Introduction
Proprioception is understood as the ability of the joint to determine position in space and detect movement (kinesthesia) and the sense of resistance acting on it 1. It is also considered an integrative quality of movement 2 that depends on specific structures, which allow signaling to register and respond to somatosensory information and its changes 3.
This quality is affected by amputation, defined as the complete and definitive resection of part or a complete limb (2). Therefore, a peripheral alteration leading to loss of static support structure, of the dynamic joint complex function and sensory, exteroceptive and proprioceptive information are presented 4.
As transtibial amputation is more prevalent in Colombia, this research focuses on this type of amputation, which causes ankle joint proprioceptors and plantar skin receptors loss. This generates changes that directly or indirectly affect proprioception 5, so physiotherapeutic management is required. Specific tools are necessary to assess the current proprioceptive condition of subjects with amputation and the impact of physiotherapy on intervention, since, after conducting a literature review and consulting with experts on the management of amputee patients in different institutions around the country, no information was found about the existence of such tools to assess proprioception in amputees.
For this reason, the objective of this research is to propose and validate content and to propose a battery for proprioceptive assessment in transtibial amputees with prosthesis, to measure the alteration in proprioceptive response secondary to amputation, according to the specific characteristics and needs of people with this level of amputation.
Materials and methods
This work was structured as a descriptive-purposeful study, and was developed in four phases 1: literature review 2, classification and analysis of information 3, design and proposal of the battery based on the best evidence found, and obtaining content and construct validity 4.
Phase 1: Literature review
In this phase, a literature review of the research topic in different databases was conducted, which allowed us to establish the conceptual basis and clarify the key concepts. The PubMed, MEDLINE, Science Direct and PEDro databases were used for this.
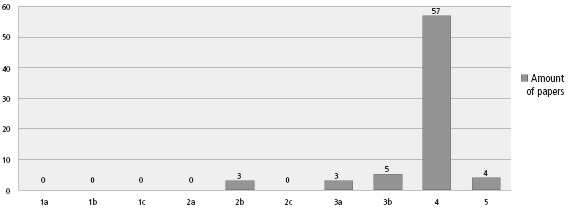
The research was conducted according to the Medical Subject Headings (MeSH), using the words ["amputation", "proprioception AND Amputation"], ["Evaluation AND Proprioception"], ["Evaluation AND Proprioception AND Amputation"]. Likewise, the search was limited to the last five years in English and Spanish languages (Table 1).
Table 1 Documents found and selected for the creation of the battery according to the revised databases.
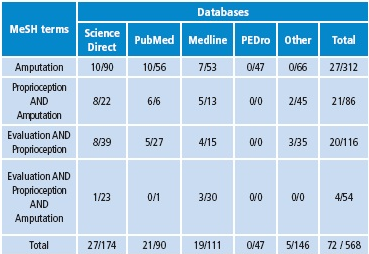
Source: Own elaboration based on the data obtained in the study
For protocol foundation, 72 original works were used and selected according to their affinity with the objective of this research, and following the inclusion and exclusion criteria established (Table 1).
Phase 2: Classification and analysis of information
After conducting the literature review, the found documents were evaluated according to the classification of the evidence proposed by The Centre for Evidence-Based Medicine in Oxford (CEBM) 6. Hence, selecting relevant information was possible for the conceptual basis of the construction of the assessment battery, framed in the literature found an in experience of professionals working with the amputee patients (Figure 1).
Selection of the population
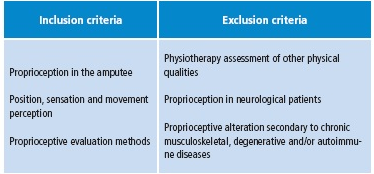
For this research, the target population consisted of the studies found in online databases, investigation records, graduation projects and thesis with sufficient information to generate the construct, which allowed stipulating the necessary components for the battery. The following inclusion and exclusion criteria were established (Table 2).
Phase 3: Propositive phase
Based on the information gathered from the best available evidence and expertise, the proposed design and validation of content and BEPAT construction was performed.
Seven specific tests were established for each item of the assessment battery to evaluate the different proprioception components taking into account the classification of the found evidence. This way, they can be supported and implemented in this population.
Phase 4: Content and construct validity
At this point, the degree in which the battery measures the proprioceptive condition of a subject with transtibial amputation with prosthesis was explored. Content validity is understood as a qualitative assessment of the questionnaire scope, that is, if it covers all dimensions of the phenomenon to be measured, since an instrument is considered to be content valid, if all aspects to be measured are contemplated 7. Now, construct validity is defined as the degree to which an instrument measures the evaluative dimension for which it was designed. This validity determines the relationship of the instrument with theory and theoretical conceptualization 7.
