Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista de la Facultad de Medicina
Print version ISSN 0120-0011
rev.fac.med. vol.62 no.4 Bogotá Oct./Dec. 2014
https://doi.org/10.15446/revfacmed.v62n4.43147
DOI: http://dx.doi.org/10.15446/revfacmed.v62n4.43147
CASE REPORTS
Association between periodontal disease and septicemia due to pyogenic hepatic abscess
Asociación de enfermedad periodontal y sepsis por absceso hepático piógeno
Análida Elizabeth Pinilla1, Myriam Consuelo López1, Martha Isabel Murcia2
1 Grupo de Apoyo Pedagógico y Formación Docente. Departamento de Medicina Interna. Facultad de Medicina. Universidad Nacional de Colombia. Bogotá, Colombia.
2 Departamento de Microbiología. Universidad Nacional de Colombia. Bogotá, Colombia.
Correspondence: Análida Elizabeth Pinilla. Departamento de Medicina Interna. Oficina 510. Facultad de Medicina. Edificio 471. Universidad Nacional de Colombia. Carrera 30 No. 45-03. Bogotá, Colombia. Telephone: +57 316500. Extension: 15011/15012/15167. E-mail: aepinillar@unal.edu.co.
Received: 25/04/2014 Accepted: 14/07/2014
Summary
Case of a 65 year-old man with type-2 diabetes mellitus for 15 years who complained of abdominal pain in the right upper quadrant associated with unquantified fever and weight loss over a period of 25 days. In the emergency room, he presented tachycardia, tachypnea and fever of 37 º C, diffuse abdominal pain from light palpation without peritoneal irritation or right upper quadrant tenderness upon fist percussion test. Within a few hours the patient evolved to septic shock and required transfer to the intermediate care unit. The abdominal computerized axial tomography showed multiloculated hepatic abscess. Percutaneous drainage was performed with the culture positive for Escherichia coli and Fusobacterium spp. Then, the differential diagnosis was made between pyogenic or amebic liver abscess. Subsequently, oral cavity examination revealed severe periodontal disease with coronal destruction; therefore, extraction was scheduled.
Keywords: Liver Abscess; Diabetes Mellitus; Mouth; Escherichia coli; Fusobacterium, Bacteremia (MeSH).
Pinilla AE, López MC, Murcia MI. Association between periodontal disease and septicemia due to pyogenic hepatic abscess. Rev Fac Med. 2014;62(4):631-5. http://dx.doi.org/10.15446/revfacmed.v62n4.43147.
Resumen
Las infecciones bacterianas de la cavidad oral, en particular gingival y periodontal, son causa de bacteriemias que, dependiendo de la historia clínica del paciente, pueden favorecer el desarrollo de infecciones a distancia como: endocarditis, abscesos piógenos en diferentes órganos como cerebro, hígado, riñón, entre otros. Por esto, se ilustra un caso de enfermedad periodontal asociado con absceso hepático piógeno. Se presenta un paciente masculino de 65 años con antecedente de diabetes mellitus tipo 2, quien consultó por dolor abdominal en hipocondrio derecho de 25 días de evolución, asociado a fiebre y pérdida de peso no cuantificados. Al examen físico, en urgencias, presentó taquicardia, taquipnea, fiebre de 39ºC; como hallazgo relevante se encontró dolor abdominal difuso a la palpación superficial, sin irritación peritoneal. No se reportó sensibilidad a la puñopercusión ni a la digitopresión intercostal en hipocondrio derecho. En pocas horas evolucionó a choque séptico, por lo que requirió traslado a unidad de cuidado intermedio. La tomografía axial computarizada abdominal evidenció absceso hepático multiloculado; se realizó drenaje percutáneo con cultivo positivo para Escherichia coli y Fusobacterium spp.; por tanto, se hizo el diagnóstico diferencial entre absceso hepático de origen piógeno o amebiano. Posteriormente, se realizó examen de cavidad oral que reveló enfermedad periodontal severa con destrucción coronal y se programó exodoncia.
Palabras clave: Absceso Hepático; Diabetes Mellitus; Boca; Escherichia coli; Fusobacterium; Bacteriemia (DeCS).
