Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista de la Facultad de Medicina
Print version ISSN 0120-0011
rev.fac.med. vol.59 no.3 Bogotá July/Sept. 2011
Investigación original
Treatment of gestational syphilis and prevention of congenital syphilis in a public hospital in Bogotá, 2010
Nayibe Vanegas-Castillo1, Yenny Nataly Cáceres-Buitrago1, Carlos Augusto Jaimes-González1, Edith Ángel-Muller2, Jorge Andrés Rubio-Romero3
1 Médico Especialista en Obstetricia y Ginecología. Universidad Nacional de Colombia, Bogotá.
2 Profesora Asociada, Departamento de Obstetricia y Ginecología, Facultad de Medicina, Universidad Nacional de Colombia, Bogotá.
3 Profesor Asociado, Departamento de Obstetricia y Ginecología, Facultad de Medicina. Instituto de Investigacionse Clínicas, Universidad Nacional de Colombia, Bogotá.
Correspondencia: nayivanegas@hotmail.com
Introduction
Syphilis is an infection which is caused by Treponema pallidum, forming part of the group of sexually transmitted infections (STI) and making it one of the main worldwide diseases. It brings with it economic, social and sanitary consequences leading to large-scale repercussions. Syphilis can affect expectant mothers and transmit itself to their foetuses, having a negative impact on maternal health and on HIV/AIDS transmission; it has been calculated that the risk of contracting the infection due to HIV is twice to five times greater in patients suffering from syphilis (1,2).
The Pan-American Health Organisation (PAHO) has proposed the challenge of eliminating congenital syphilis, setting a target incidence rate (including neonatal deaths) of less than 0.5 cases per 1,000 births. To achieve such goal it is vital that more than 95% of infected expectant mothers are detected and treated, thereby managing to reduce syphilis prevalence during pregnancy to at least 1,0% (1).
Gestational syphilis (GS) is that which is diagnosed during pregnancy, post-abortion or the immediate puerperium and which may be found in any of its phases, being the indeterminate latent phase the most frequently encountered. The general obstetric background for a woman suffering from syphilis who has not received treatment (Kassowitz's law) (2) establishes that when the first pregnancy end in abortion or neonatal death; subsecuent pregnancies end in full-term neonates having congenital syphilis and finaly neonates not being affected by the disease in latter pregnancies.
If a mother becomes infected during the first weeks of her pregnancy then severe foetal damage is caused and a small percentage end in spontaneous abortion. If she becomes infected after week 16 of pregnancy this leads to abortion in 25% of cases, neonatal death in 25% or congenital infection in around 50% of cases and only a small percentage will be born healthy. Infection of a mother at the end of her pregnancy results in transmission to her foetus, up to 60% of them being born asymptomatic.
Congenital syphilis (CS) occurs when a mother suffering from syphilis transmits the infection to her foetus during pregnancy, whether through hematogenous-transplacentary route or during birth due to the neonate coming into contact with lesions on the mother's genitalia. Clinical lesions form from the 16th week of pregnancy onwards when the immune system has developed, even though the treponaema may pass into foetal circulation since the ninth week. At least two thirds of neonates from de women with untreated syphilis become infected (2). However, the risk of infection for the foetus o neonate varies considerably according to the state of maternal syphilis (2): 70% in primary syphilis, 90 to 100% en secondary syphilis, 30% in early latent syphilis and 20% in the late latent stage.
The fundamental principle for preventing/ eliminating CS consists of detecting and treating the infection in the expectant mother to prevent vertical transmission (3). It has been estimated that of all untreated expectant mothers with syphilis, only 20% will reach the end of their pregnancies and give birth to a normal newborn.
The complications include spontaneous abortion, neonatal death, non-immune foetal hydrops, intrauterine growth retardation, premature birth, perinatal death and serious consequences in those who survive. It can lead to intrauterine death in 30%, neonatal death in 10% and neonatal disorders in 40% (1,2).
