Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista de la Facultad de Medicina
Print version ISSN 0120-0011
rev.fac.med. vol.62 no.2 Bogotá Apr./June 2014
https://doi.org/10.15446/revfacmed.v62n2.45430
http://dx.doi.org/10.15446/revfacmed.v62n2.45430
Investigación original
Gestational and congenital toxoplasmosis in two hospitals in Bogota, Colombia
Toxoplasmosis gestacionaly congénita en dos hospitales de Bogotá, Colombia
Edith Angel-Müller1; María Paula Hougton2; Carolina Eslava2; Jorge Riaño2; Gustavo E. Rey2; Jorge E. Gómez-Marín3
1 Obstetrics and Gynaecology Department, Medicine Faculty, Universidad Nacional de Colombia, Bogotá, Colombia.
2 Instituto Materno Infantil, Hospital la Victoria, Bogotá, Colombia.
3 Grupo de Estudio en Parasitología y Micología Molecular (GEPAMOL), Biomedical Research Centre, Universidad del Quindío, Armenia, Colombia.
Correspondence: Edith Angel-Müller, Departamento de Obstetricia and Ginecología, Facultad de Medicina Universidad Nacional de Colombia, Bogotá, Colombia. Dirección: Calle 121 No. 53A-38, Teléfono: + 57 6377560. Correo electrónico: eangelm@unal.edu.co
Ángel-Müller E, Hougton MP, Eslava C, Riaño J, Rey GE, Gómez-Marín JE. Gestational and congenital toxoplasmosis in two hospitals in Bogota, Colombia. rev.fac.med. 2014;62:179-185.
Recibido: 20/04/2013 / Aceptado: 10/04/2014
Summary
Background. Gestational toxoplasmosis is acquired during pregnancy and involves a risk of the parasite crossing the placenta, thereby leading to foetal infection, which can lead to serious sequelae in children, mainly chorioretinitis, cerebral calcification, hydrocephalus and intellectual disability.
Objective. Determining the prevalence of maternal and neonatal toxoplasmosis in women attending the Engativa and La Victoria hospitals in Bogota, Colombia, for delivery. Correlating the results with those of a national multicentre study. Determining IgM and IgA anti-toxoplasma prevalence in newborn (NB) umbilical cord blood.
Materials and methods. This was a cohort study, which was approved by the participating institutions' ethics committees. The patients signed informed consent forms and filled out a survey requesting demographic and prenatal care data. A blood sample was taken from the umbilical cord on delivery for determining anti-toxoplasma IgM. Anti-toxoplasma IgA was also measured in a subset of patients. Children suspected of having either clinical or serological congenital toxoplasmosis were followed-up for 12 months.
Results. The study involved taking 3,224 NB umbilical cord blood samples between April 1st 2009 and July 16th 2010. Positive anti-toxoplasma IgG was found in 28.2% of pregnant women (26.1-29.8 95%CI). Anti-toxoplasma IgM was determined in 558 pregnant women and found positive in 34 patients (i.e. 1.1 per 100 NB gestational toxoplasmosis incidence). Nine blood samples were positive (7 for IgM and 2 for IgA). Five of the NB studied (0.15%) were positive for IgG after 12 months' follow-up, thereby confirming a diagnosis of congenital toxoplasmosis accounting for 1 in every 645 live births.
Conclusion. This study showed that 70% of the pregnant women were not infected with T. gondii in the chosen hospitals in Bogotá. Gestational toxoplasmosis frequency was around 1% and 0.6% for congenital toxoplasmosis.
Key words: Toxoplasmosis, Congenital; Pregnancy, Prevalence; Diagnosis (MeSH).
Resumen
Antecedentes. La toxoplasmosis gestacional es la adquisición de la enfermedad durante la gestación, con el riesgo de que el parásito atraviese la placenta and produzca una infección fetal, que puede llevar a importantes secuelas en el niño, principalmente coroidoretinitis, calcificaciones cerebrales, hidrocefalia and retardo mental.
Objetivo. Conocer la prevalencia de la toxoplasmosis materna and neonatal, de las mujeres que asistieron para la atención del parto, en los Hospitales Engativá and La Victoria, de Bogotá, Colombia y correlacionar los resultados con los del estudio multicéntrico nacional. Determinar la prevalencia de IgM and IgA en sangre de cordón umbilical de los recién nacidos (RN).