Pinilla AE, López MC, Murcia MI. Asociación de enfermedad periodontal y sepsis por absceso hepático piógeno. Rev Fac Med. 2014;62(4):631-5. http://dx.doi.org/10.15446/revfacmed.v62n4.43147.
Introduction
Bacterial infections of the oral cavity —and particularly gingival and periodontal infections— are responsible for bacteremias that, depending on the clinical history of the patient, can favor the development of remote infections like endocarditis, and pyogenic abscesses in different organs (e.g. brain, liver, kidney, etc.).
These situations may be more frequent and profuse if the patient has an immunosuppression disorder caused by diabetes mellitus, HIV, or malnutrition, or corticosteroids or cytostatics indicated in the case of tumors or organ transplants (1-3) Furthermore, it is important to create an appropriate clinical history. This starts with listening to the patient, with an empathetic approach, so as to find the motive of the consultation, the current disease, and the patient’s background. This information will aid in taking the appropriate direction in each clinical case, and should be followed by a complete physical examination that includes the oral cavity (4). Here we present the clinical case of a patient with diabetes mellitus and hepatic abscess that required a differential diagnoses to ascertain its etiology.
Hepatic abscess (HA) is a disease that may threaten the life of the affected patient despite advances in diagnosis and treatment. In the case of pyogenic hepatic abscess (PHA), the most common causes lies in the bile duct and the colon. There may also be a background of gastric or duodenal surgery, local trauma, and pancreatitis. Nevertheless, remote hematogenous spreading should also be contemplated, as in this case. The germs isolated with the greatest frequency in the hemocultures and from the purulent material obtained from the drainage of the PHA were: Klebsiella pneumoniae, Escherichia coli and Enterococcus spp (5,6).
Anaerobic negative Gram bacteria are part of the normal flora of the mouth, upper respiratory tract, and the intestinal and the genitourinary tracts. They include Bacteroides, Prevotella intermedia, Porphyromonas gingivalis and Fusobacterium, among others. They may be associated with endogenous infections. The isolation of these germs requires special conditions and measures. The positivity of cultures in clinical samples is important and should be correlated with the clinical history (3,7,8).
In addition, it is important to take between 2 and 3 hemocultures with asepsis and antisepsis, from different sites, since, if they are positive, the presence of contamination can be ruled out (9,10). The use of automated commercial systems is recommended, including special bottles for the isolation of anaerobes, resins that capture antibiotics, incubation in equipment that provides constant agitation of the samples, and modern microbe detection systems (11).
Also, cultures of the PHA drainage and of the oral cavity where scaling occurred can be analyzed, and anaerobic and aerobic germs should be searched for. In the present clinical case, Fusobacterium spp. was isolated. It is an immobile anaerobic Gram-negative bacterium that is part of the normal flora of the oral cavity, present in dental plaque and the gingival sulcus, as well as the lung, and the gastrointestinal and genitourinary tracts (8,12,13).
Clinical case
65-year-old man with a relevant background of type-2 diabetes mellitus diagnosed 15 years before. He attended the consultation because of a presentation of 25 days of evolution consisting of abdominal pain in the right hypochondrium and epigastrium associated with adynamia, hyporexia, and weight loss. Furthermore, there was a presentation of unquantified fever and vomiting over a period of 3 days.
The patient accessed health care through the emergency room on 3 occasions and received acetaminophen. On the second occasion, the diagnostic impression was urinary tract infection, and the patient was treated with trimethoprim sulfamethoxazole without any improvement. He returned to the emergency service with a clinical presentation of a general state of deterioration and disorder of the mental sphere with confusion and faintness. Physical exam: tachycardia 120 per min, tachypnea 24 per min, fever 39ºC, and first-degree dehydration. Cardiopulmonary exam: no important findings. Abdomen: diffuse pain upon superficial palpation, without peritoneal irritation, no evidence of visceromegaly, no sensitivity reported to first percussion or to intercostal finger pressure in the right hypochondrium.