Even though its incidence has been spectacularly reduced since 1946 with treatment involving penicillin, syphilis incidence has become intensified throughout the whole world since the end of the 1970s, as a result of important sociocultural changes (4). The incidence rate has fallen in most developed countries during the last few decades, but it has remained stable or increased in developing countries and in industrialised countries' most vulnerable population groups (5-11).
Some variables clearly influence the decision for neonatal treatment, such as documented syphilis in the mother, suitable maternal treatment, clinical, paraclinical or radiological evidence of neonatal syphilis and comparing the mother's serological titre to those of her newborn, ideally using the same non-treponemal test.
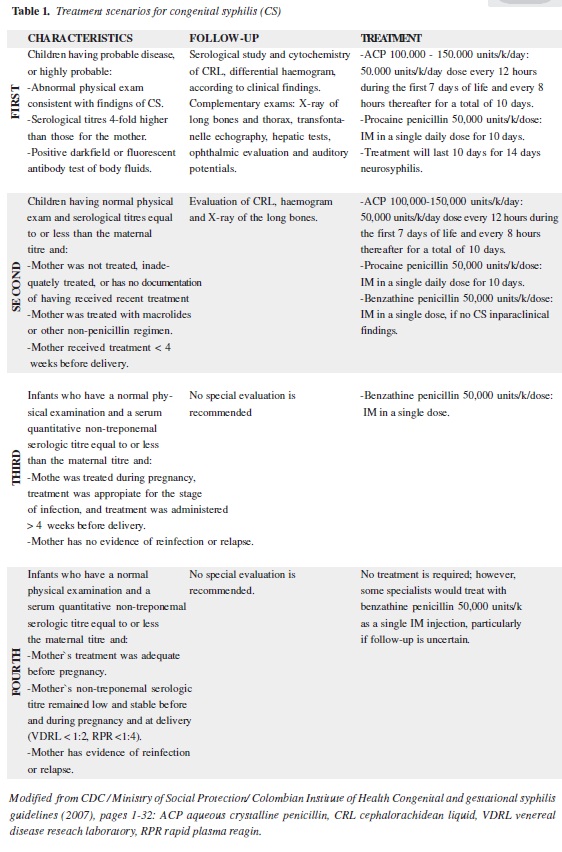
In 2006, the Centre for Disease Control (CDC) in Atlanta proposed four clinical scenarios for evaluating and managing newborn with congenital syphilis. These scenarios were adopted by the Instituto Nacional de Salud (INS) in 2007 (12,13) in the "Syphilis in pregnancy and Congenital Syphilis Protocol"(Table 1).
The identified groups at greater risk are: drug-dependent, populations having limited access to medical consultation, groups having had very early sexual initiation, low educational level, cities having growing prostitution amongst young people and low socioeconomic level and HIV-positive patients. In this latter group, the disease has greater virulence, its more difficult to treat (14,15) and it is also considered to be a facilitator of HIV transmission and its acquisition, due to the epidemiological parallelism of both complaints (16).
Amongst the factors contributing to CS persistence as a public health problem it is worth mentioning the presencie of barriers to access to prenatal care services and/or late access to it, lack of trained personnel, difficulty for treating and following-up expectant mothers and their partners and the stigma and discrimination related to STd`s (1,17).
Colombia continues to be a country having higher CS figures than PAHO's proposed goal. Thus, recognising the great impact on public health of these figures, the present study was undertaken to describe the current situation regarding GS and CS screening, diagnosis, treatment and follow-up in a public hospital in Bogotá, evaluating the treatment received by patients suffering from CS and GS and describing the difficulties currently affecting integral management of the disease.
Materials and methods
Design
This was a retrospective descriptive study based on notification registies and clinical records of expectant mothers and newborns having a diagnosis of syphilis who had been identified during prenatal control, birth or post-natal period, between the 1st of January and 31st of October 2010.
The study was designed and followed the guidelines provided in Colombian Ministry of Social Protection resolution No. 008430 of 1993. The expectant mothers and the newborns were identified from obligatory notification index cards regarding cases reported during prenatal control, hospitalization and delivery rooms. The clinical histories were reviewed and the relevant information was obtained for the purpose and objectives of the study.
