Introduction
Leishmaniasis is an infection caused by an intracellular flagellated protozoan transmitted by the bite ofhematophagous mosquitoes belonging to the family Psychodidae, genera Phlebotomus and Lutzomyia.1 Around 20 Leishmanial species have a pathogenic potential for humans, and also have the ability to infect mammals of different species and generate both cutaneous and visceral involvement. 2-4
Leishmaniasis is considered an endemic pathology in around 70 countries; however, notifying it as an event in public health is mandatory only in 32 of them, which is why its actual incidence is underestimated. 5 The World Health Organization estimates about 1.3 million new cases and 20 000 to 30 000 deaths per every year, mostly due to visceral involvement. 6 Cutaneous leishmaniasis is the most common form of the disease and occurs in exposed body regions causing ulcerative lesions and poor healing processes. 7,8 95% of the events related to this form occur in the Americas, the Middle East and Central Asia, being Afghanistan, Iran, Algeria, Syria, Brazil and Colombia the most affected countries. 6
In Colombia, the incidence of leishmaniasis is high and exceeds 12 000 cases per year; its geographical distribution involves a large part of the country. 9-11 The species L. panamensis, L. guyanensis, L. braziliensis, L. amazonensis and L. mexicana have been associated with the cutaneous and mucocutaneous form of the disease and are responsible for most cases. 12,13
According to the epidemiological bulletin of the Instituto Nacional de Salud (National Institute of Health) of Colombia, Boyacá ranks ninth countrywide regarding new cases documented in 2016, which is above the national average, being the municipalities of Otanche, San Pablo de Borbur, Pauna, Quípama and Puerto Boyacá the places with the highest number of cases reported. 14,15 This distribution puts the department at a medium risk for the occurrence of the event.
Currently, several pharmacological treatments are available in the guidelines of the Instituto Nacional de Salud to manage leishmaniasis optimally, which range from local therapies to systemic medications. 16,17 However, there is no single drug that effectively treats all Leishmania species, nor the conditions they cause. 4,18 Furthermore, the development of new compounds is limited because the most affected population is under poverty conditions and, in turn, have greater difficulty for accessing health services. With this in mind, the implementation of new drugs may represent a high acquisition cost, thus affecting mostly this type of population. 19
Pentavalent antimonials used as pharmacotherapy to treat cutaneous leishmaniasis continue to be the first management option. 16,20 Meglumine antimonate is the most used and is recommended in the guidelines of the Instituto Nacional de Salud as the first option for the management of this disease in Colombia. 3,21,22 The average dose is 20 mg/k once a day, though local or systemic application for 20 or 30 days, depending on the route of administration of the drug, being shorter in the case of systemic therapy and longer in the case of local application. 3,19
It is possible to observe therapeutic failures caused by low adherence, drug resistance and the use of subtherapeutic doses, which, in turn, are related to three factors: lack of knowledge on the part of the treating health personnel about the doses and presentation of the drugs; lack of dose adjustment according to the patient's weight during the treatment; and lack of follow-up. 19 Moreover, another factor is treatment abandonment due to local side effects such as pain at the site of application, arthralgias, myalgias and even organic involvement manifested through liver and kidney failure and disorders in the electrical conduction system of the heart, which in some cases may seriously compromise the health of patients. 8,23
This study aimed to make an epidemiological approach, not only to the distribution of the disease in Boyacá, but to its behavior and the factors that determine its occurrence in the affected population. In short, the objective is to describe the behavior, geographical distribution and initial clinical management of cutaneous leishmaniasis in the department of Boyacá between 2008 and 2015.
Materials and methods
A descriptive, retrospective study was carried out. Considering that the event is notifiable, the information generated on a regular basis through the notification form of the Epidemiological Surveillance System (SIVIGILA by its acronym in Spanish) allowed obtaining data on sociodemographic, clinical and geographical distribution conditions of the patients diagnosed with cutaneous leishmaniasis.
The study included users who were reported to SIVIGILA as confirmed cases of cutaneous leishmaniasis in the 123 municipalities of Boyacá between 2008 and 2015 and had complete epidemiological records. Patients that acquired the infection in a department other than Boyacá were excluded.
