Introduction
Scleroderma is a disease classified as localized and systemic; the latter has two variants: diffuse cutaneous systemic sclerosis (dcSSc), which is characterized by the rapid development of symmetric dermal thickening in the proximal and distal areas of the limbs, face and trunk, and limited cutaneous systemic sclerosis, which is characterized by symmetric dermal thickening limited to distal areas of the limbs and face. 1,2
In general, systemic sclerosis (SSc) is an autoimmune disease of the connective tissue, clinically characterized by dermal thickening due to the accumulation of connective tissue and may involve other organs. The etiology of this disease is multifactorial and is caused by the interaction of alterations in the immune response, excessive extracellular matrix remodeling and the presence of proliferative vasculopathy, all this under genetic and environmental influence. SSc has an estimated prevalence of 10 cases per 100 000 inhabitants, which is why it is considered a rare disease, with an incidence of 4-8 cases per 10 000 inhabitants, affecting mostly women with an average age of 45 years. 1
SSc is characterized by fibrosis that causes the thickening and hardening of the skin and other tissues. It starts with an endothelial injury and a subsequent imbalance of its repair, generating a cascade of proinflammatory events and hyperactivation of fibroblasts that constitute abnormal extracellular matrix clusters in different tissues and degrees, and almost always affecting the gastrointestinal tract, lung, kidney, heart and skin. In addition, it is associated with mortality when it manifests with interstitial lung disease and pulmonary arterial hypertension. 2
This skin condition causes lesions ranging from digital ulcers (DU) to facial atrophy, which are susceptible to management by plastic surgery. With this in mind and considering the difficulties that could arise regarding medical and surgical management of skin lesions, hand involvement and facial alteration, this work describes the results of a detailed literature review, presenting the best therapeutic options for these patients from the point of view of plastic surgery.
Etiopathogenesis
Vascular proliferative disease
Endothelial activation has been demonstrated through the detection of increased plasma levels in intercellular adhesion molecules, endothelin 1, thrombomodulin and von Willebrand factor expression, associated with excessive apoptosis of endothelial cells. When this injury becomes chronic, platelet adhesion, leukocyte adhesion and activation of the fibrinolytic system occur, which together with the increase in vascular permeability lead to deterioration of the vascular wall. 3
This process causes excess extracellular matrix, which leads to fibrosis and subsequent loss of tissue elasticity and reduction of vascular lumen, which ultimately result in hypoxia and tissue necrosis. Angiogenesis, when trying to supply by perfusion, produces an aberrant formation of capillaries, which is secondary to an imbalance between angiogenic and angiostatic factors. Microvasculopathy is reinforced by hyperplasia of pericytes, responsible for inhibiting cell migration and vascular proliferation. 3
Fibrosis
The bone marrow contributes to an increase in the number of pre-fibroblastic cells through the release of pluripotent mesenchymal cells and progenitors of fibroblasts. Fibrocyte precursors migrate and accumulate in tissues according to the gradient of chemokine receptors (CRs) such as CCR3, CCR5, and CXCR4, which have been found at high levels in the skin of patients with dcSSc. The effector protein that orchestrates the whole process is TGF־pis, produced by fibroblasts, T cells, monocytes and platelets, which is released as a complex that is activated inside the ECM by the tissue injury. 4
Oxidative stress
Superoxide anions are produced during ischemic phenomena and, together with the activation of the NF-kB pathways, generate oxidative stress. Indirect markers of reactive oxygen species have been reported in serum analysis of patients with SSc, as well as oxidative proteins and lipid peroxidation. 3
Immune system