Materiales and métodos. Estudio de cohorte. El estudio fue aprobado por los comités de ética de las instituciones. Las pacientes firmaron el consentimiento informado y, posteriormente, se les diligenció el formato de recolección de datos, para conocer las características demográficas and los datos del control prenatal. En el parto, después del pinzamiento del cordón, se tomó una muestra de sangre de este, para determinar IgM antitoxoplasma y en un subgrupo de pacientes también se midió la IgA antitoxoplasma. Los niños con datos clínicos o serológicos sospechosos de toxoplasmosis congénita, se siguieron hasta los 12 meses.
Resultados. Se tomaron muestras de 3.224 RN, entre el 1 de abril de 2009 y el 16 de julio de 2010. En las gestantes se encontró IgG anti-Toxoplasma positiva en 28,2% (IC95% 26,1-29,8). Se determinó la IgM anti-Toxoplasma en 558 gestantes encontrando 34 positivas, calculando una incidencia de toxoplasmosis gestacional de 1,1 por cada 100 RN. Se estudiaron 3215 muestras de cordón umbilical y se encontraron nueve casos positivos (siete con IgM y dos con IgA). De los RN estudiados, cinco (0,15%) tuvieron resultado positivo de IgG al año de edad, con lo cual se confirmó el diagnostico de toxoplasmosis congénita; esto equivale a un diagnóstico de toxoplasmosis congénita en 1 de cada 645 nacidos vivos.
Conclusión. En este estudio se encontró que, en los hospitales de Bogotá estudiados, aproximadamente el 70% de las mujeres al momento de la gestación no se han infectado con el T gondii. La frecuencia de la toxoplasmosis gestacional es de aproximadamente 1% y la de toxoplasmosis congénita de 0,6%.
Palabras clave: Toxoplasmosis Congénita, Embarazo, Prevalencia, Diagnóstico (DeCS).
Introduction
Toxoplasma gondii is a parasite causing one of the most common parasitic infections in human beings. The parasite's vertical transmission in pregnant women may lead to significant morbidity and mortality for the foetus and the newborn and serious consequences regarding children's neurological and ophthalmological development.
Congenital toxoplasmosis is one of the Colombian health plan's priorities; it forms part of the objective aimed at improving children's health. It is also part of the policy for implementing a congenital anomalies surveillance system, emphasising German measles, syphilis and toxoplasmosis. This study is appropriate at a time when management of the disease is controversial and when data is needed which will hopefully provide answers for resolving such controversy.
Toxoplasma gondii infection is a worldwide zoonosis. Prevalence varies between geographical regions and seems to be related to people's eating and hygienic habits, thereby supporting the oral route as the most important transmission mechanism (1). Serological studies have shown that at least a third of the world's adult population has been infected by the parasite (2); this means that 1,000 to 2,000 million people are currently infected (3).
The largest study in Colombia concerning toxoplasmosis prevalence in the general population was carried out in 1982 (the Colombian Health Study) which calculate prevalence as being 47% (4). According to the study, prevalence increased with age and there were significant variations between regions. The highest prevalence was found on Colombia's Atlantic coast (63%) whilst prevalence in the central region was almost half this (36%). The risk of acquiring the infection was calculated as being 1.5% in females aged 10-15 years old and fell to 0.7% in the 40-44 year-old group (5).
Toxoplasmosis prevalence varies greatly regarding pregnant women; it is around 54% in France but only 12% in Sweden (6). Toxoplasma gondii seroprevalence for 15 to 55 year-old women in the USA is 15% (7), around 35% in México and 59% to 78% in Brazil (Sao Paulo, Rio de Janeiro) (8).
Primary infection incidence during pregnancy varies greatly from country to country, the average varying from less than 1 to more than 15 per 1,000 pregnancies. Incidence in European countries has been calculated as being 2.9 in Denmark, 3.4 in Holland and 8.1 in France per 1,000 susceptible pregnant women. A study of pregnant women in Quindío, Colombia, found around 1.9% incidence (5, 9).