In a few hours, the presentation evolved to septic shock, metabolic acidosis, and prerenal kidney failure, for which he was moved to the intermediate care unit and required inotropic support. Due to the focalization of the pain in the abdomen, an abdominal computerized axial tomography (CAT) was performed, showing a multiloculate hepatic abscess (Figure 1). Immediately, ceftriaxone 2 g/d was administered, along with metronidazole 1500 mg/d, without previously taking hemocultures. The initial hemogram revealed severe leukocytosis (34 800) and neutrophilia (87%), with progressive response until normalization of leukocytes and neutrophils after percutaneous drainage and antibiotic therapy.
To complete the PHA treatment, percutaneous drainage guided by ultrasonography was performed. The drainage culture showed presence of the Gram-negative bacteria Escherichia coli and Fusobacterium spp. For the differential diagnosis between a pyogenic or amebic origin of the hepatic abscess, a test for antibodies against Entamoeba histolytica with negative results from the IgG ELISA with a reference value of 0.180, absorbency of 0.34, and negative immunodiffusion (14).
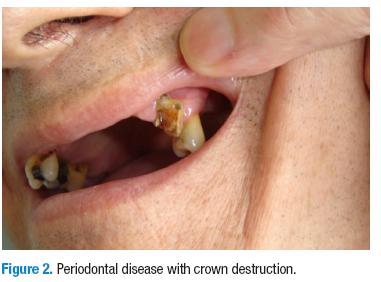
5 days after, an examination of the oral cavity was carried out in which severe periodontal disease with crown destruction that had improved with the initiation of antibiotic treatment. Tooth extraction was scheduled (Figure 2). Given the evidence in the literature of the presence of Fusobacterium spp. in odontogenic infections, and the fact that there was no evidence of another source of infection that would explain this remote infection, an inference was made, though clinical judgment, about the possible origin of the bacteremia that caused the pyogenic hepatic abscess through hematogenous dissemination.
Discussion
HA is an etiological entity with a varied clinical presentation. As such, it requires a complete clinical record for the physician to suspect it. HA is defined as one or more lesions in the liver associated with a positive bacterial culture in the material obtained through percutaneous aspiration or surgery (3,15). It may be secondary to intra-abdominal infection (infection of bile duct, intestinal tract) or extra-abdominal infection through significant bacteremia from the oral cavity, endocardium, etc. In this case, the entrance to the liver is through the bile duct, the portal system, and the hepatic artery.
It is also always important to clarify the differential diagnosis in all patients with HA in order to specify the etiology and, in this way, provide a specific treatment. In tropical countries, the first cause to be ruled out is infection with E. Histolytica. Nevertheless, there are other infectious agents including bacteria, fungi, and parasites (5,6,16,17).
The clinical presentation of the patient with PHA can be of diverse etiologies, with little significant differentiation in symptoms: fever, asthenia, weight loss, anorexia, general discomfort, vomiting, nausea, coughing, abdominal pain. Also, in the physical examination, alteration of the vital signs is discovered with systemic inflammatory response, heptomegaly, and abdominal pain located in the right hypochondrium and right flank of the epigastrium (18).
Up until the 1970s, the diagnosis of AH was suspected from clinical data and unspecific laboratory exams. It was confirmed by diagnostic hepatic puncture or surgery. These procedures permitted obtaining the contents of the abscess and, in rare cases, confirming the amebic etiology of the abscess through the observation of the trophozoite of E. histolytica. With the advent of hepatic ultrasonography, the presence of PHA, suspected due to the clinical history, is confirmed in the vast majority of patients. For this reason, it is the first choice in terms of imaging procedures.
Later, tests like immunodiffusion and the ELISA test became gold standards for the diagnosis of AHA, displacing the classic (and sometimes uncertain) investigation method of finding trophozoites in the abscess drainage. This exam allows us to carry out a differential diagnosis between amebic and bacterial etiologies, as was the case for the reported patient (14,19,20). Furthermore, other diagnostic images, like the CAT and the magnetic resonance scans, are currently available, not to mention interventional radiology. These diagnostic images describe the PHA, but they do not allow for the differentiation of the etiology. Thorax radiography may show elevation of the hemidiaphragm and varying degrees of pleural effusion (15). All of the above has allowed us to reduce morbimortality related to HA.