Alteration of humoral and cellular immunity is demonstrated by the presence of B lymphocytes with chronic CD19 and CD85 labeling, manifested by specific autoantibodies -such as anticentromere antibodies (ACA), anti-topoisomerase I antibodies (also known as Scl70־ antibodies) and anti־RNA polymerase III antibodies- and alterations in the function of fibroblasts. ACA are characteristic in localized sclerosis, which is usually more benign than the diffuse form, even though it is associated with the subsequent development of pulmonary hypertension, digital ulcers and gastrointestinal involvement. 5
Genetic correlation
In general, the course of systemic rheumatic diseases is related to polymorphisms of the major histocompatibility complex -MHC or HLA-, associated, to a great extent, with class II antigens. 2 Genetic risk factors include protein tyrosine phosphatase (PTPN22), a non-receptor gene that produces susceptibility to SSc, diabetes mellitus type I, systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA). Other shared genes such as BANK1, IRF5 and STAT4 have also been reported. 6
Environmental correlation
Some of the risk factors that could be etiologically related to this entity, according to some case reports, are exposure to silica and organic solvents, permanent silicone implants and contact with infectious agents such as parvovirus B19 and cytomegalovirus. The association of these viruses with endothelial damage, given the infection and the poor response of adaptive immunity, may generate profibrotic cytokine production and cause vascular injury and activation of fibroblasts. 7,8
Classification
Scleroderma is classified as localized and systemic; the latter is divided into two categories according to the skin condition: limited scleroderma, characterized by ACA, and diffuse scleroderma, characterized by anti-topoisomerase I (Scl70). 1,2,5
Diagnosis
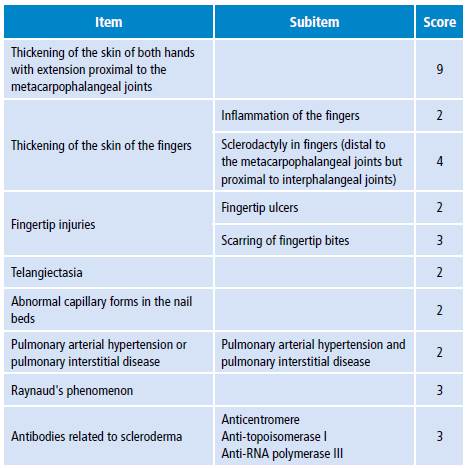
In 2012, the ACR-EULAR (American College of Rheumatology/ European League against Rheumatism) committee established new classification criteria for SSc (Table 1), which increased sensitivity from 0.75 to 0.91, and specificity from 0.72 to 0.92 with respect to the 1980 criteria. Given the heterogeneity of disease presentation, differentiating isolated sclerosis from disease overlap is often difficult. The range of overlapping diseases is between 10% and 27% of cases. 6,9
Based on the Canadian Scleroderma Research Group database, it was found that telangiectasias and ACA increase the sensitivity of SSc diagnosis from 57% to 97% in the presence of Raynaud's phenomenon (RP) and proximal skin thickening. Therefore, easily discernible clinical features (RP and telangiectasias), as well as serology, seem to be of considerable diagnostic value. 9
Thickening of the skin of the fingers and fingertip injuries have two possible manifestations; the highest score between both manifestations will be taken into account for categorization purposes in this case. The maximum possible score is 19 and patients with a score of 9 are classified as SSc. 10
Probable differential diagnoses that cause thickening of the skin should be considered, even if they do not appear symmetrically - as in the case of morphea (plaques, bullous and linear distribution), linear scleroderma en coup de sabre, progressive facial hemiatrophy and rigid skin syndrome- and diffusely -as is the case of eosinophilic fasciitis; storage diseases such as scleromyxedema, amyloidosis and nephrogenic systemic fibrosis; metabolic conditions such as phenylketonuria, cutaneous porphyria and hypothyroidism; toxic agents such as silica, polyvinyl chloride, bleomycin and toxic oil syndrome; and genetic etiologies such as progeria or Werner syndrome. 11
Comorbidities
The type and frequency of target organ involvement in patients with scleroderma are variable. The main organs affected include the cardiovascular system with pulmonary hypertension; the pulmonary system with pulmonary hypertension and pulmonary fibrosis; the gastrointestinal tract with esophageal alteration and involvement of the small intestine; the renal system with kidney failure; the joints with arthritis, arthralgias and calcinosis; among others. 12
Hand and systemic sclerosis
Manifestations of scleroderma in the hand include RP, digital ischemia, changes in the skin, calcinosis, and joint contractures.