Results
The result of this research was the proprioceptive assessment battery for the population described. This is complemented by a format for general assessment of the current condition of the patient, the manual application, and the content and construct validation phase done with expert opinion.
Battery for proprioceptive assessment in transtibial amputees with prosthesis - BEPAT
The assessment battery was determined according to the components of proprioception: statesthesia, kinesthesia and effector activities 8. By performing seven tests, evaluating different specific components of proprioception, through proprioceptive receptors was sought. They shall be made in bilateral, passive and active way, with and without using prostheses in static and dynamic conditions, which will determine the proprioceptive condition of subjects. Thus, the following tests were proposed:
Test to the Golgi tendon organ (GTO)
GTO is located in the tendon structure that responds to muscle stress. The percussion of a tendon is the stimulus that leads to a rapid and instantaneous stretching of muscle and tendon receptors sensitive to stretch. So they transmit an energetic and synchronous signal to large motor neurons α in the dorsal horn of the spinal cord, through rapidly conducting afferent fibers, namely, myelinated fibers. The axons of these large motor neurons α are the efferent pathway that produces an immediate, short and involuntary muscle contraction 1.
This test is performed by direct percussion of the patellar tendon 3. The patient should be placed in a sitting position on a chair or couch. In addition, the therapist must directly strike on the patellar tendon, whose expected response is leg extension. The record of this test will depend on the intensity of the motor response.
It is important to note that if the response is hyperreflexia or clonus, the patient shall be deemed with a neurological disorder and, thus, a modification based on their proprioceptive response will be presented 9.
Joint position sense test
The test to measure joint position is based on accuracy to replicate and detect a position, on both active and passive form 1. Some of the tests seek to identify the replication error or the sensitivity of a position; the higher the error, the more evident altered proprioception is 10. This is one of the most common and easier proprioception measurement 11 tests.
Also, it seeks a passive movement in the knee joint, after removing visual signals 12. This is done because the joint position sense (JPS) provides the body with information about the speed and direction of active and passive movements without visual control 13. In this regard, studies using this test to measure the statesthetic direction 14, based on position sense through mechanoreceptor sensations, have been reported 15. The test aims to make the subject identify the position of the leg from a passive movement, as well as to make an active move to a position determined by the therapist.
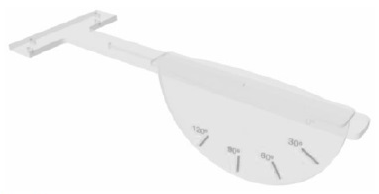
For this test, an angular identifier was designed (Figure 2). This instrument was designed in acrylic material, a movable semicircle with demarcations at angles 0°, 30°, 60°, 90° and 120°, corresponding to the five positions established in the test. Its design allows direct support to the stretcher, which facilitates manipulation by the evaluator.
Angular reproduction test
Assessment of joint reproduction is another sub-modality of proprioception, whose measurement is done through the identification of a static joint angle with replication methods 16.
This test is a variable of the test mentioned above. It is performed with and without prosthesis in a sitting position with the angular identifier referred to in the joint position test. This will be actively done on the limb to be evaluated; the subject maintains the position for a few seconds and goes back to the initial position 11 through the reproduction of movements at specific angles 13. At this point, that the subject replicates movement is intended after having passively perceived it in the contralateral limb, that is to say, if the leg to evaluate is the left leg, the therapist must perform the movement with the right leg and keep it at one of five positions established.
Unipodal test
With these tests, response of joint receptors and vestibular system is evaluated, which allows maintaining unipodal position due to the changes in acceleration and speed in body adjustments, necessary to achieve muscle activation demanded by this type of testing 3. Similarly, the test on one foot has been widely used for the measurement of functional joint stability, because it reproduces the forces encountered during activities in a controlled environment 8. It also seeks to determine the time that the person keeps unipodal visual position without support on different surfaces: stable 3 and unstable 15-16, as shown in Figure 3
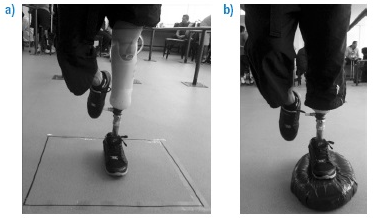
Figure 3 Example of the unipodal support test a) stable surface, b) unstable surface. Source: Own elaboration based on the data obtained in the study
It is important to clarify that the maximum support time for a healthy leg is 1 minute and 30 seconds on the prosthesis. This was determined according to reports indicating that a percentage of unipodal support on the lower limb with prosthesis decreased significantly compared to the healthy lower limb 4. In addition, the subjects had difficulties in assuming the load the lower limb with prosthesis, caused by alterations in soft tissues affected by amputation and which could be related to a deficit in the support function of body weight, at the level of the lower limb with prosthesis and particularly in knee instability of the sagittal and frontal planes 4.