The analyzed variables were age, sex, weight, occupation, place of occurrence of the case, health insurance system, ethnicity, place of origin, number and location of cutaneous leishmaniasis lesions, previous hospitalization, previous treatment, estimated dose per day and total number of vials administered.
Statistical analysis
Statistical analysis of demographic and clinical conditions was performed using the IBM SPSS program (Chicago, Illinois) version 23. Univariate and bivariate analyses of the aspects established in the categorization of the variables were carried out. Qualitative variables such as sex, geographic area, ethnicity, health insurance system, among others, were analyzed using absolute and relative frequencies. On the other hand, quantitative variables were processed through measures of central tendency.
An analysis was made taking into account the geographical distribution of the cases reported in Boyacá between 2008 and 2015. A color scale was used: green for municipalities with 1 to 8 cases, yellow for 9 to 16 cases, orange for 17 to 24 cases and red more than 25 cases. To elaborate the maps with the geographic distribution of the patients affected by cutaneous leishmaniasis, the EpiMap extension of EpiInfo was used.
Regarding clinical management of patients, criteria for locating the lesions were determined by means of frequency analysis. This was confirmed by weight and the amount of doses in milligrams -if the patients received an adequate initial dose-, and the amount of vials during the chemotherapy period established according to the protocol of the Instituto Nacional de Salud (National Health Institute) of Colombia. Data were obtained from calculating the initial dose per day adjusted by weight for each patient. Then, the number of vials that should be administered during the 20 days of treatment was established taking into account that the excess content of each vial per day should be discarded and compared with the estimated initial dose recorded in the notification form and the total amount of vials administered to each patient.
Ethical considerations
This study was elaborated following the guidelines of the Council for International Organizations of Medical Sciences. This research is risk-free according to Resolution 8430 of 1993 of the Ministry of Health Colombia, which establishes scientific, technical and administrative regulations for health research. 24 Moreover, confidentiality, respect and security of the information were preserved at all times during its processing. However, authorization from the Ministry of Health of Boyacá, Public Health Surveillance Area, was requested to access the databases. The research protocol was presented to the Ethics Committee of the Universidad de Boyacá.
