Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista de la Facultad de Medicina
Print version ISSN 0120-0011
rev.fac.med. vol.62 no.4 Bogotá Oct./Dec. 2014
https://doi.org/10.15446/revfacmed.v62n4.44397
DOI: http://dx.doi.org/10.15446/revfacmed.v62n4.44397
ORIGINAL RESEARCH
Maternal near miss morbidity in Colombia: variables related to opportune access to health care related to the number of inclusion criteria
Morbilidad materna extrema en Colombia: variables relacionadas con el acceso oportuno a la atención en salud según el número de criterios de inclusión
José Luis Pérez-Olivo1, Esther Liliana Cuevas1, Sara García-Forero1, Adalberto Campo-Arias2
1 Instituto Nacional de Salud. Bogotá, Colombia.
2 Instituto de Investigación del Comportamiento Humano. Bogotá, Colombia.
Correspondence: José Luis Pérez-Olivo. Avenida Calle 26 No. 51-20, Instituto Nacional de Salud, Grupo Maternidad Segura. Bogotá, Colombia. Telephone: +57 1 2207700. E-mail: jl.perez82@uniandes.edu.co.
Received: 15/07/2014 Accepted: 08/08/2014
Summary
Background. In Colombia, maternal near miss morbidity is monitored in the health surveillance system. The National Health Institute included a special report on cases that met three or more World Health Organization criteria according to the World Health Organization criteria.
Objective. To estimate the relationship between variables related to opportune access to health care services in Colombia during 2013 depending on inclusion criteria –three or more– for maternal near miss morbidity.
Materials and methods. A cross-sectional analysis of the national registry of obligatory notification on maternal near miss morbidity was performed. Cases with three or more criteria were compared with those with one or two according to some variables related to the timely access of health care services.
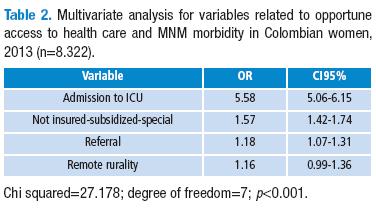
Results. A total of 8 434 maternal near miss morbidity cases were reported, women were aged between 12 and 51 years old (M=26.4, SD=7.5). 961 (11.4%) lived in remote rural areas; 4 537 (53.8%) were uninsured under the health system, or they were affiliated to either the subsidized or special health care regime; 845 (10.0%) belonged to an ethnic minority; 3 696 (44.4%) were referred to a more complex service; 4 097 (49.2%) were admitted to the intensive care unit; and 3 975 (47.1%) met three or more of the inclusion criteria for maternal near miss morbidity. They were combined to meet three or more of the case inclusion criteria: intensive care unit admission (OR=5.58; IC95% 5.06-6.15); being uninsured or affiliated to the subsidized or special regime (OR=1.57; IC95% 1.42-1.74); and referral to a more complex service (OR=1.18; IC95% 1.07-1.31).
Conclusions. In Colombia, the timely access of health care services is related to maternal near miss morbidity with three or more inclusion criteria.
Keywords: Morbidity; Pregnancy; Pregnancy Complications; Health Services Accessibility; Quality of Health Care; Cross-Sectional Studies (MeSH).
Pérez-Olivo JL, Cuevas EL, García-Forero S, Campo-Arias A. Maternal near miss morbidity in Colombia: variables related to access of health care related to the number of inclusion criteria. Rev Fac Med. 2014;62(4):553-8. http://dx.doi.org/10.15446/revfacmed.v62n4.44397.
Resumen
Antecedentes. En Colombia, la morbilidad materna extrema es monitoreada en el sistema de vigilancia epidemiológica. El Instituto Nacional de Salud incluyó el análisis particular de los casos que reunieran tres o más criterios de inclusión de definición de caso.
Objetivo. Estimar la relación entre variables relacionadas con el acceso oportuno a la prestación de los servicios en salud y los criterios de inclusión –tres o más– para morbilidad materna extrema en Colombia durante 2013.
Materiales y métodos. Se realizó un análisis transversal del registro nacional de notificación obligatoria sobre morbilidad materna extrema; los casos con tres criterios o más se compararon con aquellos con uno o dos según algunas variables relacionadas con el acceso oportuno a la prestación de servicios en salud.