Worldwide congenital toxoplasmosis prevalence in the newborn may vary from 1 to 10 per 10,000 live births, depending on the geographical area. This has been calculated as being 1/10,000 live births (LB) in Sweden, 3/10,000 LB in Brazil and 10/10,000 LB in France (9). It has been estimated that this could range from 2 to 10 per 1,000 LB in Colombia, representing 600 to 3,000 children born every year with congenital infection, 10% of whom die (i.e. 600 children die every year from this infection throughout Colombia, representing 3.7% of infant mortality in Colombia). These figures highlight the fact that congenital toxoplasmosis is a serious public health problem and represents one of the three main causes of prenatal infection (10).
It has been proposed that anti-Toxoplasma IgM and IgA should be measured in umbilical cord blood when a baby is born for diagnosing congenital toxoplasmosis. Studies have found sensitivity ranging from 28% for the ELISA test to 91% for the immunosorbent agglutination assay (ISAGA) and 78% specificity has been found for IgM (11,12); 54% sensitivity has been found for IgA in cord blood and 88% specificity for the ISAGA IgA test in the absence of specific IgM (11, 13). It is not known whether there are geographical variations regarding the presence of specific IgA in the absence of anti-Toxoplasma IgM.
No data is available reflecting the current situation in Bogotá. A 1998 study reported 47% prevalence for anti-Toxoplasma IgG antibodies in 637 maternal sera samples and 2.2% frequency in recently infected patients (according to criteria requiring the simultaneous presence of anti-Toxoplasma IgM and IgA) (14). It is not known which frequency rate (data has not been updated since 2010) has been used in current studies concerning toxoplasmosis during pregnancy or how many receive treatment or the correlation with figures from the Colombian multicentre study on neonatal toxoplasmosis (15).
This study's main objective was to ascertain maternal and neonatal toxoplasmosis prevalence in two hospitals in Bogotá, Colombia, and correlate the results with those from the Colombian multicentre study (April 2009 to July 2010).
The secondary objectives included describing this cohort of patients' demographic characteristics. They also included describing data regarding anti-Toxoplasma IgM and IgA prevalence in umbilical cord blood from a representative group of newborn from two hospitals in Bogotá obtained during the Colombian multicentre study and correlating this with data obtained from analysing the pregnant women's clinical histories. Another objective focused on ascertaining Toxoplasma IgG and IgM seroprevalence during pregnancy in the mothers of the newborn being studied.
Materials and methods
This was a cohort study. All patients going into labour at both target hospitals were invited to participate (consecutively) until sample size had been completed.
Ethical aspects. The study was approved by Hospital Engativa ESE ethics committee (memorandum CERE 08, 14th August 2009) and the Universidad del Quindio's ethics committee (minute 14, 23rd June 2008). It was considered that this study, which involved obtaining umbilical cord blood samples, was a risk-free procedure and that identifying infection would benefit any infected child. All the women who agreed to participate in the study signed an informed consent form.
Surveys. A questionnaire was completed for each participant which asked for data regarding their age, level in the Colombian system for selecting beneficiaries for social (security) programmes, prenatal controls, toxoplasmosis tests during pregnancy, positive anti-Toxoplasma IgM test and diagnosis of and treatment for toxoplasmosis.
Blood samples and laboratory tests. Blood samples were taken from the umbilical cord at the moment of birth. The hospitals' laboratory staff centrifuged and stored the samples in tubes for a maximum 8 days at 4°C and then sent them to the reference laboratory. These sera were analysed for antitoxoplasma IgM by fluorometric enzyme immunocapture assay (Toxoplasma gondii IgM, Vircell, Grenada, Spain), according to the manufacturer's indications. An IgA detection test was made of 10% of the samples using an immunosorbent agglutination assay (ISAGA, Biomerieux, Lyon, France); this is an immunocapture reference test which uses formolised toxoplasma antigen. This methodology has been described in in an article by Gomez (15).
Patient follow-up. All the children so identified were followed-up until their infection state was ascertained. A diagnosis of congenital toxoplasmosis was confirmed according to that established by the European Research Network on Congenital Toxoplasmosis. This included IgG specific antibodies persisting after 12 months of age, stable titres in the absence of treatment, compatible signs (cerebral calcification, toxoplasmic retinochoroiditis and/ or hydrocephalus) or positive anti-Toxoplasma IgG and IgM titres in a mother's sera and anti-Toxoplasma IgG in a child's sera (16). Children having reduced IgG titres and in whom anti-Toxoplasma IgG was negative in the absence of treatment were considered not to be infected. Treatment was provided based on current recommendations, i.e. sulfadiazine, pyrimethamine and folinic acid (5).