Population and place
The clinical records of the expectant mothers and newborns diagnosed as having syphilis were included. The study was carried out in a public institution which attends patients from contributory and subsidised healthcare regimes and those covered by the Colombian social security scheme, characterised by providing attention to obstetric patients and those having socioeconomic conditions involving greater vulnerability such as poverty and prostitution.
Definitions of variables
Gestational syphilis: any pregnant women who have just given birth or who have had a recent abortion with clinical evidence (genital ulcer or lesions compatible with secondary syphilis) and/ or a positive or reactive treponemal (including rapid treponemal tests) or non-treponemal test who have not received suitable treatment for syphilis during their present pregnancy or who became re-infected and did not receive adequate treatment (1). This definition, described by PAHO was prefered over the colombian's Instituto Nacional de Salud (2007) definition, as it includes patients for whom adequate treatment and/or re-infection had not been documented.
Confirmed gestational syphilis: a pregnant women who have just given birth or who have had a recent abortion with reactive non-treponemal test greater than or equal to 1:8 dilutions or a lower dilution with a positive treponemal test (18).
Probable case of congenital syphilis: all abortions, live or dead newborns from women having clinical evidence or positive reactive non-treponemal or treponemal tests during pregnancy, birth or puerperium who have not been treated or who have been inadequately treated and who have presented one or more of the following factors:
-Having had another STI during their pregnancy;
-Not having had serological follow-up after treatment or that this had been inappropriate;
-Not having reported contacts; and
-Having presented a deficient serological response certified by therapeutic response.
Newborn having one of the following:
-Venereal disease research laboratory/rapid plasma reagin (VDRL/RPR) serological result reactive up to 1:4 titres;-Positive CS clinical, laboratory and radiological criteria regarding the newborn;
-VDRL titres four times higher in the child than the mother or the equivalent of a change in two or more dilutions of maternal titres (2); and
-Specific reactive IgM.
Confirmed case A: probable case in which an increase has been detected in two or more initial titre dilutions less than 1:8 during follow-up. Newborn complying with the following conditions:
-Presenting any reactive syphilitic test regarding the cerebrospinal fluid (CSF); and
-Identification of T. pallidum by darkfield microscope, direct fluorescence or other special staining allowing it to be identified in lesions from the neonate, placenta, umbilical cord or autopsy material.
Child older than seven months: reactive treponemal and non-treponemal tests. Clinical evidence of syphilis: the presence of hepatosplenomegaly, cutaneous-mucosal lesions (reddish infiltrated papules and pustules in the perioral región, on tñe limbs, palms, soles, perianal and perigenital regions), osteochondritis, periostitis, radiolucid bands in bones, mucopurulent rhinitís, pseudoparalysis, jaundice or anaemia (9).
Confirmed case B: newborn having signs and symptoms compatible with congenital syphilis who could not be followed-up and for whom laboratory tests could not be made.
Compatible case: asymptomatic newborn classified as a probable case who could not be followed-up and for whom laboratory tests could not be made.
Complete evaluation of the newborn: it was considered when all of the following diagnostic tests had been done: complete physical exam, haematic picture, uriñe sample, long bone radiography and of the thorax, cytochemistry of the CSF, VDRL in blood and CSF, hepatic and renal function tests (12).
Consistency of formulated neonatal treatment: the pertinence of the formulated treatment according to CDC clinical scenario (13).
Statistical analysis
Data from the clinical records was collected manually and recorded on a form and then tabulated in a datábase created in Excel (2007 versión).
The information was summarised in percentages for qualitative variables and in means and averages for continuous variables, according to their distribution.