Muscle spindle test
This test complements the unipodal test since both are performed simultaneously, on unstable and stable surfaces. It also provides information on the activation time and amplitude of the response of the muscle spindle 17.
The muscle spindle is a proprioceptive receptor located in the muscle structure. It senses the length or stretch degree, the mechanical stimulation degree and the speed at which stretching is applied. Similarly, it sends this information to the central nervous system and indirectly influences voluntary muscle control and agonist-antagonist muscle synergy 11,16.
The test is conducted through surface electromyography (SEMG) 18. This technique detects and analyses the electrical potential produced during muscle contractions. Thus, surface electrodes transmit information regarding muscle activation. Such is the case of the intensity of muscle contraction, myoelectric manifestation of muscle fatigue and recruitment of motor units, for, subsequently, manifesting activation of muscle spindle 19. To achieve this, a set of five electrodes should be placed as follows: two in the hamstring, two in the extensor muscle group of the knee and one grounding on the tubercle of the tibia 19. For this test, data on activation time and amplitude values that give information about recruitment and muscle activation, will be reported.
Step test
The next test is based on some principles of cognitive therapeutic exercise (Perfetti method), where each change of position involving support transfers and postural adjustments requires tone, sensation and predisposing factor adjustment for controlling body movement 20-21. This is based on sense and movement control, and is done by simultaneously establishing a unilateral load support to release contralateral motor control and allow movement. The notion of load support and alternating discharge represents a high level of perceptual-motor control 20.
Also, techniques grade one and two, which serve the purpose of the tests, were chosen 21:
Grade two
Postural adjustments due to pressure support and identification of external resistors.
The subject is placed in step position, moving back and forth with one leg. Steps will be taken on different platforms. The test will be conducted with closed eyes and in two phases:
Different tension surface: The objective of this test is to identify the differences in resistance of the surfaces to which the subject will be exposed. Three oval rubber platforms with different levels of hardness (density) will be used: they are known as stability trainers and have a progressive resistance system depending on colorimetry.
Surfaces of different heights: The objective of the test is to identify the difference in angular position of the knee according to the different heights in which the foot is placed in step position. Three square platforms (30x30cm), with thickness of different calibers between 3cm, 6cm and 9 cm, made in microporosa, (a high density, inert and nonporous foam), that is ideal because of its ability to absorb vibrations and impacts, will be used. Several studies, which seek to identify different degrees of movement in the knee joint have been found 15. Therefore, each height is related to the degrees of movement of the knee joint. The 3 cm platform relates to approximately 25º of flexion; the 6cm platform with 35° of flexion and the 9cm platform with approximately 45° of flexion. This generates perception of different heights, based on the knee movement when retained after a transtibial amputation (Figure 4).
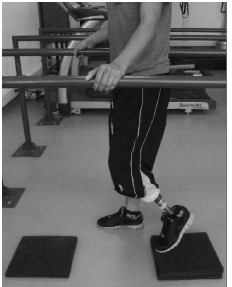
Figure 4 Example of the step position test on surfaces with different heights. The patient must take a step forward and one step back depending on the orders provided by the therapist, and without visual aids; therefore, platforms should be perceived in advanced. Source: Own elaboration based on the data obtained in the study
Rating scale: Each item is rated on a numerical scale of 0, 1 and 2, which changes according to the data (number of attempts, time, among others). Each item will be given a differential rating for each of the lower limbs. A sum of the scores obtained in each test is obtained; the maximum score is 36 points for each leg. This, in turn, will be classified according to proprioceptive response into five categories in the final results table (Table 3).
Table 3 Classification of the proprioceptive response according to the numerical grade.
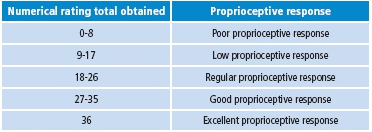
Source: Own elaboration based on the data obtained in the study
For application of the battery, a manual to describe the necessary instructions for the implementation of each test was created. It also has information about materials and instruments, patient position, therapist position, verbal commands, test records and scores 22.
Content and construct validity
This process was carried out solely through a survey with questions regarding relevance, clarity, precision, reproducibility, records and scores for the tests. Then, the battery was sent to 10 experts in amputee management from the International Committee of the Red Cross, Universidad Autónoma de Manizales, Escuela Colombiana de Rehabilitación, Centro Integral de Rehabilitación de Colombia (CIREC, for its acronym in spanish), Servicio de Prótesis y Amputados del Hospital Militar Central, Universidad del Rosario, Laboratorio de Órtesis y Prótesis Gilete; seven surveys answered by these institutions were returned.