Resultados. Se notificaron 8.434 casos de morbilidad materna extrema, edades entre 12 y 51 años (M=26.4; DE=7.5). 961 (11.4%) residentes en zona rural remota, 4.537 (53.8%) en régimen no asegurado, subsidiado o especial, 845 (10.0%) pertenecientes a minoría étnica, 3.696 (44.4%) fueron remitidas a un servicio de mayor complejidad, 4.097 (49.2%) recibieron servicios en unidad de cuidados intensivos y 3.975 (47.1%) reunieron tres o más criterios de inclusión de caso morbilidad materna extrema. Se asociaron a reunir tres o más criterios de inclusión de caso: el ingreso a unidad de cuidados intensivos (OR=5.58; IC95% 5.06-6.15), régimen no asegurado, subsidiado o especial (OR=1.57; IC95% 1.42-1.74) y remisión a servicio de mayor complejidad (OR=1.18; IC95% 1.07-1.31).
Conclusiones. En Colombia, el acceso oportuno a los servicios de atención en salud se relaciona con morbilidad materna extrema de tres o más criterios de inclusión.
Palabras clave: Morbilidad; Embarazo; Complicaciones del Embarazo; Accesibilidad a los Servicios de Salud; Calidad de la Atención de Salud; Estudios Transversales (DeCS).
Pérez-Olivo JL, Cuevas EL, García-Forero S, Campo-Arias A. Morbilidad materna extrema en Colombia: variables relacionadas con el acceso a la atención en salud según el número de criterios de inclusión. Rev Fac Med. 2014;62(4):553-8. http://dx.doi.org/10.15446/revfacmed.v62n4.44397.
Introduction
The World Health Organization (WHO) understands maternal near miss (MNM) morbidity as “a woman who nearly died but survived a complication that occurred during pregnancy, childbirth or within 42 days of termination of pregnancy” (1). This is a recently reviewed and integrated concept to simplify and unify the diversity of terminology and definitions, and to facilitate codification and notification in national records (1-3).
Given the existing polysemy surrounding the concept of MNM, systematic reviews in the last decade showed divergent prevalences for MNM morbidity. For example, Wilson and Salihu observed a prevalence of 1% in the United States and of between 3% and 9% in developing countries (4). Van Roosmalen and Zwart, in countries of high financial incomes —including Canada, Finland, Holland, and the United Kingdom—, found prevalences of between 3.8 and 12 per 1000 live births (5). Tunçalp and cols. found prevalences of between 0.6% and 15% based on the criteria of specific diseases related to the event; between 0.04 and 4.5% based on management strategies; as well as 0.1% and 0.9% based on organ failure criteria (Mantel’s criteria). In all of these cases, the highest frequencies were found in developing countries of Africa, Latin America, and Asia (6).
In some circumstances, the MNM morbidity prevalence, incidence or rate is taken as an indicator of the quality of maternal health care in a region or country. This milestone is more sensitive than the maternal mortality rate, given the greater frequency of these events (1,7). In Colombia, the epidemiological surveillance system (Sivigila) of the National Health Institute recently included MNM in the maternal health indicators of Colombian women together with several criteria for defining it (8).
The present study evaluates the possible associations between some variables related to the opportune access to health services and MNM inclusion criteria. These variables include insurance —access to the health system—, admission to the Intensive Care Unit (ICU) —the capacity for resolving health problems—, belonging to an ethnic minority —cultural barrier—, living in a remote rural area —geographic barrier—, the reference system —level of care—, and the severity of the cases —found from the number of inclusion criteria that the MNM case meets—. The findings of this research will allow for a better knowledge of MNM morbidity in the national context with regard to the severity of the cases.
The goal of the present study was to estimate the relationship between the variables related to opportune access to health care services with relation to the inclusion criteria — three or more— for MNM morbidity in Colombia in 2013.
Materials and methods
A cross-sectional study was designed with a secondary analysis of all of the obligatory notification cases of Sivigila. The study was carried out following the ethical principles of health research, of information available in registries, and of the management of confidentiality and anonymity of data, according to Colombian norms (9).
For this analysis, the following variables were taken: insurance —as an indicator of access to the health system—, admission to the ICU —as an estimate of the health problem solving capacity of the care system—, living in a remote rural area —as a measure of the geographic accessibility of the resources—, the use of the reference system —the level of attention needed for care—, and the number of inclusion criteria for the definition of the case of MNM —as a proxy of the level of severity of the cases—.
For the categorization of MNM, meeting one of the criteria presented in the annex of this document is necessary. Given that the National Health Institute takes cases with three or more inclusion criteria as a cut-off point for doing additional analysis of notified cases —since they are considered to be at a level of greater severity—, this cut-off point was taken for the present study. In addition, it is necessary to keep in mind that the notification of these cases is relatively recent, and the possibility of under-recording is high.