Epi-Info software (CDC, Atlanta, GA, USA) was used for analysing the data. The results were expressed as means and standard deviation for continuous variables and numbers and percentages (N, %) for categorical variables.
Results
Samples were collected from the participating patients between the 1st April 2009 and 16th July 2010 at Hospital Engativa (level 2) and Hospital La Victoria (at the Instituto Materno Infantil, level 3); 1,448 newborn at Hospital Engativa and 1,776 from the Instituto Materno Infantil were included in the study (total 3,224).
The pregnant women's average age was 22 years old (mode 19; range 10 to 49 years old).
Distribution by age was as follows: 19.4% pregnant adolescents (10-18 years old), 72.1% pregnant adults (19-35 years old) and 8.4% older pregnant females (>35 years old).
Socioeconomic level was identified for 2,880 patients. Distribution by social strata was as follows: 35.8% in social level one, 43.4% in level two, 20.3% in level three, 0.5% in level four and 0.1% in level six.
Regarding obstetric background, data was obtained for 2,982 pregnant women. The average and the mode regarding parity was 1 birth (ranging from 1 to 10); 27.7% of the patients were nulliparous, 69.7% multiparous (1-4 births) and 2.6% were large-scale multiparous (>5 births). 17.5% had undergone 1 abortion and 4.5% had had more than one abortion. 1.7% of the patients had suffered 1 or more stillbirths during their reproductive lives.
Concerning prenatal controls, data was obtained for 3,045 patients; the average and mode were 5 prenatal controls (ranging from 0 to 20); 7.4% of the patients had not attended any, 64.8% had attended 1 to 6 and 27.8% of the patients had attended 7 or more prenatal controls. Regarding the newborn, the Capurro method was used for estimating gestational age in 2,678 of the patients; the average was 39 weeks (the same as the mode, ranging from 20 to 42 weeks): 0.3% were less than 28 weeks, 3.9% 28 to 34 weeks, 6.1% 35 to 36 weeks and 89.7% were more than 37 weeks old.
Data concerning the newborn was collected for 3,087 patients; 49.3% were female and 50.7% male. Average birthweight was 3,005 gr and the mode was 3,030 (ranging from 455 gr to 4,800 gr. Neonates were classified according to weight as follows:
Extremely low birthweight (ELBW) <1,000 g (0.4%); Very low birthweight (VLBW) 1,000-1,500 g (1.0%); Low birthweight (LBW) 1,501-2,500 g (2.2%); Normal birthweight (NBW) 2,500-3,500 g (85.4%); and Excessive birthweight (EBW) > 3,500 g (1.0%).
Clinical data regarding neonates was found in 2,843 questionnaires. Neither hepato-splenomegaly nor microcephaly was found in any newborn in the study; jaundice was identified in 0.4% (11 children) and macrocephaly in one neonate.
Regarding obstetric echography, 96.4% of the 2.841 data collected recorded normal echography, only 3.6% being abnormal. The type of abnormality found was not specified in the questionnaires.
Maternal serum markers
Data was found in 3,058 questionnaires for evaluating anti-Toxoplasma IgG during pregnancy. This test was made for 76.7% of the patients; the result was known for 2,258 patients and positive IgG was reported for 28.2% (26.1-29.8 95%CI) of them.
Anti-Toxoplasma IgG seropositivity prevalence became increased with age, bearing in mind the patients from whom samples were taken and for whom the result was known, as follows: Adolescents (479): 17.0%, Adults (1832): 29.8%, Older pregnant females (232): 36.7%.
Anti-Toxoplasma IgG seropositivity prevalence according to socioeconomic strata was as follows: 26.5% were in social strata 1, 23.3% in social strata 2, 23.6% in social strata 3, 40% in social strata 4 and 0% in social strata 5 and 6.