In 1882, Maurice Raynaud was the first to describe a transient, acral, vasospastic phenomenon, induced by cold or stress, known as RP, which occurs in the fingers and toes and, less frequently, in the nose, ears and nipples; it may be asymmetrical and may not affect all fingers. 13,14 Typical changes in skin coloration include initial pallor, cyanosis and red fingers as an expression of the compensatory vasodilation phase. About 90% of patients with SSc suffer from RP. 15
There are two types of presentations associated with RP: primary and secondary. The presence of RP as the only symptom, without other concomitant connective tissue disease such as SSc, Sjogren's syndrome or SLE, is defined as primary RP. On the other hand, presentations associated with the connective tissue pathologies described above are defined as secondary RP. RP is a manifestation commonly associated with SSc in up to 95% of patients, in which peripheral vascular alteration and involvement of internal organs occur. It is necessary to make a differential diagnosis between primary and secondary RP in order to guide management, taking into account that the primary form is considered a benign pathology that can show significant improvements with topical and lifestyle changes (Table 2).
Table 2 Clinical characteristics of Raynaud's phenomenon in scleroderma.
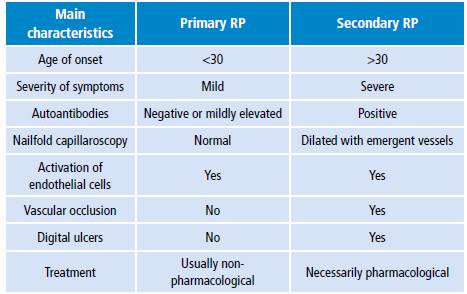
Source: Own elaboration based on Johnson. 10
Mild to moderate symptomatology with onset at an early age may suggest primary RP, while an increase in frequency and an extension in the duration of attacks, together with other symptoms such as dyspnea and dysphagia, are more suggestive of secondary RP. Signs such as sclerodactyly, telangiectasia, ulcerations and ACA (with or without a specific pattern) on physical examination help establish an SSc diagnosis (Figure 1). 16

Source: Own elaboration based on the data obtained in the study.
Figure 1 Proximal interphalangeal joint flexion contractures with thickening of the skin.
In order to establish a diagnosis, it is necessary to rely on the clinical history, carry out an adequate physical examination and perform complementary paraclinical examinations -color doppler ultrasound and nailfold capillaroscopy.
DUs are necrotic skin lesions on the soft part of the fingers or superimposed bony prominences. They occur in up to 50% of patients with scleroderma and are extremely painful, leading to substantial disability in the affected hand 17-19; they can develop in hands and feet.
DUs may develop due to multiple factors, including repeated microtrauma, thinning skin, dry skin and underlying calcinosis. However, chronic digital ischemia as an expression of unresolved RP is the most important risk factor for the development of ulcers in this group.
Calcinosis is the formation of calcium deposits in soft tissues - without direct joint involvement-, is more frequently associated with limited scleroderma and may be localized or extensive. The main complications associated with this pathology are skin ulcers and infection.
At the pathophysiological level, calcinosis is caused by tissue hypoxia that leads to a decrease in perfusion with subsequent inflammatory activity, which, in turn, triggers the activation of macrophages and imbalance between various mediators that produce an increase in the entry of calcium into the cells. 20
Joint involvement occurs almost always in the interphalangeal and metacarpophalangeal joints. Proximal interphalangeal joint flexion contractures are developed by retraction in the volar surface. 21 This often leads to skin breakdown on the dorsal aspect of the joint due to tension and thinning skin. Usually, metacarpophalangeal joints are fixed in extension or hyperextension. In contrast to proximal interphalangeal joint flexion contractures, it is believed that metacarpophalangeal joint position is secondary to capsular narrowing, capsule adhesion and extensor component. 21 Early initiation of hand therapy can help limit or delay the development of disabling contractures and digital skin ulcerations.
Treatment
The management of scleroderma of the hand should be carried out by a multidisciplinary team consisting of a hand surgeon, a rheumatologist, a dermatologist and a hand therapist. 22
Primary RP is considered a benign pathology that is not accompanied by structural alterations in most cases; therefore, complications such as DUs and gangrene should not be a frequently associated outcome. This phenomenon usually improves with non-pharmacological measures such as lifestyle modifications, which include suspending cigarette smoking, avoiding exposure to cold and wearing appropriate clothing and mechanisms to avoid psychological stress.
In cases of primary RP that does not improve with non-pharmacological measures or in secondary RP, pharmacological management should be initiated. At present, there are several pharmacological groups that, through different mechanisms of action, aim to reduce the frequency and duration of vasospastic episodes, with consequent prevention of DUs.
