use, and interpretation of psychiatric measures [CD-ROM]. In: Rush AJ, Pincus HA, First MB, Zarin DA, Blacker D, Endicott J, et al. Handbook of psychiatric measures. Washington: American Psychiatric Association;2002. [ Links ]
18. Grimes DA, Schulz KF. Uses and abuses of screening tests. Lancet. 2002;359(9309):881-4. [ Links ]
19. Irwing L, Bossuyt P, Glasziou P, Gatsonis C, Lijmer J. Designing studies to ensure that estimates of test accuracy are transferable. BMJ. 2002; 324(7338): 669-71. [ Links ]
20. Kerr LK, Kerr LD Jr. Screening tools for depression in primary care: the effects of culture, gender, and somatic symptoms on the detection of depression. West J Med. 2001;175(5):349- 52. [ Links ]
21. Pérez-Stable EJ, Miranda J, Muñoz RF, Ying YW. Depression in medical outpatients. Underrecognition and misdiagnosis. Arch Intern Med. 1990;150(5):1083-8. [ Links ]
22. Dean AG, Dean JA, Coloumbier D, Burton AH, Brendel KA, Smith DC, et al. Epi Info 6.04c. A word processing, database, and statistic program for public health [Database] Atlanta and Geneva: Center for Disease Control and Prevention and World Health Organization; 1997. [ Links ]
23. First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV axis I diagnosis –clinical version. (In Spanish). Barcelona: Masson; 1999. [ Links ]
24. Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37-46. [ Links ]
25. Rey JM, Morris-Yates A, Stanislaw H. Measuring the accuracy of diagnostic test using receiver operating characteristics (ROC) analysis. Int J Method Psychiatr Res. 1992;2:39-50. [ Links ]
26. Cronbach LJ. Coefficient alpha and the internal structure of test. Psychometrika. 1995;16:297-334. [ Links ]
27. Streiner DL. Figuring out factors: the use and misuse of factor analysis. Can J Psychiatry 1994; 39(3):135-140. [ Links ]
28. Oviedo HC, Campo-Arias A. An approach to the use of Cronbach’s alpha (In Spanish). Rev Colomb Psiquiatr 2005;34(4):572-580. [ Links ]
29. STATA for windows 9.0. [software]. College Station, Texas; Stata Corporation, 2005. [ Links ]
30. Myers JK, Weissman MM. Use of a self-report symptom scale to detect depression in a community sample. Am J Psychiatry. 1980;137(9): 1081-4. [ Links ]
31. Fechner-Bates S, Coyne JC, Schwenck TL. The relationship of self-reported distress to depressive disorders and other psychopathology. J Counsult Clin Psychol. 1994;62(3): 550-9. [ Links ]
32. Breslau N. Depressive symptoms, major depression, and generalized anxiety: a comparison of self-reports on CES-D and results from diagnostic interviews. Psychiatry Res. 1985;15(3): 219-29. [ Links ]
33. Hosmer DW, Lemeshow S. Applied logistic regression. New York: John Wiley & Sons Inc; 2000. [ Links ]
34. Williams JW Jr, Noël PH, Cordes JA, Ramirez G, Pignone M. Is this patient clinically depressed? JAMA. 2002; 287(9): 1160-70. [ Links ]
35. Boisvert JA, McCreary DR, Wright KD, Asmundson GJ. Factorial validity of the center for epidemiologic studies depression (CES-D) scale in military peacekeepers. Depress Anxiety. 2003;17(1): 19-25. [ Links ]
36. Byrt T, Bishop J, Carlin JB. Bias, prevalence and kappa. J Clin Epidemiol. 1993;46(5): 423-9. [ Links ]
37. Streiner DL. Diagnosing tests: using and misusing diagnostic and screening tests. J Pers Assess. 2003;81(3): 209-19. [ Links ]
38. Cortina JM. What is coefficient alpha? An examination of theory and applications. J Appl Psychol. 1993;78:98-104. [ Links ]
39. Floyd FJ, Widaman KF. Factor analysis in the development and refinement clinical assessment instruments. Psychol Assess. 1995;7:286-99. [ Links ]
40. Gorsuch RL. Exploratory factor analysis: its role in item analysis. J Person Assess. 1997;68(3): 532-60. [ Links ]
41. Guarnaccia PJ, Angel R, Worobey JL. The factor structure of the CES-D in the Hispanic Health and Nutrition Examination Survey: the influences of ethnicity, gender and language. Soc Sci Med. 1989; 29(1):85-94. [ Links ]
42. Nguyen HT, Kitner-Triolo M, Evans MK, Zonderman AB. Factorial invariance of the CES-D in low socioeconomic status african americans compared with a nationally representative sample. Psychiatry Res. 2004;126(2): 177-87. [ Links ]
43. Brown C, Schulberg HC, Madonia MJ. Clinical presentations of major depression by african americans and whites in primary medical care practice. J Affect Disord. 1996;41(3):181-91. [ Links ]
44. Iwata N, Turner RJ, Lloyd DA. Race/ ethnicity and depressive symptoms in community-dwelling young adults: a differential item functioning analysis. Psychiatry Res. 2002;110(3):281-9. [ Links ]
45. Escobar JI, Gomez J, Tuason VB. Depressive phenomenology in north and south american patients. Am J Psychiatry. 1983;140(1): 47-51. [ Links ]
46. Pignone MP, Gaynes BN, Rushton JL, Burchell CM, Orleans CT, Mulrow CD, et al. Screening for depression in adults: a summary of the evidence for the U. S. Preventive Services Task Force. Ann Intern Med. 2002;136(10):765-76. [ Links ]
47. Medow MA, Borowsky SJ, Dysken S, Hillson SD, Woods S, Wilt TJ. Internal medical residents’ ability to diagnose and characterize major depression. West J Med. 1999;170(1):35-40. [ Links ]
48. Greenfield SF, Reizes JM, Magruder KM, Muenz LR, Kopans B, Jacobs DG. Effectiveness of community-based screening for depression. Am J Psychiatry. 1997;154(10): 1391-7. [ Links ]
49. Flores-Gutiérrez MY, Páez F, Ocampo- Castañeda J, Corona-Hernández F. Medicine student and medical professional knowledge about depressive syndrome (In Spanish). Salud Mental 2002; 23: 12-17. [ Links ]
50. Mojtabai R. Diagnosing depression and prescribing antidepressants by primary care physicians: the impact of practice style variations. Mental Health Serv Res. 2002;4(2):109-18. [ Links ]
Recibido para evaluación: 19 de junio de 2007 Aprobado para publicación: 22 de agosto de 2007














