Introduction
Violent behaviour perpetrated by individuals with severe mental illnesses has been recognised since ancient times1,2 and is a focus of attention for both the general public and academic community. However, although mental illness, and in particular schizophrenia, have been associated with a greater risk of violent behaviour compared to the general population, most individuals suffering from mental illness are not dangerous.3-5
In Colombia, the 2003 National Study of Mental Health showed a lifetime prevalence of mental illness of 36.4%, with a prevalence of 27% in Medellín.6 Besides violence,7 mental illness has been associated with various negative outcomes, such as higher rates of mortality due to general disease, suicide, poverty, marginalisation and stigmatisation.8-10 The risk of violent behaviour in mentally-ill patients has been associated with substance abuse, psychotic symptoms, lack of treatment adherence and poor mental illness awareness.11,12 When a crime is committed in a mental illness context that nullifies the perpetrator's capacity to understand the nature and consequences of his/her actions, he or she is deemed unfit to plead.13,14 Under the Colombian criminal code, criminal liability does not apply to those who are unfit to plead due to mental illness, but it does propose custodial and non-custodial measures for these patients. Internment in a suitable mental health institution or clinic is one such custodial measure, where patients receive psychiatric treatment and support.15,16
In Colombia, few studies have been conducted on mentally-ill patients who commit crimes.17 The objective of this study is the socio-demographic, clinical and legal characterisation of a group of patients deemed unfit to plead and institutionalised at a secure psychiatric institution.
Methods
A retrospective, descriptive, observational study, with a secondary information source. The reference population constituted 117,528 inmates who in 2013 were detained at 138 detention facilities in Colombia. Of these, 0.3% were unfit to plead.18 The sample comprised all patients admitted to the Psychiatry Department of the San Juan de Dios Clinic in La Ceja, Antioquia who were deemed unfit to plead between December 2000 and December 2013. Many of these patients are no longer interned at the institution because they either served the sentence imposed, ran away or died. These percentages are clarified in the descriptive analysis.
The San Juan de Dios Clinic is a private institution located in the Antioquia department in northern Colombia that provides psychiatry services to the Colombian Penitentiary and Prison Institute (INPEC) in order to provide treatment to patients deemed unfit to plead due to mental illness. The impunity of the patients admitted during the study period was determined by a judge from the Colombian legal system and the psychiatric diagnoses were obtained through an unstructured clinical interview conducted by clinical psychiatrists, who followed the diagnostic criteria of the Diagnostic and Statistical Manual (DSM)-IV-TR.19
Socio-demographic variables (age, gender, education, marital status, place of birth and origin), clinical variables (psychiatric diagnosis, medical comorbidities, psychiatric treatments, other medical treatments, use of toxic substances) and legal variables (type of crime, previous convictions, read-mission as unfit to plead) were included. For all the study variables, the required information was obtained and the unit of analysis was the patients who were unfit to plead. One of the research psychiatrists, who works as a psychiatrist within the Colombian Comprehensive Rehabilitation Programme (CRP), designed and produced the database. Qualitative variables were described with absolute and relative frequencies, while the median [interquartile range] was used for age due to the fact that the variable did not present normal distribution. Although the study is descriptive, associations between the type of crime and the other variables were investigated. To that effect, the x2 test of independence was used to compare the variables.
Association was explored using the OR, considering statistical association when p is <0.05 and there is a 95% confidence interval (95% CI). For the data analysis, the SPSS software, version 21.0 (SPSS Inc., Chicago, IL, USA), licensed to CES University, was used. This study is classified, in accordance with Article 11 of Ministry of Health Resolution 008430/1993, as "risk-free" research, as it uses a secondary source to obtain information; the results were approved by the CRP Committee of the San Juan de Dios Clinic in La Ceja, Antioquia, which safeguards ethical matters in research projects performed on this population. Moreover, the research protocol was assessed by the Research Committee of CES University, which did not request assessment by the University's Ethics Committee due to being a research project with a secondary information source.