Results
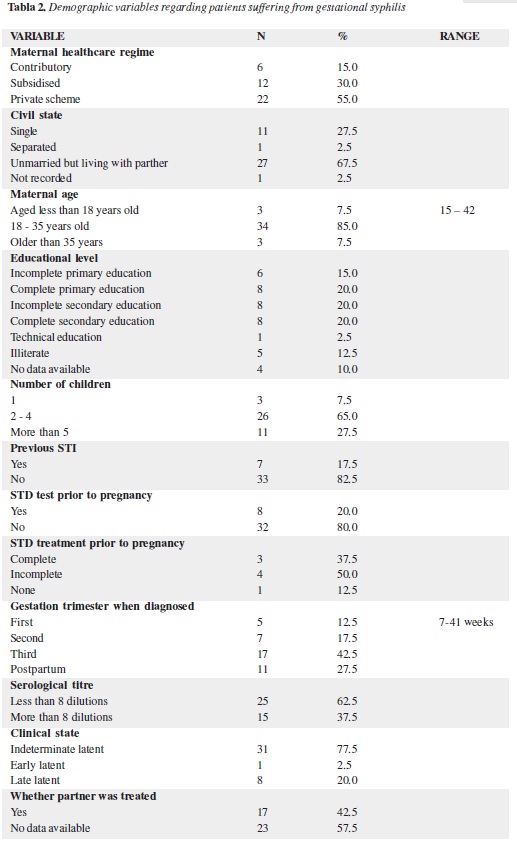
A total of 2,945 live births and 310 abortions took place during the study period and 65 obligatory notifications for syphilis were filled in: 40 for GS and 25 for CS. In the cases of GS, five had a background of abortion (4 early and one late abortion associated with holoprosencephaly) and five expectant mothers treated during prenatal control (2 during the first trimester, 1 in the second trimester and 2 in the third trimester). Twenty-nine (72.5%) expectant mothers were diagnosed during labour and one during the immediate puerperium, whose birth and newborn were attended at another institution.
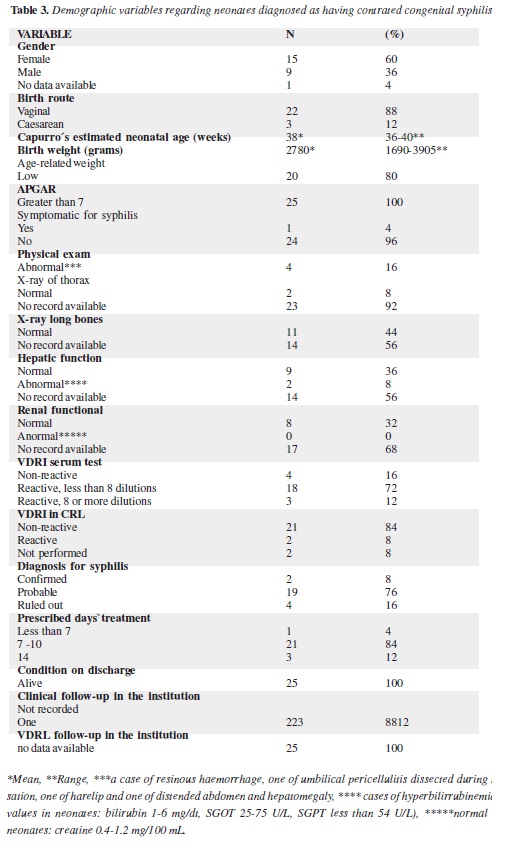
Out of the 29 patients diagnosed during labour and the one during the puerperium, only 25 clinical histories of their newborn infants could be found to be included in the analysis. One was born and hospitalised in another institution and no information was obtained concerning the remaining four neonates. Table 2 shows the demographic characteristics of the women diagnosed as having GS and Table 3 the demographic characteristics of the newborns who were followed-up and treated. It was found that 20% of the patients had a background of syphilis being diagnosed prior to their pregnancy and only 37.5% of them had received a complete treatment. Of the six patients identified as having had an abortion, one (16.6%) had attended prenatal control and received treatment for GS; the five remaining women were diagnosed during their hospitalisation for abortion.
All patients were classified as being in the latent stage and received treatment with an initial dose of benzathine penicillin when discharged. There were no records in the clinical histories concerning follow-up procedures: it they had their next doses administered, the change in the the nontreponemal titres (if they received next doses) or if their sexual partners' received treatment.