Results
Sociodemographic conditions
Out of 949 epidemiological records found, 40 were excluded due to poor quality of the data or lack of data. The analysis included 909 files correctly entered in the system. The average age was 23 years (σ: 19, min-max: 4-52), and 429 cases (47.2%) occurred in the 0-18 age range; of these, 155 cases (17%) occurred in the 0-5 range. The general distribution of affected individuals determined by life cycle is shown in Table 1, which makes evident that adults (29 to 59 years) were involved in 26.5% of the cases. Regarding sex, except for children (6 to 11 years), men (63.6% of the total sample) were more involved in this type of cases than women.
Table 1 Sociodemographic conditions and age group of patients diagnosed with cutaneous leishmaniasis in Boyacá, Colombia. 2008-2015.
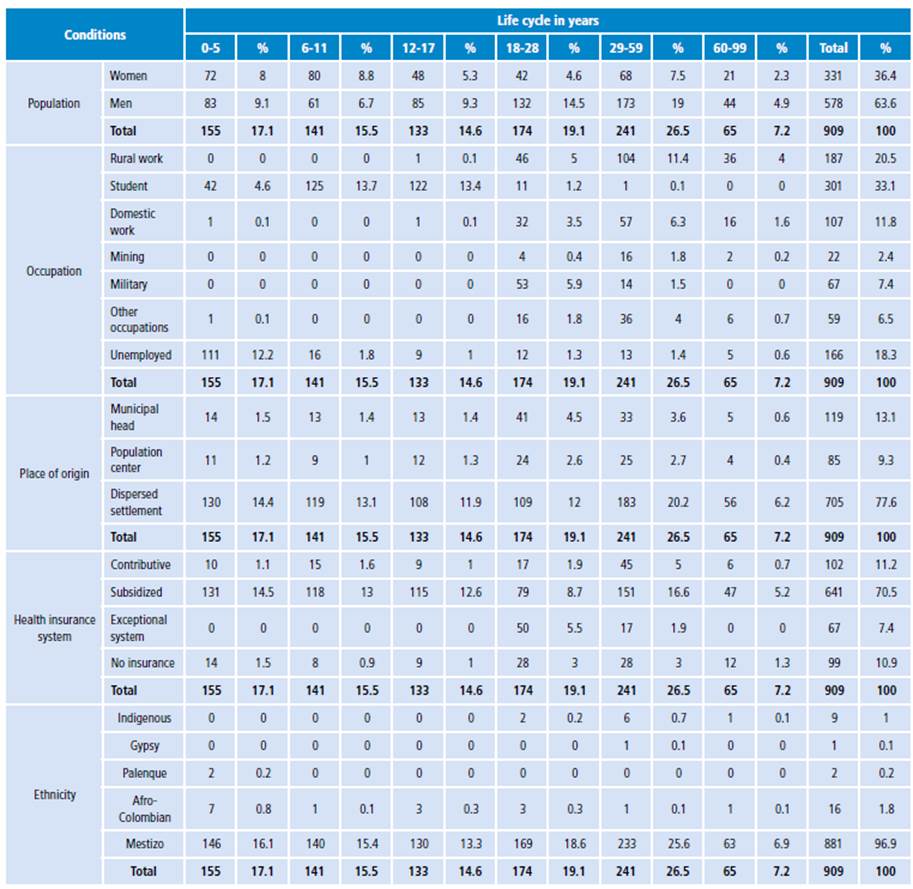
Source: Own elaboration based on the data obtained in the study.
According to the place of residence of the patients, three classifications were used: municipal head, population center and dispersed settlement, the latter being the most affected with 75% of the cases.
Most subjects affected (71.9%) were students, people without a specific occupation and workers in rural areas, most of them enrolled in the subsidized system (70.5%) ofthe General System of Social Security in Health. The most frequent ethnicity (96.9%) was specified as "other" in the compulsory notification sheet, which corresponds to cross-breeding between natives and Europeans during colonial times (mestizo).
Geographical distribution
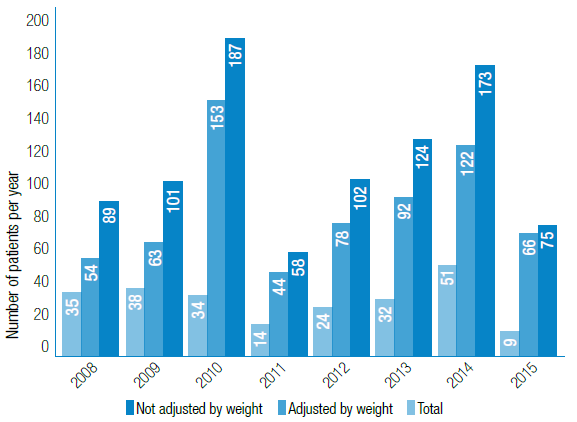
When analyzing notifications issued during the 8-year period under study, a varied behavior was observed, showing two major peaks in 2010 with 187 cases and 2014 with 173 cases, in contrast to 2011, when only 58 cases were recorded (Figure 1).
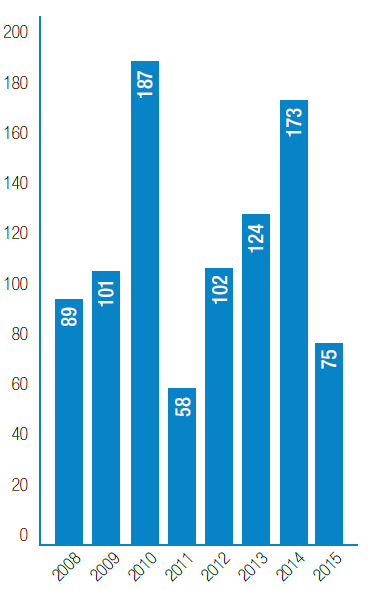
Source: Own elaboration based on the data obtained in the study.
Figure 1 Number of cutaneous leishmaniasis cases reported per year in Boyacá, Colombia. 2008-2015.
Figure 2 shows the behavior in the municipalities that reported cases of cutaneous leishmaniasis during the study period. This information allowed to determine that 5 of the 123 municipalities of the department presented the highest number of cases, being the municipality of Otanche the one that reported the highest prevalence with 344 cases (37.8%), followed by San Pablo de Borbur with 139 (15.3%). It should be noted that these five municipalities account for 81% of the total cases reported during the study period.