In PHA, as in this clinical case, diverse bacteria are isolated from the material obtained from the drainage. In this patient, Escherichia coli and Fusobacterium spp. were isolated, like in other studies (5,6). Fusobacterium nucleatum has been associated with periodontal disease, and it is well known that hematogenous dissemination of the bacteria from the oral cavity can occur. For this reason, individuals must maintain an adequate oral hygiene and go to their dentist periodically for mechanical dental cleaning in order to avoid oral infections and the risk of systemic dissemination (21,22). As a result, the isolation in this case of Fusobacterium spp suggested bacteremia, something that could not be corroborated from hemocultures because the patient was presenting severe periodontal disease that was diagnosed late and retrospectively (Figure 1).
This case emphasized the association between PHA and periodontal disease in a patient with type-2 diabetes mellitus. However, this association could present in diverse comorbidities and not only with type-2 diabetes mellitus. Infections of the oral cavity have varying etiologies —bacterial, mycotic, viral, or mixed— and can spread by different mechanisms —hematogenous, nervous, lymphatic, adjacency—. As a result, they can cause brain abscesses, meningitis, cavernous sinus thrombosis, odontogenic sinusitis, peri-orbital infections, bacterial endocarditis, mediastinitis, pneumonia, and even septicemia, among other pathologies (23).
In this clinical case, the mechanism of infection of the PHA was secondary to dental disease and is different to infection from the bile duct or the colon. Bacteremia from the oral cavity passed through the circulatory system through the inferior vena cava and then arrived to the liver through the hepatic artery. In contrast, bacteremia from the colon arrives to the liver through the portal system (13).
Conclusions
The clinical history is indispensible. We must insist that a physician should examine the oral cavity to rule out a dental septic source as the origin of the bacteremia.
HA is a differential diagnosis for abdominal pain in all patients, particularly in patients with immunosuppression disorders as in this clinical case where the patient had type-2 diabetes mellitus. Medical imaging is an essential diagnostic tool when AH is clinically suspected, even though it does not allow the specification of the etiology. Nevertheless, ultrasonography remains the first choice due to its availability and low cost. Frequently, additional imaging with the CAT or MR scan is not necessary.
When attempting to confirm PHA, the source of the bacteremia should always be investigated without forgetting the oral cavity, as well as other causes like the endocardium and the abdominal cavity. Given the presence of AHA in tropical countries, there the first step is to rule out this etiology and later search for other causes (16,17,20). When PHA is suspected, drainage must be performed with the help of an ultrasound and cultures of aerobic and anaerobic germs should be requested.
Conflict of interest
None declared by the authors.
Financing
None declared by the authors.
Acknowledgments
To the patient and his family for their cooperation.
References
1. Crippin JS, Wang KK. An unrecognized etiology for pyogenic hepatic abscesses in normal hosts: Dental disease. Am J Gastroenterol. 1992; 87:1740-3. http://doi.org/dkj3rs. [ Links ]
2. Brook I, Frazier EH. Microbiology of liver and spleen abscesses. J Med Microbiol. 1998; 47:1075-80. [ Links ]
3. Athavale NV, Leitch DG, Cowling P. Liver abscesses due to Fusobacterium spp that mimick malignant metastatic liver disease. Eur J Clin Microbiol Infect Dis. 2002; 21:884-6. [ Links ]
4. Vélez JR, Casabuenas J. La historia clínica. Un ensayo sobre el acto sumo del arte en la medicina. Sus elementos prácticos y sus fundamentos filosóficos. Bogotá: Prisma Asociados; 2006. [ Links ]