Data was obtained for 558 patients regarding anti Toxoplasma IgM during pregnancy; positive results were found for 34 patients. Gestational toxoplasmosis incidence in this group of patients was 1.1 per 100 NB based on calculating the total of pregnant women studied (3,224). It is worth noting that 7.5% of the patients having positive IgG did not take the IgM test and 18% did not claim their results.
Data regarding treatment during pregnancy was obtained for 2,803 patients, 29 of whom (1% of the pregnant women in this cohort) received treatment.
Twenty-five (69.4%) of the 34 patients having a positive result received treatment; 22 received spiramycin and the treatment received by the other 3 was unknown.
Newborn serum markers
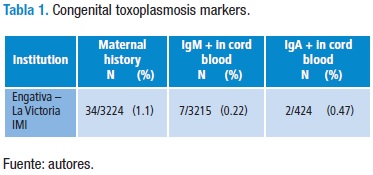
An anti-Toxoplasma IgM result was obtained in cord blood in 3,215 patients; 7 samples were positive. Anti-Toxoplasma IgA was measured in a subgroup of 424 patients, 2 of them proving positive (Table 1).
Analysing the data for patients from Engativá and La Victoria-IMI revealed that no NB were identified as having positive IgM in cord blood amongst the pregnant females having positive IgM detected during pregnancy. The 7 NB having positive IgM in cord blood came from mothers having negative IgG during their pregnancy.
All children having positive IgM results in umbilical cord blood had normal obstetric echographies. No positive IgM results were found in cord blood in the NBs suffering jaundice or in macrocephalic NB in the study.
Of the 3,224 NB recruited, those having a clinical neonatal maternal history or serological results giving rise to a suspicion of congenital toxoplasmosis were followed-up. It was found that 5 children (0.15%) had a positive IgG result regarding their year of age, thereby confirming their diagnosis of congenital toxoplasmosis (i.e. a diagnosis of congenital toxoplasmosis in 1 in 645 LB).
Discussion
This group of patients had antenatal screening for toxoplasmosis, IgG being measured in 77% of the pregnant women. The report was available for 73% of them, giving 28.2% (26%-29% 95%CI) seroprevalence. The prevalence found in this study was lower than the prevalence found in 1998 in Bogotá (43%) and that reported in Bosa (45%) (17). The problem regarding the prevalence obtained from clinical history data is that this does not allow ascertaining whether the techniques' cut-off points were different, whether results were correctly transcribed or whether different techniques were used. An alternative explanation is that the population's socioeconomic conditions have improved during the last few years and this has favoured a reduction in prevalence (18,19).
Analysing seroprevalence by age revealed that IgG seropositivity during pregnancy increased significantly with age. This has been described previously and may be explained by pregnant adolescent females' longer exposure to infection. This group has increased in Colombia during the last few years, placing it at greater risk of congenital toxoplasmosis transmission and thereby aggravating the social and economic load of pregnancy during adolescence.
It was found that the average week for IgG titres being taken was during week 20 and that for IgM during week 26, suggesting that the start of screening during prenatal control and/or controls began late, thereby hampering acute infection being detected during the first half of pregnancy, delaying opportune treatment and possibly leaving greater sequelae in the foetus.
Positive gestational toxoplasmosis IgM incidence in our study was 1.1 per 100 LB. The aforementioned national study found a history of toxoplasmosis during pregnancy in 143 questionnaires from the 15,333 cases studied (0.93 per 100 LB) (15). Previous studies have found that 0.6% to 3% of pregnant women acquired the infection during pregnancy, that such risk was greater in adolescents who had 1.5% probability of seroconversion and that this was lower for pregnant women aged 35 or more years old (0.7% risk of seroconversion) (20). However, it is considered that the rate found in this study could have been under-reported since not all IgG positive patients had an IgM test and those who were negative did not have suitable follow-up, meaning that such data remained unknown and thus seroconversion rates could not be evaluated.
A 61% of the patients were treated with spiramycin. The new Colombian Comprehensive Attention Guidelines (21) for maternal toxoplasmosis recommend level B treatment and evidence has been produced regarding the need for early treatment for improving treatment benefit. This data thus highlights the need for improving early identification and beginning of treatment by overcoming the administrative barriers preventing it. On the other hand, there was a group of pregnant women regarding whom no justification could be found for using spiramycin, thereby indicating the need for ongoing training in gestational toxoplasmosis management for improving its pertinence and effectiveness by using the new comprehensive attention guidelines which clarify the pattern to be followed when managing this infection.