The analysis was performed taking into account the criteria established by Palisano in 1996, cited in Alvis et al.3, who claimed that the percentage established to determine content validity corresponds to 60% for each question. It is important to note that the favorable percentage was directly related to the experts who agreed with the proposed battery and that the total number of experts who answered each item was taken as 100%. For all items in the battery, content and construct validity was determined, since results were above 70%.
Discussion
The items included in the battery of proprioceptive assessment in people with transtibial amputation, and prosthesis-BEPAT allow determining the response of the sensorimotor system including the afferent component, based on the proprioceptive receptors, the integration process and efferent responses 1, which influence the proprioceptive response of the subject.
Each proposed item correlates to activation of proprioceptive receptors 13-15 involved in the execution of each test. This measurement allows quantifying and qualifying proprioceptive response in static and dynamic situations. This has been proposed by some authors to classify the degree of alteration in the proprioceptive response 8,11,24-27.
This proposal, where assessment is bilateral, includes the Golgi tendon organ test 1,3, the joint position 10-11 and angular reproduction test 13,16, unipodal position on different surfaces 8,15-16 and evaluation of neuromuscular spindle 17 since, according to evidence reports, their use in the measurement of proprioception in individuals without structural alteration 28-29 has been documented, although they are also used in other musculoskeletal disorders 10,13,15,22. The application of these tests is possible in transtibial amputees since the preserved knee joint has mechanoreceptors and proprioceptors that allow signaling somatosensory information, even with structural loss and associated functional changes 2. However, residual activity of receptors in the knee joint 23 generates the perception of movement and control in space, along with new body image caused by the use of the prosthesis.
On the other hand, bilateral assessment offers a differential rating to each lower limb, showing proprioceptive alteration secondary to structural loss 2 after transtibial amputation. In turn, the evidence generated with the use of prosthesis, according to some experts, allow subjects to perceive more easily the movements made. Molina 4 addressed the issue of unipodal support on the healthy limb and on the prosthesis and found that, despite structural loss, a person with a prosthesis tolerates unipodal support, even if the duration is less than that of the healthy leg. This supports the proposal for a unipodal support test for transtibial amputees and sets a shorter time for the limb with the prosthesis.
Regarding the additional test conducted for unipodal support of the muscle spindle 18 through SEMG, it is possible to say that this instrument manages to record directly muscle spindle activity and complements proprioceptive information to establish the condition of the subject. Experts suggest that this test will depend on how easy it is to access the device. However, based on research proposals, the results obtained with the test quantify the activity of this receptor, known as one of the main proprioceptors.
Several studies mention the importance of a dynamic assessment of proprioception 11,13, since it depends on three key components: statesthesia, kinesthesia and effector activities 8, which are the reason for the creation of a test whose proprioceptive receptors assessment, as a whole, is done in a dynamic situation by taking back and forth steps 20-21, which is related to the perception of different tensions and heights. This information is collected by the aforementioned residual receptors. The results of this research show the articulation of the response obtained from each proprioceptive receptor in the development of functional activities, which allows control of body and movement, along with the use of the prosthesis.
In the process of content and construct validation, no differences were found regarding the views of experts on battery tests; instead, approval of all the proposed items was obtained and recommendations to facilitate the use and battery application were provided. Some of the suggestions related to application in clinical settings may be used for a pilot test.
Scarce published evidence about the proprioceptive assessment in people with structural alterations is one of the limitations of this research.
Conclusion
This study found that proprioception is a fundamental quality for managing amputee patients because it provides a sense of movement, body control and adaptation to the new body image caused by the use of the prosthesis. Therefore, it is necessary that both proprioception and other qualities of movement go through a specific evaluation process before intervention. In addition, the proprioception assessment process will help to improve the prescription of the prosthesis, the success of the rehabilitation treatment and the participation of individuals in their environment.
Creating a proprioceptive assessment battery applicable to amputee population allows obtaining objective, qualitative and quantitative information on functional disorders affecting body movement. Thus, the investigative processes that can update the tools proposed by physiotherapy for assessment of amputees are strengthened.
Finally, further validation of the battery is recommended through a pilot test with an adequate population sample that allows data collection and completion of each corresponding weighted item of the battery. Also, inter- and intrarater reliability testing should be performed.
It is important to further the research process on proprioception assessment to expand the field of study and to be able to have more useful and reliable measurement tools.