Calcium channel blockers
Calcium channel blockers are the first־line pharmacological treatment for patients with RP and SSc, since they have a vasodilatory effect that acts on the vascular smooth muscle. Nifedipine is used at doses of 30-120 mg/day depending on the severity of the symptoms. 23
Prostacyclin analogs
Prostacyclines are synthesized by endothelial cells and mast cells from prostaglandins that act as potent vasodilators. Iloprostol acts by preventing platelet aggregation and formation and as a potent vasodilator; its intravenous use during a crisis is associated with a reduction in the duration of the episode, in addition to a higher cure rate. 24
Phosphodiesterase-5 inhibitors
The drugs included in this pharmacological group act by modulating the cGMP response. Their use has been demonstrated in erectile dysfunction and pulmonary arterial hypertension; in addition, they have proven to be effective in the treatment of patients with severe RP and DUs. Sildenafil has shown benefits in reducing RP symptoms, severity and frequency of acrocyanosis in patients with SSc. 25,26 Other phosphodiesterase-5 inhibitors that have proven to be effective in the management of severe RP are Tadalafil and Vardenafil; however, they require further studies.
Endothelin receptor antagonists
Bosentan, as an inhibitor of endothelin-1 receptors (ET-A, ET-B), is useful for the treatment of idiopathic pulmonary hypertension and associated with SSc; it is also used for DUs. 27 In special situations, combined therapy of endothelin-1 receptor antagonists and phosphodiesterase-5 inhibitors at low doses for the management of severe DUs in SSc has shown promising advances that require further studies in order to be implemented. 28
Other vasodilator agents
Angiotensin-converting enzyme (ACE) inhibitors, such as losartan, and angiotensin II receptor blockers (ARBs) have been used in primary and secondary RP to prevent the final formation of angiotensin II, which acts as a potent vasoconstrictor. Both ACE and ARBs are a clinical option for patients with RP that do not improve or experience side effects triggered by calcium channel blockers. 29
Prazosin, an alpha-adrenergic blocker, has been used in some studies at doses of 1-5mg 3 times a day, showing a decrease in the frequency and severity of vasospasm episodes associated with SSc and RP.
Fluoxetine, a drug belonging to the serotonin reuptake inhibitors group, has also been used for primary and secondary RP, since serotonin acts as a potent vasoconstrictor when found in large concentrations in platelets, thus inhibiting reuptake, which in theory could benefit patients suffering from RP.
Physical therapy
This treatment should be initiated since the onset of the disease and periodically, both as physical and occupational therapy, to avoid complex joint contractures or delay their development. In physical therapy, skin conditioning measures should be taken, such as massages, low frequency current, application of heat and carbon dioxide baths. 30
Surgical treatment
For the surgical treatment of digital lesions associated with SSc, it is necessary to determine the level of immunosuppression in the patient prior to the procedure, carrying out a multidisciplinary approach with rheumatology in order to obtain immunotherapy optimization. In addition, patients should be made aware of associated risks such as delayed healing, increased risk of infection, increased anesthetic risk associated with the possibility of vasospasm in different tissues during the procedure, possible intimal arterial injury and digital ischemia. These factors make patients with SSc a significant challenge for surgical treatment.
Surgical interventions of the hand in patients with SSc are indicated when pharmacological therapy has failed or has not been successful, almost always due to severe vasospasm crisis, recurrent ulcerated lesions and digital pain difficult to handle, leaving digital amputation as the last resort. 31
Some general recommendations to be taken into account during the surgical procedure are wound closure without tension; using Gelpi retractor, atraumatic tissue forceps and sutures moderately; prolonging the time of permanence of the sutures when the normal cicatrization process is delayed; using local anesthesia due to local circulatory advantages; and using tourniquets, if necessary, for no more than two hours. 32
The main surgical management options are chemical or surgical, cervical, thoracic or ultra-selective digital sympathectomy, which can be considered as emergency measures to achieve rapid vasodilation. 14,19,33-35 A predictor ofsuccess in management with sympathectomy is performing a peripheral nerve block with bupivacaine. 36
Performing a preoperative angiography can be helpful to locate arterial obstructions, and also to define the surgical approach and the adequate planning of the procedure to be performed, considering the possibility of doing an arterial bypass, according to the obstruction to blood flow, by grafting the occluded segment to improve blood flow and the DU healing process significantly.