A 0.22% rate was found for anti-Toxoplasma IgM in cord blood, this being better than that calculated in the Colombian multicentre study (1.2%) (15). It is known that testing IgM and IgA in cord blood leads to detecting 70% of NB and that 10 to 12 months postnatal follow-up is required for detecting the rest of the infected children (22). All cases should thus ideally be identified since pregnancy, thereby allowing the best benefits possible and reducing the probability of any child developing signs of infection.
One reason explaining why early serological markers were not detected in the NB is that they received treatment involving prenatal spiramycin which reduced parasitaemia and delayed or modulated NB immunological response (14). Regarding treatment, no evidence was found in our study which led to ascertaining its impact in avoiding infection as few cases were treated (i.e. not enough to demonstrate any statistically significant effect).
It was found that the presence of a negative IgG in pregnant woman was underestimated; it was interpreted as no risk of toxoplasmosis, and the patient is not follow during the pregnancy with new determinations of IgM or IgG. or, even less so, warned about taking preventative measures or educated regarding preventative strategies.
This study's results are relevant when it is taken into account that the sample size was several times greater than that in similar work and represents a tangible effort at understanding the real situation regarding toxoplasmosis in Bogotá. However, one of the study's weaknesses lay in the loss concerning patient follow-up during all phases of the study. Patients were found who had attended very few or no prenatal controls; only two thirds of the patients who had attended prenatal controls had taken an antitoxoplasma IgG test during pregnancy. Some patients never knew the result of their tests and it was not known why some did not claim them or why there had been a delay in making them available.
The type of irregular screening which these patients received was not very useful and had very poor performance in the study conditions, involving as it did deficient prenatal control, late interpretation and contradictory maternal serum markers, late start to and irregular treatment as well as problems regarding health insurance. However, two out of five children in this cohort were detected in this way and no sequelae were found.
Conclusions
IgG seropositivity during pregnancy was seen to increase significantly with age, being 17% in adolescents, 29% in adult females and 37% in women over 35 years of age.
Gestational toxoplasmosis incidence due to positive IgM titre was 1.1% per 100. Congenital toxoplasmosis incidence in both hospitals during this study was 0.15%.
The detection strategy regarding gestational and congenital toxoplasmosis must be improved.
Conflict of Interest: None declared by the authors.
Financing: This work was financed by Colciencias (project # 111304-18247). Colciencias had no part in designing, developing or the publication of this study.
Acknowledgements: None declared by the authors.
Referencias
1. Montoya J, Liesenfeld O. Toxoplasmosis. Lancet. 2004;363: 1965-1976. [ Links ]
2. Gómez J. (2002). Toxoplasmosis: Un problema de salud pública en Colombia. Rev. Salud Pública. 2002;4:7-10. [ Links ]
3. Gómez J, Montoya M, Castaño J. Epidemiología de la infección por Toxoplasma gondii en gestantes de Armenia - Quindío Colombia. Colomb Med 1993;24:14-18. [ Links ]
4. Juliao CA, Moreno GS. Estudio Nacional de Salud: Toxoplasmosis en Colombia. Ministerio de Salud Bogotá: Imprenta Instituto Nacional de Salud. 1988. [ Links ]
5. Gomez Marín JE. Evaluación del tratamiento de la gestational toxoplasmosis en una cohorte colombiana. Infectio. 2005;9:16-23. [ Links ]