Four expectant mothers were found during prenatal control by the study cut-off date and received treatment consisting of three doses of benzathine penicillin. During the observation time it was possible to document the serological follow-up and negativisation of VDRL titres in one of them. Foetal compromise was not seen in any of these women.
Of the 30 patients identified during labour and the puerperium by non-treponemal tests and confirmed by treponemal tests, none showed clinical evidence of the disease. Twenty of them (66%) were not diagnosed or treated during their pregnancy; six had received incomplete dosage schemes and only four complete treatment, one of them with an aqueous crystalline penicillin (ACP) dosage scheme lasting 14 days. From the mothers who had received complete treatment, three newborns were treated for 10 days with a ACP dosage scheme (1 newborn with hepatomegaly and oedema of the abdominal wall with reactive VDRL, one with reactive VDRL and normal clinical exam and one with non-reactive VDRL and normal clinical exam). Neurocongenital syphilis was ruled out in the newborn infants from these four women.
One woman presented coinfection with HIV and her newborn was treated as in scenario 1 and also received complete prophylaxis for HIV.
On being discharged, all the women were prescribed treatment consisting of 3 doses of 2,400,000 UI benzathine penicillin. No data was available regarding either the maternal or neonatal clinical records referring to the administration of antibiotics after leaving the hospital or any record of their compliance with the proposed schemes.
Women's prenatal care records under-register the changes of the serological titres from the non-treponemal tests, thereby hampering the estimation of the effectiveness of the formulated treatment or its flaws during pregnancy.
Table 3 gives the characteristics of the notified neonates. Twenty-five newborn infants were classified as probable cases of CG and were treated; 23 of them were found to be asymptomatic and free of clinical findings orientating an early diagnosis. The presence of neurosyphilis was confirmed in 2/24 (8.3%) of the asymptomatic newborn infants; they received 50,000 units/k/dose intravenous ACP every 12 hours for 14 days. Clinical and epidemiological criteria ruled out CG in one case.
The newborn treated for probable and confirmed disease left the institution in good condition and completed the parenteral antibiotic scheme.
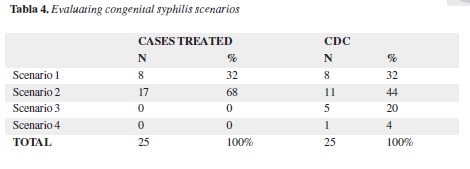
On analysing the clinical records of the expectant mothers and their newborn in line with the scenarios proposed by CDC and adapted by the Instituto Nacional de Salud regarding standards for treating CS, it was found that 100% of the cases were treated as scenario 1 and 2. Of them, 24% could have been candidates for a single dose of benzathine penicillin (scenarios 3 and 4), as shown in table 4.
No cases of maternal or perinatal syphilis-related mortality were presented. There was one foetal
death (a late abortion) that had a major malformation (semilobar holoprosencephaly) without a direct association with the diagnosis of syphilis. There were no cases of neonatal mortality and all newborn infants left the institution alive. There was no data in the clinical records regarding, treatment, clinical or serological follow-up of the mothers or their neonates' after their hospitales withdrawal.
Discussion
The present study provided an overview of gestational and congenital syphilis diagnosis, treatment and follow-up, showing that the disease continúes to affect highly vulnerable populations (low socioeconomic level, poverty, drug de-pendence) (19), leading to adverse conditions hampering integral management. However, it was not possible to make a complete evaluation of maternal socioeconomic conditions, such as social strata and occupation, due to the lack of data in the clinical records.
Late access to maternal healthcare was noticeable regarding congenital disease incidence. Most GS cases were diagnosed when the mother was admitted to give birth or underwent an abortion, many of them coinciding with expectant mothers' first access to healthcare services. Likewise, the users' lack of knowledge regarding the disease could have influenced this. The foregoing situation determined that neonates were given preferential or "excessive" management regarding to the antibiotic treatment scheme, as it was considered that the mothers' individual conditions did not guarantee that they, their sexual partners and much less their newborn would receive suitable treatment and strict follow-up and supervision in an outpatient basis.