A descriptive analysis of the variables was carried out and frequencies and percentages were established. The relationships between factors related to opportune access were evaluated repeatedly. The factors were taken as independent variables, and having three or more inclusion criteria as the definition of a MNM case was taken as the dependent variable through the calculation of odds ratios (OR), with confidence intervals of 95% (CI 95%). Finally, an adjustment of the associations was made through logistic regression. For this, Greenland’s (10) recommendations were followed. The goodness of fit was estimated with the Hosmer-Lemeshow test (11). The statistical analysis was carried out in the program SPSS 16.0.
Results
During 2013, there was notification of 8 434 women with cases of MNM. All of the cases were included in the analysis. The ages of the women observed ranged from 12 to 51 years (M=26.4; SD=7.5). 845 (10.0%) women were identified as belonging to an ethnic minority, 961 (11.4%) were residents of a remote rural area, 4 537 (53.8%) had an affiliation to the system that was not insured, or it was subsidized or special —this category was established after a series of several comparisons that showed that all three variables had similar relationship to the dependent variable and, after a statistical test, it was seen that there were not statistical differences between them that were significant enough to merit considering them separately—, 3 696 (44%) required referral to a more complex level of attention —this, with a basis in 8 322 cases due to information omissions—, 4 097 cases (49.2%, n=8 322) indicated admission to the ICU, and 3 975 (47.1%) presented three or more MNM inclusion criteria.
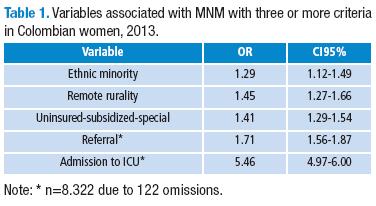
In the bivariate analysis, it was observed that all of the variables of opportunity of access to health care showed a statistically significant association to having three or more MNM case inclusion criteria (Table 1).
Repeatedly, in the multivariate analysis, identification as part of an ethnic minority was not included, given that, in the adjustment, it lost statistical significance and did not produce a change of more than 10% in the most robust association, following Greenland. Also, remote rurality did not maintain statistical significance. Nonetheless, it was left in the final model. The goodness of fit was not adequate, and so it should be interpreted with due caution since the probability indicates that the model does not follow the habitual distribution of the test (Table 2).
Discussion
In the present study, it is observed that the notified cases of MNM with three or more inclusion criteria maintain a relationship with the type of affiliation that the women have to the Colombian health system — be it an affiliation without insurance, a subsidized affiliation, or a special one— and that they require services with a greater capacity to solve medical services –referral and admission to the ICU—.
In the present study it was observed that the notified cases of MNM with three or more inclusion criteria maintain a relationship with some of the characteristics of the population related to opportune access to health care (and of the population of gestating women especially). In general, the findings are consistent with what can be expected in terms of the type of affiliation, given that, with the exception of special regimes, uninsured women and those affiliated to the subsidized regime are part of a population segment where the effects of inequalities and social inequities converge (12,13).
In the present study, a statistically significant association between MNM morbidity and the need for referral and for care in the ICU was found. It is hoped that the most severe cases of MNM merit care at levels of higher complexity, referrals, and even treatment in the ICU for their positive resolution (7).
Elsewhere, it was observed that belonging to an ethnic minority —a measure of the presence of a cultural barrier to access— and remote rurality —an estimator of a geographic barrier to access— had no relationship with the severity of the MNM cases (14,15). This may suggest the existence of bias in the information on current data of the Colombian system.
Conclusions
This study is a contribution to the available information on maternal health in Colombia. Usually official health information systems focus on descriptive aspects of the data (16). However, the findings should be interpreted carefully due to the usual questioning of the quality of information from official health institutions (17,18). Also, one should keep in mind the limitations of cross-sectional analyses that prevent the establishment of a clear line of causality (19).
It is concluded that timely access to health care services is related to MNM with three or more inclusion criteria in Colombia. Women who are uninsured or subsidized, or in the special health care regime, present MNM more frequently, and the most severe cases require services of a higher level of complexity. Periodic evaluation of the characteristics of women with MNM and of the timely access to health care services that are provided to this group is required.
Conflict of interest
None declared by the authors.
Financing
The Human Behavioral Research Institute (Bogotá, Colombia) financed the participation of Dr. Adalberto Campo-Arias.
Acknowledgements
To the National Health Institute and the Human Behavioral Research Institute for their collaboration and financing of this research.