6. Dutton GN, Gilbert R. Epidemiology of infection in pregnant women. En E. P. Thomas Ambroise, Congenital toxoplasmosis. Scientific Background, Clinical Management and Control. Paris: Springer-Verlag. 2002:237-49. [ Links ]
7. Jones J, Kruzon-Moran D, Wilson M, McQuillan G, Navin T, & McAuley J. Toxoplasma gondii Infection in the United Sates: seroprevalence and risk factors. Am J Epidemiol. 2001; 154:357-65. [ Links ]
8. Bahía-Oliveira LM, Jones JL, Azevedo-Silva J, Alves CC, Oréflce F, Addiss DG. Highly endemic, waterborne toxoplasmosis in north Rio de Janeiro state, Brazil. Emerg Infect Dis. 2003;9:55-62. [ Links ]
9. Rosso F, Agudelo A, Isaza A, Montoya JG. Toxoplasmosis congénita: aspectos clínicos and epidemiológicos de la infección durante el embarazo. Colomb. Med. 2007;38:316-37. [ Links ]
10. Pinon JM, Dumon H, Chemla C, Franck J, Petersen E, Lebech M, et al. Strategy for diagnosis of congenital toxoplasmosis: evaluation of methods comparing mothers and newborns and standard methods for postnatal detection of immunoglobulin G, M, and A antibodies. J Clin Microbiol. 2001;39:2267-71. [ Links ]
11. Tissot Dupont D, Fricker-Hidalgo H, Brenier-Pinchart MP, Bost-Bru C, Ambroise-Thomas P, Pelloux H. Usefulness of Western blot in serological follow-up of newborns suspected of congenital toxoplasmosis. Eur J Clin Microbiol Infect Dis. 2003; 22:122-5. [ Links ]
12. Gilbert RE, Thalib L, Tan HK, Paul M, Wallon M, Petersen E. European Multicentre Study on congenital toxoplasmosis (2007). Screening for congenital toxoplasmosis: accuracy of immunoglobulin M and immunoglobulin A tests after birth. J Med Screen. 2007;14:8-13. [ Links ]
13. Barrera AM, Castiblanco P, Gómez Marín JE, López MC, Ruiz A, Moncada L, Reyes P, et al. Frecuencia de toxoplasmosis adquirida durante el embarazo en el Instituto Materno Infantil de Bogotá. Revista de Salud Pública. 2002;4:286-93. [ Links ]
14. Gómez-Marin JE, de-la-Torre A, Angel-Müller E, Rubio J, Arenas J, Osorio E, et al. First Colombian multicentric newborn screening for congenital toxoplasmosis. PLoS Negl Trop Dis. 2011;5:1195. [ Links ]
15. Lebech M, Johnson DHM, Seitz HM, Thulliez P, Gilbert RE, et al. Classification system and case definitions of Toxoplasma gondii infection in immunocompetent pregnant women and their congenitally infected offspring. Eur J Clin Microbiol Infect Dis. 1996;15:799-805. [ Links ]
16. Guacaneme MC, Suárez E, Meneses NE, Prieto CH. Comportamiento epidemiológico de la toxoplasmosis en las gestantes usuarias del Hospital Pablo VI Bosa I Nivel Empresa Social del Estado 1999. Seinvestiga. 2001;6:40. [ Links ]
17. Gómez-Marin JE, Montoya-de-Londono MT, Castano-Osorio JC. A maternal screening program for congenital toxoplasmosis in Quindio, Colombia and application of mathematical models to estimate incidences using age-stratified data. Am J Trop Med Hyg. 1997;57:180-6. [ Links ]
18. Juliao O CA, Moreno GS. Estudio Nacional de Salud: Toxoplasmosis en Colombia. Ministerio de Salud Bogotá: Imprenta Instituto Nacional de Salud. 1988. [ Links ]
19. Gómez-Marin J. Toxoplasma. Capítulo 27. En: Diaz FJ, Estrada S, Franco L, Jaramillo JM, Maestre A, Ospina S, Robledo C, Robledo J. Microbiología de las Infecciones Humanas. 2007:384-99. Medellín: Corporación para las Investigaciones Biológicas. [ Links ]
20. Cortés JA, Gómez Marin J, Silva P, Arévalo L, Arevalo I, Alvarez MI, Beltrán S, Corrales I, Angel Muller E, Ruiz J, Gómez PI, en representación del Grupo Desarrollador de la Guía de atención Integral de embarazo, parto and puerperio. Guía de atención integral para la prevención, detección temprana y tratamiento de las complicaciones del embarazo, parto and puerperio: sección toxoplasmosis en el embarazo. Infectio. 2012; 16:230-46. [ Links ]
21. Torres E, Rivera R, Cardona N, Sanchez V, Lora F, Gómez-Marin JE. Evaluation of IgG anti-toxoplasma avidity and PCR in the postnatal diagnosis of congenital toxoplasmosis. Pediatr Infect Dis J. 2013; in press. [ Links ]