Healthcare workers recognise that screening patients who attend prenatal care and providing them attention when they give birth is a dynamic process. Patients are subjected to treponemal tests with reactive non-treponemal tests according to the institutional protocols and national maternal clinical guidelines. The diagnostic challenge lies in patients having had prior disease, lacking treatment, having been partially treated or where there is insufficient information in the clinical records.
The recommended and most widely implemented management scheme uses benzathine penicillin according to clinical state, reserving the use of ACP for cases of neurosyphilis and tertiary syphilis (2,18,20).
The conduct defined and practised for GS in this institution was in line with national and international recommendations for the stages of the disease found here. However, there is a lack of information in the clinical records regarding the dose and scheme of treatment supplied to these patients and to their sexual partners during out-patient follow-up and also there is a problem of under-recording data in the institutional registries.
The diagnosis of CS continues to be based on the clinical probability of having the infection (based on the characteristics of maternal infection and the treatment so established) and on non-treponemal test results. As reported in the literature, it is hard to routinely find clinical signs that lead to the diagnosis of CS in neonates.
It was also found that there was no uniformity regarding applying/requesting paraclinical studies for the newborn apart from non-treponemal tests. No radiological or blood chemistry tests were performed in this study for suspected CS cases and no alterations were reported in the tests which were carried out.
Uncertainty regarding a definitive diagnosis of CS leads to the probable cases being over-treated, as shown in table 4, where 24% of neonates received dosage schemes for CS when scenarios 3 and 4 according to CDC classification were probably being dealt with, only requiring a single dose of procaine penicillin. The long-term effects nor the possible advantages and disadvantages of such conduct cannot be determined in this study, given that only information regarding the first month after birth was available and that there was no information in the institution about following-up the newborn after they had left the hospital.
It is proposed that each case of CS should be suitably classified according to the aforementioned scenarios in order to decrease the percentage of patients being classified in a higher risk scenario than they should really be and, thus, avoid them receiving over-treatment and unnecessary hospitalisation. Following-up neonates beyond their leaving hospital must be stressed since having simply received treatment does not guarantee total cure of the disease, above all in cases of neurosyphilis. Such follow-up should be continued at least until a child reaches the age of two.
The present study has weaknesses as it did not lead to determining CS incidence or the effectiveness of penicillin treatment schemes for preventing CS. Likewise, as it has been a descriptive and retrospective analysis based on notification records and clinical histories, it also has limitations due to bias regarding information, the difficulty involved in follow-up, suitable recording of the disease and the loss and lack of information and feedback that happens when patient are transferred between the different complexity levels of hospital attention in the Colombian state network.
An integral model should be promoted whose objective would be reporting cases of maternal and gestational syphilis, facilitating the collection of data and thereby the early diagnosis and treatment of the mother, following her up as well as her sexual partners and child until two years of age. Likewise, effectiveness of treatment during pregnancy and in neonates must be evaluated and communication and feedback strengthened at all levels of healthcare attention for expectant mothers and their children.
Eradicating the disease from our population also demands that pre-established standards must be complied with, that national policy must be directed towards improving socioeconomic conditions, the educational level of the underprivileged classes and carrying out educational campaigns focused on topics such as receiving and providing good treatment, family planning, prenatal care and knowledge about prevention and treatment of sexuallytransmitted diseases.
Conclusions
The fundamental principle in preventing and eliminating congenital syphilis is the detection and treatment of gestational infection for preventing its vertical transmission. An integrated healthcare attention approach must be conceived, directing medial know-how and interventions towards screening, diagnosing and providing the suitable treatment of pregnant women and not waiting for the infected newborn to be diagnosed and treated.
The following factors influencing GS and CS persistence in our population may be identified: late access to prenatal control, the population's lack of knowledge regarding the disease's impact on the foetus and neonate, the poor supervisión of compliance with treatment schemes and sexual contacts and the lack of institutional clinical follow-up through inter-institutional feedback activities between district healthcare entities.