A study performed in 22 patients, with a mean follow-up time of 46 months after periarterial sympathectomy, showed subjective improvement in 18 patients, defined as the improvement of the healing process and decrease in pain and number of DUs. In addition, laser doppler flowmetry was performed, showing a statistically significant increase in skin perfusion after surgery with an average of 31 months during the follow-up. 37
In general, surgical treatment is indicated in symptomatic cases of patients with calcinosis associated with difficult pain or functional limitation. 38 However, resection with curette, scalpel and, in some cases, dental drills may also be performed. The recurrence rate after resection is low in its single form, while the probability of recurrence is higher when there are multiple ulcers and often only allows a reduction in volume. 31 Other carbon dioxide laser therapies by exact ablation of superficial calcifications have been proposed to reduce symptoms and healing time by 410־ weeks without significant tissue damage. 39,40 The severity of calcinosis is not related to the severity of the underlying disease. 32-41
Due to excess tension in the dorsal skin of the proximal interphalangeal joints, wounds, painful ulceration with risk of infection, arthritis, joint dislocation, osteomyelitis and subsequent joint destruction with minimal traumas are likely to be observed.
Digital deformities are frequent in patients with SSc, and the most usual is the proximal interphalangeal joint flexion contractures, followed by hyperextension of the interphalangeal joint (swan neck) and skin and muscle contracture between the thumb and the second metacarpal bone.
Regarding metacarpophalangeal joints, compensatory hyperextension occurs due to a proximal interphalangeal joint flexion contracture, which can be improved with resection arthroplasty and complete removal of the metacarpal head or with prosthetic restoration. 42 Both techniques can improve 30-50° mobility, which is considerably better than the previous manual function. In theory, metacarpophalangeal joints can maintain active flexion but, over time, collateral ligaments, joint capsule and skin can severely limit the flexion of the joint.
Significant contractures in proximal interphalangeal joint flexion may lead to thinning skin and rupture of the extensor mechanism, and also to restrict severely the grip function, which requires surgical management. For this purpose, arthrodesis of the proximal interphalangeal joint flexion contracture has been proposed. Subluxations can also occur frequently, which may require bone shortening by means of osteotomies of the phalanx and arthrodesis to achieve wound closure without tension. Arthrodesis is preferably performed with Kirschner wires to reduce tissue trauma. The optimal flexion degree during arthrodesis of the proximal interphalangeal joint flexion contracture is about 30° for the index finger, increasing to 4555°־ for the little finger. 42
When removing the tourniquet, digital perfusion should be monitored; in case of absence, digital shortening osteotomies or fixation of the joint with greater flexion must be performed to decrease tension in blood vessels. 34
To a lesser extent, cases of hyperextension in proximal interphalangeal joint flexion contracture, secondary to the metacarpophalangeal joint subluxation in flexion and similar to the swan neck in patients with rheumatoid arthritis, may be observed. As patients lose their ability to spread fingers at the metacarpophalangeal joints level, they compensate by hyperextending proximal interphalangeal joints. 43,44
Other less frequent deformity is contracture of the first interdigital space between the thumb and the index finger, which reduces the mobility of the thumb and decreases the patient's ability to grasp large objects. The thumb is often fixed in adduction on the saddle joint and in metacarpophalangeal joint hyperextension. Therefore, trapezius resection may be necessary to restore the abduction capacity of the thumb. The fixation of the interphalangeal joint of the thumb in slight flexion can improve the grip function, also improving opposition in relation to the index or the middle finger. 35
Surgical management of patients with SSc and hand involvement, resection of symptomatic subcutaneous calcifications and digital artery sympathectomy are available as treatment options. In case of contractures, digital arthrodesis, as well as resection arthroplasties or prosthetic replacements, can improve the grip function. 45
Orofacial manifestations of scleroderma
Scleroderma also involves oral and facial tissues with thickening of the skin, thinning lips, deepening of wrinkles and xerostomia. In addition, clinical manifestations such as thinner pointed nose and stiffness or hypomobility of the tongue may occur, causing difficulties in speech and swallowing (Figure 2). 46

Source: Own elaboration based on the data obtained in the study.