References
1. Say L, Souza JP, Pattinson RC. WHO working group on Maternal Mortality and Morbidity classifications. Maternal near miss-towards a standard tool for monitoring quality of maternal health care. Best Pract Res Clin Obstet Gynaecol. 2009;23:287-96. http://doi.org/dhd5dh. [ Links ]
2. Souza JP, Cecatti JG, Haddad SM, Parpinelli MA, Costa ML, Katz L, et al. The WHO maternal near-miss approach and the maternal severity index model (MSI): tools for assessing the management of severe maternal morbidity. PloS One. 2012;7:e44129. http://doi.org/zc4. [ Links ]
3. Galvão LP, Alvim-Pereir F, de Mendonça CM, Menezes FE, Góis KA, Ribeiro Jr RF, et al. The prevalence of severe maternal morbidity and near miss and associated factors in Sergipe, Northeast Brazil. BMC Pregnancy Childbirth. 2014;14:25. http://doi.org/zc5. [ Links ]
4. Wilson RE, Salihu HM. The paradox of obstetric "near misses": converting maternal mortality into morbidity. Int J Fertil Womens med. 2006;52:121-7. [ Links ]
5. Van Roosmalen J, Zwart J. Severe acute maternal morbidity in high-income countries. Best Pract Res Clin Obstetr Gynaecol. 2009;23:297-304. http://doi.org/bkjsh7. [ Links ]
6. Tunçalp Ö, Hindin MJ, Souza JP, Chou D, Say L. The prevalence of maternal near miss: a systematic review. BJOG. 2012;119:653-61. http://doi.org/zc6. [ Links ]
7. World Health Organization. Evaluating the quality of care for severe pregnancy complications. The WHO near-miss approach for maternal health. Geneva: World Health Organization; 2011. [ Links ]
8. Presidencia de la República de Colombia. Decreto 3518 por el cual se crea y reglamenta el Sistema de Vigilancia en Salud Pública y se dictan otras disposiciones. Bogotá: Presidencia de la República de Colombia; 2006. [ Links ]
9. Ministerio de Salud. Resolución 008430 por la cual se establecen las normas científicas, técnicas y administrativas para la investigación en salud. Bogotá: Ministerio de Salud; 1993. [ Links ]
10. Greenland S. Modeling and variable selection in epidemiologic analysis. Am J Public Health. 1989;79:340-9. http://doi.org/frsvfn. [ Links ]
11. Hosmer DW, Taber S, Lemeshow S. The importance of assessing the fit of logistic regression models: a case study. Am J Public Health. 1991;81:1630-5. http://doi.org/br4h96. [ Links ]
12. Borrell C. Desigualdades y servicios de salud. Saúde e sociedade. 2006; 15:9-22. http://doi.org/dmfvzs. [ Links ]
13. Cardona D, Acosta LD, Bertone CL. Inequidades en salud entre países de Latinoamérica y el Caribe (2005-2010). Gac Sanit. 2013;27:292-7. http://doi.org/f2f6t3. [ Links ]
14. Presidencia de la República de Colombia. Decreto 2174 por el cual se organiza el Sistema Obligatorio de Garantía de Calidad del Sistema General de Seguridad Social en Salud. Bogotá: Presidencia de la República de Colombia; 1996. [ Links ]
15. Congreso de Colombia. Ley 1434 por medio de la cual se reforma el Sistema General de Seguridad Social en Salud y se dictan otras disposiciones. Bogotá: Congreso de Colombia; 2011. [ Links ]
16. Palacio-Mejía LS, Hernández-Ávila JE, Villalobos A, Cortés-Ortiz MA, Agudelo-Botero M, Plaza B. Sistemas de información en salud en la región mesoamericana. Salud Publica Mex. 2011;53:s368-74. http://doi.org/fzt4x6. [ Links ]
17. Alazraqui M, Mota E, Spinelli H. Sistemas de Información en Salud: de sistemas cerrados a la ciudadanía social. Un desafío en la reducción de desigualdades en la gestión local. Cad Saude Pública. 2006;22:2693-702. http://doi.org/c7zv23. [ Links ]
18. Lozano R, Soliz P, Gakidou E, Abbott-Klafter J, Feehan D, Vidal C, et al. Evaluación comparativa del desempeño de los sistemas estatales de salud usando cobertura efectiva. Salud Publica Mex. 2007;49:S53-69. http://doi.org/cmpw2j. [ Links ]
19. Hernández-Avila M, Garrido-Latorre F, López-Moreno S. Diseño de estudios epidemiológicos. Salud Publica Mex. 2000;42:144-54. http://doi.org/cf3qfm. [ Links ]