Integrating clinical data regarding every newborn together with that regarding the mother will lead to the corresponding therapeutic scenario being properly located and optimise antibiotic treatment for each case. This could lead to reducing hospital stay, healthcare system costs, as well as those for its users and tend towards curing the disease.
Obligatory GS and CS notification activities must be strengthened to avoid under-recording and ensure the broadcasting of knowledge about the associated demographic factors, the difficulties emerging during diagnosis, treatment and follow-up and in implementing public health policy aimed at eliminating the disease of congenital syphilis.
The present work received an honourable mention in the Lafrancol Laboratory research awards, Bogotá, April 2011.
References
1. Valderrama J, Zacarías F, Mazin R. Sífilis materna y congénita en América Latina: un problema grave de solución sencilla. Revista Panamericana de Salud Pública. 2004; 16:211-217.
2. Berman SM. Maternal syphilis: pathophysiology and treatment. Bull Worid Health Organ. 2004; 82:433-8.
3. Rawstron SA, Bromberg K. Failure of recommended maternal therapy to prevent congenital syphilis. Sex Transm Dis. 1991; 18:102-6.
4. Lawrence RM, Lawrence RA. Breast milk and infec-tion. Clin Perinatol. 2004; 31:501-28.
5. Genç M, Ledger WJ. Syphilis in pregnancy. Sex Transm Infect. 2000; 76:73-9.
6. Deperthes BD, Meheus A, O'Reilly K, Broutet N. Maternal and congenital syphilis programmes: case studies in Bolivia, Kenya and South Africa. Bull World Health Organ. 2004; 82:410-6.
7. Chakraborty R, Luck S. Managing congenital syphi-lis again? The more things change... Curr Opin Infect Dis. 2007; 20:247-52.
8. Cheng JQ, Zhou H, Hong FC, Zhang D, Zhang YJ, Pan P, Cai YM. Syphilis screening and intervention in 500,000 pregnant women in Shenzhen, the People's Republic of China. Sex Transm Infect. 2007; 83:347-50.
9. Walker GJ, Walker DG. Congenital syphilis: a continuing but neglected problem. Semin Fetal Neonatal Med. 2007;12:198-206.
10. Rotchford K, Lombard C, Zuma K, Wilkinson D. Impact on perinatal mortality of missed opportunities to treat maternal syphilis in rural South Africa: baseli-ne results from a clinic randomized controlled trial. Trop Med Int Health. 2000; 5:11:800-4.
11. UNDP/World Bank/ WHO. Special programs for re-search and training in tropical diseases. The sexually transmitted diseases diagnostics initiative (SDI). SDI Report: Laboratory-based evaluation of rapid syphilis diagnostics. 2003.
12. Ministerio de la Protección Social, Instituto Nacional de Salud. Protocolo de Sífilis congénita y gestacional. 2007: 1-32.
13. Congenital Syphilis, Sexually Transmitted Diseases. Treatment Guidelines. Center for Disease Control and Prevention. 2006.
14. Walker GJ. Antibiotics for syphilis diagnosed during pregnancy. Cochrane Database Syst Rev. 2001; CD001143.
15. Vaules MB, Ramin KD, Ramsey PS. Syphilis In Pregnancy: a Review. Primary Care Update for OB/ Gyns. 2000; 7:26-30.
16. Joint United Nations Programme on HIV/AIDS. Con-sultation on STD interventions for preventing HIV: what is the evidence? Geneva; 2000 (UNAIDS/03.04E).
17. World Bank. World Development Report 1993: inves-ting in health. New York: World Bank. 1993.
18. Schmid G. Economic and programmatic aspects of congenital syphilis prevention. Bulletin of the World Health Organization. 2004; 82:402-409.
19. Rodríguez-Medina CL. Causas frecuentes de condiciones críticas de salud madre-hijo, en los hospitales universitarios de la Samaritana y del Valle entre febrero y junio de 2005. Rev fac med unal. 2008; 56:109-124.