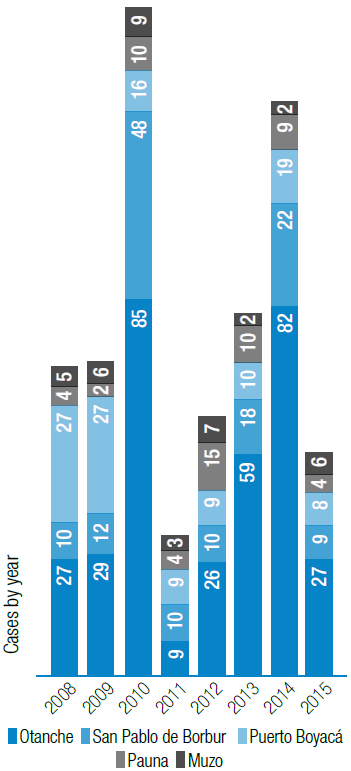
Source: Own elaboration based on the data obtained in the study. Initial clinical management
Figure 2 Municipalities with reports of patients with leishmaniasis in Boyacá, Colombia. 2008-2015.
According to the geographical distribution analysis, the municipalities with the highest number of cases are located in the western province during the entire period, especially in the municipalities of Otanche, San Pablo de Borbur, Puerto Boyacá and Pauna. The maps also show some cases of municipalities that have no risk for the event, among them Chiquinquirá, Chita, Duitama, El Cocuy, Nobsa, Panqueba, Saboya, Sogamoso, Tibasosa and Ventaquemada (Figure 3).
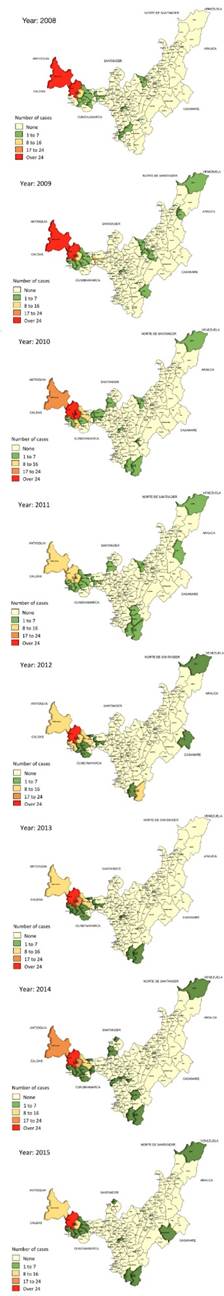
Source: Own elaboration based on the data obtained in the study.
Figure 3 Geographical distribution of cutaneous leishmaniasis cases in Boyacá, Colombia. 2008-2015.
The number of cutaneous leishmaniasis lesions is variable: 665 cases (73.1%) had a single lesion; 179 (19.7%) had two; 57 (6.3%) had three and 8 (0.8%) had four or more. The presence of lesions was greater in upper and lower limbs with a total of 482 (53%) and 333 (36.6%) cases, respectively. 247 (27.2%) patients had lesions on the face and 162 (17.8%) on the trunk. The sum of injuries is greater than the number of patients because some individuals were affected by injuries that involve more than one body segment or have more than one injury.
Initial clinical management
The number of cutaneous leishmaniasis lesions is variable: 665 cases (73.1%) had a single lesion; 179 (19.7%) had two; 57 (6.3%) had three and 8 (0.8%) had four or more. The presence of lesions was greater in upper and lower limbs with a total of 482 (53%) and 333 (36.6%) cases, respectively. 247 (27.2%) patients had lesions on the face and 162 (17.8%) on the trunk. The sum of injuries is greater than the number of patients because some individuals were affected by injuries that involve more than one body segment or had more than one injury.
The percentage of patients infected and previously hospitalized due to leishmaniasis was 3%. Similarly, a history of previous treatment was found in 9.6% of the total of patients included in this study. Figure 4 shows the number of subjects who received adequate and inadequate treatment regarding the therapeutic dose according to the weight in kilograms discriminated per year. Of the total cases, 73.9% received the number of vials required according to their weight during the study period. The lowest rate of error in the calculation of the initial dose (12%) was observed in 2015.