5. Huang CJ, Pitt HA, Lipsett PA, Osterman FA, Lillemoe KD, Cameron JI, et al. Pyogenic hepatic abscess: changing trends over 42 years. Ann Surg. 1996; 223:600-7. http://doi.org/cpzkqg. [ Links ]
6. Tsai FC, Huang YT, Chang LY, Wang JT. Pyogenic liver abscess as endemic disease, Taiwan. Emerg Infect Dis. 2008; 14:1592-600. http://doi.org/d4fd76. [ Links ]
7. Ohyama H, Nakasho K, Yamanegi K, Noiri Y, Kuhara A, Kato-Kogoe N, et al. An unusual autopsy case of pyogenic liver abscess caused by periodontal bacteria. Jpn J Infect Dis. 2009; 62:381-3. [ Links ]
8. Nozawa Y, Joshita S, Fukushima M, Sugiyama Y, Ichikawa Y, Kimura T, et al. A case of pyogenic liver abscess infected with Fusobacterium necrophorum depicted by microscopy and confirmed by tissue culture. Intern Med. 2011; 50:1815-9. http://doi.org/bdr3kw. [ Links ]
9. Weinstein MP, Reller LB, Murphy JR, Lichtenstein KA. The clinical significance of positive blood cultures: a comprehensive analysis of 500 episodes of bacteremia and fungemia in adults. I. Laboratory and epidemiologic observations. Rev Infect Dis. 1983; 5:35-53. http://doi.org/dnvsdx. [ Links ]
10. Washington JA. Collection, transport, and processing of blood cultures. Clin Lab Med. 1994; 14:59-68. [ Links ]
11. Cockerill FR, Wilson JW, Vetter EA, Goodman KM, Torgerson CA, Harmsen WS, et al. Optimal testing parameters for blood cultures. Clin Infect Dis. 2004; 38:1724-30. http://doi.org/cwxmzn. [ Links ]
12. Hwang JJ, Lau YJ, Hu BS, Shi ZY, Lin YH. Haemophilus parainfluenzae and Fusobacterium necrophorum liver abscess: a case report. J Microbiol Immunol Infect. 2002; 35:65-7. [ Links ]
13. Lei WY, Chang WH, Shih SC, Liu CJ, Shih CH. Pyogenic liver abscess with Prevotella species and Fusobacterium necrophorum as causative pathogens in an immunocompetent patient. J Formos Med Assoc. 2009; 108:253-7. http://doi.org/bbqtnq. [ Links ]
14. Nicholls RS, Restrepo MI, Duque S, López MC, Corredor AA. Standardization and evaluation of ELISA for the serodiagnosis of Amoebic Liver Abscess. Mem Inst Oswaldo Cruz. 1994; 89:53-8. http://doi.org/fp8pmj. [ Links ]
15. Pinilla AE, López MC, Castillo B, Murcia MI, Nicholls RS, Duque S, et al. Enfoque clínico y diagnóstico del absceso hepático. Revista Médica de Chile. 2003; 131:1411-20. http://doi.org/c6xfrn. [ Links ]
16. Pinilla AE, López MC, Ricaurte O, Castillo B, Murcia MI, Nicholls RS, et al. Liver Abscess Caused by Ascaris lumbricoides: Case Report. Rev Inst Med Trop S Paulo. 2001; 43:303-6. http://doi.org/bqgvwd. [ Links ]
17. Lodhi S, Sarwari AR, Muzammil M, Salam A. Smego RA. Features distinguishing amoebic from pyogenic liver abscess: a review of 577 adult cases. Trop Med Intern Health. 2004; 9:718-23. http://doi.org/c47wc4. [ Links ]
18. Stanley SL. Amoebiasis. Lancet. 2003; 361:1025-34. http://doi.org/c7jh6z. [ Links ]
19. Marín E, Pinilla AE, López MC. Absceso hepático amebiano. Revisión de 100 años de esta patología en Colombia. Acta médica colombiana. 2000; 25:218-26. [ Links ]
20. López MC, Quiroz DA, Pinilla AE. Diagnóstico de amebiasis intestinal y extraintestinal. Acta médica colombiana. 2008; 33:75-83. [ Links ]
21. Wagner KW, Schön R, Schumacher M, Schmelzeisen R, Schulze D. Case report: brain and liver abscesses caused by oral infection with Streptococcus intermedius. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 102:e21-3. http://doi.org/d974bz. [ Links ]
22. Kajiya T, Uemura T, Kajiya M, Kaname H, Hirano R, Uemura N, et al. Pyogenic liver abscess related to dental disease in an immunocompetent host. Intern Med. 2008; 47:675-8. http://doi.org/br8fss. [ Links ]
23. García CI, de la Teja E, Ceballos H, Ordaz JC. Infecciones faciales odontogénicas. Informe de un caso. Revista odontológica mexicana. 2009; 13:177-83. [ Links ]