Figure 2 Thickening of the skin associated with hypotrophy in cheeks and pronounced bony prominences.
The main oral manifestation is microstomia, which is caused by sclerosis of the perioral tissues; in addition, difficulties may arise regarding social relationships, chewing and oral hygiene. 46
The face is the door to interpersonal relationships, so it is very important to achieve the best possible correction in patients with SSc defects. 47,48 Cutaneous manifestations include linear scleroderma, in particular the en coup de sabre form, and progressive facial hemiatrophy or Parry-Romberg syndrome, which is almost always observed in the face. 49
Linear scleroderma is characterized by a clearly marked depression in the midline of the forehead that can extend to the eyebrow and involve underlying soft tissues, as well as the scalp -in the form of atrophic alopecia plates following a linear pattern-, and the face where cheeks, nose, upper lip and eyes are the most affected areas. 49 If the lesion is narrow, it can be resected and sutured by first intention; if it is broad, there are different reconstructive procedures such as autologous tissue grafting, biomaterials, pedicled flaps and free flaps.
Progressive facial hemiatrophy is characterized by unilateral facial atrophy with involvement of the skin, subcutaneous cellular tissue, fat, muscle and, in some cases, osteocartilaginous structures. In general, it resolves spontaneously and involves especially the dermatomes of one or several branches of the trigeminal nerve. This involvement favors the appearance of ocular alterations such as endophthalmos, uveitis, paralysis of the ocular musculature, ptosis or Horner's syndrome, and of deformations in the jaw with subsequent dental malocclusion, inadequate implantation of the teeth, atrophy of the roots or delay in the appearance of the teeth. This disorder is predominant in women, usually occurs during the first or second decade of life and progresses slowly for 2 to 20 years and then enters into a stationary or plateau phase. 49
One of the most used therapeutic tools to correct these soft tissue deficits is autologous fat graft, which help improve the facial contour. 48,50 To conduct this type of treatment, adequate control of the disease is a must; the anatomical regions from where the fat is extracted include the abdomen, trochanteric areas, flanks, jowls and pubis. 47,50
Adipocytes in these sites are rich in alpha 2 receptors and are sensitive to catecholamines; they also have antilipolytic action. The survival of these cells is better when placed in a rich medium in circulation; the most viable graft goes from a less vascularized area to a more vascularized one, for example, abdomen fat used to fill face blemishes. 47,50
Grafted adipocytes first go through an ischemia phase with infiltration of macrophages, histiocytes and polymorphonuclear cells to clean the remains of tissues. On the fourth day, graft revascularization is initiated by host neoangiogenesis. Revascularization is centripetal and begins in the periphery: the central fat suffers ischemia and is not revascularized, unless the fragments are small. 47,50
Lipografting is an outpatient surgery that offers good results for defects caused by scleroderma with facial hemiatrophy sequelae. It has a low rate of complications and no rejection effect because it is an autologous graft. Due to the characteristics of the adipose cells, 2 to 3 applications are required to obtain a lasting and aesthetically satisfactory result. 51
Hyaluronic acid has been used for soft tissue augmentation with satisfactory results. Its advantages include tolerability, availability, low cost, reversibility, efficiency in volume gain, cosmetic improvement of the deformity and few side effects. Hyaluronic acid is the most common glycosaminoglycan in the skin and, when injected, it promotes growth, softening and hydration through powerful links with water. In addition, this benefit plays an important role in cell growth, membrane receptors function and adhesion. It also stimulates the production of collagen, which could explain why some patients have more long-lasting results. 52
Xerostomia is a common finding that occurs due to fibrosis of the salivary glands and presents as a symptom of dry mouth. It can cause a high rate of periodontal disease, increase the incidence of Candida infections 46 and other manifestations in the jaw and the temporomandibular joint (TMJ) secondary to bone resorption, making itself clinically evident through alterations in the condyle, glenoid cavity and coronoid process. Jaw bone resorption is observed more frequently in patients with diffuse cutaneous SSc and causes marked facial sclerosis and limitation for oral opening. Systematic radiographic screening in different groups of patients with SSc shows incidence of jaw resorption between 20% and 33%. Its multifactorial etiology includes ischemia due to vasospasm, intense vasculitis, compression secondary to perivascular fibrosis and direct stress on the condyle. 46,53
The treatment for xerostomia may be conservative with the use of devices or surgical with joint repositioning through maxillary, mandibular osteotomy and genioplasties. Macintosh et al.53 reported the management of two severe cases of injury at the TMJ level associated with functional consequences such as open bites and malocclusion; in both cases, patients underwent surgery to remove the injured segment and position chondrocostal grafts with satisfactory results and restoration of occlusion with long-term maintenance.