Results
Descriptive analysis
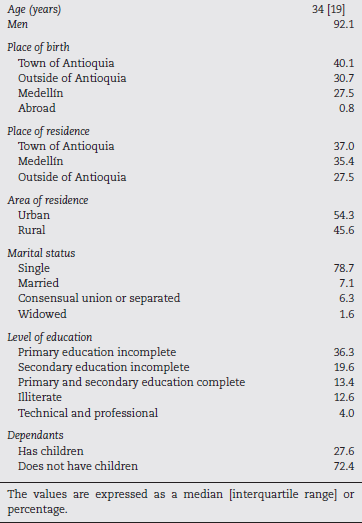
The final analysis included 127 patients deemed unfit to plead. The median age was 34 [19] years; however, there were patients as young as 17 and as old as 80, which reflects the age of the first psychotic breakdown and the stability of clinical symptoms in time. 117 patients (92.1% of the study population) were men; the remaining 7.8% are the 10 women included in the study. 40.15% of the patients were born in a town in Antioquia, which represents a good percentage of the population native to the rural area of the department where the study was performed; 27.5% were native to the urban area of Antioquia, represented by Medellín; and it was also found that 30.7% of the patients were born outside of Antioquia, with 0.8% coming from abroad. As regards the place of residence, the majority came from a town in Antioquia (37.0%), while the others were from Medellín (35.43%) and outside of Antioquia (27.55%). When they committed their respective crimes, the majority of the patients (54.3%) were living in an urban area. The most common level of education in this group of patients deemed unfit to plead was incomplete primary education (36.2%), followed by incomplete secondary education (19.68%). Strikingly, 12.6% had received no education whatsoever. The majority of the patients deemed unfit to plead were single (78.7%) followed by married (7.1%), in a consensual union or separated (6.3%), and widowed (1.6%) (Table 1).
Clinical variables
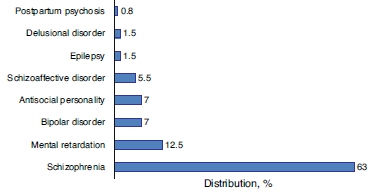
Impunity due to schizophrenia was determined in 53.5% of cases. The psychiatrists from the institution where they were interned confirmed the diagnosis in 63% of patients. This was followed by mental retardation (12.1%) (Fig. 1).
92.9% of the patients received treatment with antipsychotics. The majority (81.3%) were administered treatment with typical antipsychotics. Moreover, 35.4% of the patients received depot (long-acting injectable) antipsychotics. Other psychotropic drugs used were benzodiazepines (19.7%), antidepressants (14.3%) and anticonvulsants (3.8%). 18.1% of the patients deemed unfit to plead presented general medical comorbidities. As regards the use of toxic substances, 74.8% of the patients smoked, 66.9% consumed alcohol and 58.3% were using some form of drug prior to hospitalisation.
Legal variables
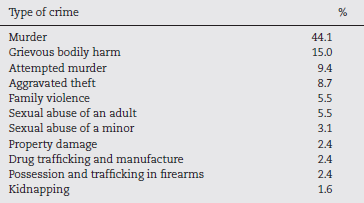
29.1% of the patients deemed unfit to plead had previous convictions. However, when broken down by diagnosis, it was found that 55.5% of the antisocial patients had previous convictions, 37.5% of the bipolar patients, 29.6% of the schizophrenic patients, 28.5% of the patients with schizoaffective disorder and 18.7% with mental retardation; the patients with delusional disorder, postpartum psychosis and epilepsy had no previous convictions. In this sample of patients deemed unfit to plead, the most prevalent type of crime that led to the imposition of the internment measure was murder (44.1%), followed by grievous bodily harm (15.0%) (Table 2). 50.3% of the victims had some degree of kinship with the patient and 19.6% were people with whom the patient was acquainted. The minimum internment was 10 months and the maximum, 40 years. During the internment, 4.7% of the patients ran away and the same percentage were readmitted as unfit to plead due to repeat offences. Only one patient died during hospitalisation due to non-psychiatric medical reasons.
Bivariate analysis
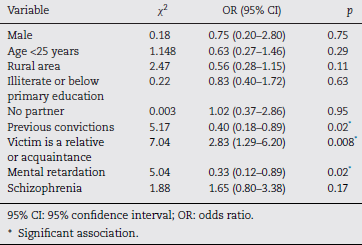
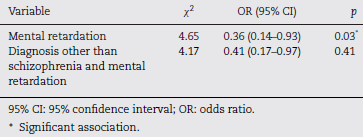
Although the main objective of the study did not involve a bivariate analysis, some variables intersected each other seeking association. The "type of crime" variable was recategorised, "murder" was grouped together with "attempted murder" (murderous conduct) and then this was compared with the other study variables. A statistical association was only found for the following variables: (a) having no previous convictions (X2 = 5.177; OR = 0.40; 95% CI, 0.18-0.89; p = 0.31), and (b) the victim being a relative or acquaintance (X2 = 7.046; OR = 2.83; 95% CI, 1.29-6.02; p = 0.01). The "victim is a relative or acquaintance" variable was grouped together and compared to "schizophrenia diagnosis" and "other diagnosis besides schizophrenia and mental retardation", and it was found that having schizophrenia is a risk factor for the victim being a relative or acquaintance (X2 = 11.58; OR=3.81; 95% CI, 1.73-8.41; p = 0.001). Mental retardation is a protective factor against the victim being a relative or acquaintance (X2 = 4.65; OR = 0.36; 95% CI, 0.14-0.93; p = 0.03). Tables 3 and 4 show the results of the bivariate analysis.