Source: Own elaboration based on the data obtained in the study.
Figure 4 Pharmacological treatment with meglumine antimonate, calculated according to the guidelines of the Colombian Ministry of Health and Social Protection and discriminated by year in patients with cutaneous leishmaniasis from Boyacá, Colombia. 2008-2015.
Discussion
The results of this study indicate that leishmaniasis is a disease that affects young people, residents of rural areas, who work in forested areas, which coincides with Cella et al.25 and Bsrat et al.26 Regarding sex, it was more frequently observed in men, which is similar to the reports found in the works carried out by Cella et al.25, Soares et al.27, Aguado et al.28 and Cota et al.29
As in the studies of Cota et al.29 and Pontello et al.30, the body areas most affected by cutaneous leishmaniasis are the upper and lower limbs. The number of predominant lesions in the subjects of this study was one injury, which coincides with Blanco et al.31.
Regarding geographical distribution, a high number of cases was observed in the western province, especially in the municipalities of Otanche, San Pablo de Borbur, Puerto Boyacá and Pauna, which have been classified by other studies as critical sites for the presence of vectors infected by the Leishmania parasite. 32
Pentavalent antimonials were the drugs used in the patients included in this study, mainly meglumine antimoniate. Some findings include inadequate dosing in over 25% of the cases due to deficiencies in the calculation of the initial dose of the treatment. Such situation may have a negative impact on the health of patients since it is considered a risk factor for resistance to the action of the compounds used in the management of leishmaniasis. 33,34 Inadequate pharmacological therapy for this pathology is a widely recognized problem in the current medical literature; however, there are no studies to compare our results in this regard, since no research addresses the initial clinical management performed on patients affected by cutaneous leishmaniasis. Mohapatra 33 states that the lack of knowledge of physicians about the presentation, dose and duration of treatment is one of the main causes of resistance to antileishmanial drugs in developing countries.
This study did not include any follow-up information regarding the treatment of patients because data were taken from the SIVIGILA notification sheets and there are no sections that allow for a clinical follow-up or cure criteria; therefore, it was impossible to assess the efficacy of pharmacological management and verify the healing process of patients whose cases were notified as confirmed leishmaniasis. Furthermore, there was no record of the doses applied to patients per day, which is decisive for the management of this pathological entity, since a 20-day duration and not proving its application may lead to failures during the administration of the treatment and complications such as drug resistance.
One of the limitations of this study is the lack of an instrument for monitoring the clinical picture of patients affected by cutaneous leishmaniasis in Boyacá, Colombia. In spite of that, this study aimed at updating the existing information regarding the epidemiological behavior and geographical distribution of leishmaniasis in Boyacá. In addition, a description of the initial pharmacological treatment was established to provide recommendations to health decision-makers at the regional and national levels in order to correct inadequate behaviors and encourage other authors to study vector-borne diseases in greater depth. There are still shortcomings in the identification and management of these cases, which constitutes a problem of interest for public health.
Conclusions
Findings related to the type of presentation and behavior of the disease are similar to other works, which lead to believe that its behavior is as expected. West Boyacá is the region most affected by leishmaniasis in the department; five of the municipalities in this area are classified as critical due to the high presence of infected vectors, which may be related to the geographical location and the influence of fluvial sources. This last point must be taken into account when developing strategies for the epidemiological control of the disease.
Regarding initial management, and in spite of the guidelines for diagnosis and management, the lack of knowledge of the treating medical personnel has led to inadequate management in 1 of every 4 patients diagnosed who have been treated with subtherapeutic doses, causing failures that result in recurrences.
Once again, there is a need to create a public health surveillance instrument that not only collects report data but also adherence monitoring and medication administration, as well as the occurrence and management of collateral effects and complications of the disease.
Regulating entities should detect failures in the notification files of the disease, because when a clinical and pharmacological follow-up is required, it is necessary to modify these documents to improve surveillance and control processes of cutaneous leishmaniasis. Efficient training of the treating medical personnel and the health team that interacts with these patients is essential to reduce the rates of treatment failure.