20. Sheffield JS, Sánchez PJ, Morris G, Maberry M, Zeray F, McIntire DD, et al. Congenital syphilis after maternal treatment for syphilis during pregnancy Am J Obstet Gynecol 2002; 186:569-73.
1. Valderrama J, Zacarías F, Mazin R. Sífilis materna y congénita en América Latina: un problema grave de solución sencilla. Revista Panamericana de Salud Pública. 2004; 16:211-217. [ Links ]
2. Berman SM. Maternal syphilis: pathophysiology and treatment. Bull Worid Health Organ. 2004; 82:433-8. [ Links ]
3. Rawstron SA, Bromberg K. Failure of recommended maternal therapy to prevent congenital syphilis. Sex Transm Dis. 1991; 18:102-6. [ Links ]
4. Lawrence RM, Lawrence RA. Breast milk and infection. Clin Perinatol. 2004; 31:501-28. [ Links ]
5. Genç M, Ledger WJ. Syphilis in pregnancy. Sex Transm Infect. 2000; 76:73-9. [ Links ]
6. Deperthes BD, Meheus A, O'Reilly K, Broutet N. Maternal and congenital syphilis programmes: case studies in Bolivia, Kenya and South Africa. Bull World Health Organ. 2004; 82:410-6. [ Links ]
7. Chakraborty R, Luck S. Managing congenital syphilis again? The more things change... Curr Opin Infect Dis. 2007; 20:247-52. [ Links ]
8. Cheng JQ, Zhou H, Hong FC, Zhang D, Zhang YJ, Pan P, Cai YM. Syphilis screening and intervention in 500,000 pregnant women in Shenzhen, the People's Republic of China. Sex Transm Infect. 2007; 83:347-50. [ Links ]
9. Walker GJ, Walker DG. Congenital syphilis: a continuing but neglected problem. Semin Fetal Neonatal Med. 2007;12:198-206. [ Links ]
10. Rotchford K, Lombard C, Zuma K, Wilkinson D. Impact on perinatal mortality of missed opportunities to treat maternal syphilis in rural South Africa: baseline results from a clinic randomized controlled trial. Trop Med Int Health. 2000; 5:11:800-4. [ Links ]
11. UNDP/World Bank/ WHO. Special programs for research and training in tropical diseases. The sexually transmitted diseases diagnostics initiative (SDI). SDI Report: Laboratory-based evaluation of rapid syphilis diagnostics. 2003. [ Links ]
12. Ministerio de la Protección Social, Instituto Nacional de Salud. Protocolo de Sífilis congénita y gestacional. 2007: 1-32. [ Links ]
13. Congenital Syphilis, Sexually Transmitted Diseases. Treatment Guidelines. Center for Disease Control and Prevention. 2006. [ Links ]
14. Walker GJ. Antibiotics for syphilis diagnosed during pregnancy. Cochrane Database Syst Rev. 2001; CD001143. [ Links ]
15. Vaules MB, Ramin KD, Ramsey PS. Syphilis In Pregnancy: a Review. Primary Care Update for OB/ Gyns. 2000; 7:26-30. [ Links ]
16. Joint United Nations Programme on HIV/AIDS. Consultation on STD interventions for preventing HIV: what is the evidence? Geneva; 2000 (UNAIDS/03.04E). [ Links ]
17. World Bank. World Development Report 1993: investing in health. New York: World Bank. 1993. [ Links ]
18. Schmid G. Economic and programmatic aspects of congenital syphilis prevention. Bulletin of the World Health Organization. 2004; 82:402-409. [ Links ]
19. Rodríguez-Medina CL. Causas frecuentes de condiciones críticas de salud madre-hijo, en los hospitales universitarios de la Samaritana y del Valle entre febrero y junio de 2005. Rev fac med unal. 2008; 56:109-124. [ Links ]
20. Sheffield JS, Sánchez PJ, Morris G, Maberry M, Zeray F, McIntire DD, et al. Congenital syphilis after maternal treatment for syphilis during pregnancy Am J Obstet Gynecol 2002; 186:569-73. [ Links ]











 text in
text in