Discussion
127 patients deemed unfit to plead were characterised legally, clinically and socio-demographically. The common denominator of the cases was the simultaneity of the mental disorder and criminal conduct. 51.8% of all the Colombian inmates in the study period were aged between 30 and 44 years and 93.1% were male, consistent with the findings of another study.18 As regards the level of education, it was found that, among the study subjects, there was 1.3 times more illiteracy and a smaller proportion of subjects with a basic primary education than that stated in reports on the Colombian prison population from the same period (5.4% illiterate and 58.3% with an incomplete primary education).
In this study, the main psychiatric diagnosis is schizophrenia, which contrasts with the information reported in a meta-analysis of 62 studies which included 23,000 general criminally liable prisoners, where antisocial personality disorder was the most common, affecting 40-70% of cases.20 The prevalence of schizophrenia is estimated at less than 1% of the general population, but schizophrenics commit murder in 5-20% of cases.21-25 This strong association between schizophrenia and murder is consistent with the observations of this study, where schizophrenics committed the majority of the murders. The average incidence of murders committed by mentally-ill patients has been estimated at 0.13/100,000/year.16,26 However, according to Eronen et al., 27 the risk of schizophrenic patients of either gender committing a murder was 10 times higher than the general population, and the risk increased a further seven-fold when associated with alcohol consumption. In this study, it was found that 7 in 10 patients were drinking alcohol at the time of the crime, and the majority of the murderers had schizophrenia.
Another link studied between mental illness and criminality is related to the fact that schizophrenic subjects are 3.8 more likely to have a criminal record for third-party assault.28 In the patients under study, it was found that 1 in 3 schizophrenics had previous convictions.
A meta-analysis performed by Nielssen et al.29 in 2010 found that 4 in 10 murders committed by people with psychotic disorders were committed before the patient started receiving treatment for their psychosis, and that the murder rate for psychotic patients prior to treatment is approximately 15 times higher than the annual rate observed post-treatment. In this study, we did not have the information needed to establish whether the schizophrenic patients had already been diagnosed and treated before committing the crime.
It has been established that, worldwide, the age at onset of schizophrenia falls within the 17-35 year bracket, with medians of 22-23 years.30 The median age in this study's schizophrenia group was 36 years and 46.9% of the schizophrenic patients were older than 35 years, thus making it likely that they were not diagnosed or treated until after they had committed the crime. This idea is also supported by the fact that, in Colombia, the mental disorder treatment gap is 86.1%,31 one of the highest figures in Latin America and the Caribbean.
The types of crime most commonly committed by the Colombian prison population include theft (18.2%) and murder (16.8%). However, in our study murders accounted for almost half of all crimes, followed by personal injuries.
Most of the victims of the murders committed by schizophrenic patients were relatives,32,33 which coincides with this study's findings, where having schizophrenia was significantly associated as a risk factor for the murder victim being a relative or acquaintance. Mental retardation, on the other hand, served as a protective factor against the victim being a relative or acquaintance.
Finally, the findings of this study must be considered in light of the following methodological limitations. Firstly, insufficient socio-demographic, clinical and legal information was available on the patients for various reasons: (a) the patients were referred by the criminal system to the psychiatric institution with very little information; (b) despite psychiatric treatment, the patients provided limited clinical information; and (c) during hospitalisation, there were very few visits by relatives or friends to provide relevant clinical information on the patients. Secondly, although the diagnoses were performed by two clinical psychiatrists with ample experience in managing psychiatric hospital patients, no structured interviews or assessment scales were used to verify the diagnoses. Nevertheless, despite these limitations, this study provides valuable socio-demographic, clinical and legal information on patients deemed unfit to plead in Colombia.
Conclusions
The results obtained in this research project do not stray significantly from the characterisations of patients deemed unfit to plead performed in other countries, although this type of study does not allow general conclusions regarding the prevalence of diagnoses in patients deemed unfit to plead to be made, nor does it establish accurate comparisons between the general and prison population. This aspect has not yet been studied in Colombia, the characteristics and baseline conditions of which are different to populations in other countries. Even so, this study clearly reveals a profile that shows the typical patient deemed unfit to plead at the San Juan de Dios Clinic in La Ceja to be a young, single adult male with a low level of education, substance abuse and a schizophrenia diagnosis, who commits the crime under the influence of psychotic symptoms, and who achieves symptom stability if he undergoes treatment; the majority of patients do not reoffend and the main victims of the act committed are relatives. In general terms, these descriptions are consistent with the analyses and clinical impressions of the psychiatrists, who tend to believe that psychotic patients are those most at risk of assaulting third parties. Thus, in addition to studies that analyse services for patients deemed unfit to plead, new studies are needed that involve incarcerated patients in Colombia. We could therefore argue that decreasing the gap in the diagnosis and treatment of mental disorders might be among the practical measures for preventing violence associated with mental illness.