Telangiectasia on the face and oral mucosa is caused by the dilatation of small blood vessels. They can also affect the upper limb and be a source of emotional stress because they generate a perception of disfigurement and dissatisfaction with body image. Traditionally, intense pulsed light therapy (IPL) and pulsed dye laser (PDL) have been implemented improving appearance and tonality. 46,54 PDL is associated with effects on the application site, being transient but with a significant presence of ecchymosis, edema, hypopigmentation and scarring. On the other hand, IPL can be painful and does not prevent recurrence, but it offers similar efficacy with few side effects. The findings suggest that both methods are effective; however the PDL has better results in terms of appearance than IPL. 46,54
Skin ulcers and scleroderma
Ulcers on bony prominences are based on a surrounding avascular tissue of an atrophic nature, which is vulnerable to microtrauma and poor scarring. 55-58
To treat and prevent ulcerations in patients with scleroderma, different alternatives are combined. Therapeutic options include pharmacological treatment, which uses vasodilators such as calcium channel blockers, alpha-adrenergic inhibitors, ACA, ARB II, nitrates, phosphodiesterase-5־ inhibitors and prostacyclines -which have platelet inhibitory properties. 55-59
Additional causes of ulceration of the skin of the limbs include peripheral arterial occlusive disease, venous insufficiency, and rheumatoid arthritis. Up to 10% of leg ulcers occur in association with rheumatoid arthritis. 60 When these conditions occur simultaneously, a combined therapeutic approach that includes pharmacological and surgical techniques is often necessary. 60,61
Away from traditional treatments, cultured keratinocyte grafts appeared in the 1970s as an alternative to vascular, diabetic and post-traumatic ulcers. Based on these initiatives and advances in biotechnology, today, new types of grafts can be found that incorporate semi-synthetic biopolymers originated from hyaluronan benzylic ester and autologous fibroblasts, offering improvements in biointegration. The neoepithelialization capacity of the surface of the bloody area is estimated in 2 weeks on average, while resorption of the biomaterial mediated by macrophages ends in 6 weeks. 62
Adjuvant therapy for the treatment of ulcers
Hematopoietic progenitor cell mobilization for autologous transplantation is a useful therapeutic option in allogeneic or autologous transplantation in diseases linked to the hematopoietic system, and is applicable in cell therapy for chronic occlusive arterial disease, ulcers management and immune system reconditioning. 63
Filgrastim, a human granulocyte-colony stimulating factor (G-CSF), is an endogenous hematopoietic growth factor that stimulates the proliferation and differentiation of neutrophil precursors and increases survival and activity of mature neutrophils, which play a critical role in innate immunity and influence the adaptive immune response. 64,65
In turn, autologous plateletrich plasma (PRP) -which contains components such as fibrin, interleukins, and high concentrations of angiogenic growth factors that support healing- acts as a sealing and excipient medium. In addition to its important anti־inflammatory effect, PRP has been proven to have antimicrobial activity against Escherichia coli, Staphylococcus aureus, Candida albicans and Criptococcus neoformans.66,67
A recent Cochrane meta-analysis showed evidence on the effect of autologous PRP on wound healing. This study included ten randomized clinical trials with 442 participants (mean age 61 years and 42% women), who had multiple causes of chronic ulceration (decubitus ulcers, arterial ulcers, venous and mixed ulcers), and exposed evidence of substantial improvement in healing time, hospital stay, length of treatment and infections. 66
The results achieved with intralesional application of PRP in diabetic foot ulcers coincide with the healing capacity of bone marrow mononuclear cells. 68
Conclusions
SSc almost always affects the integumentary system and is characterized by thickening of the skin and loss of elasticity. In addition, this disease may involve organs such as lungs, heart and gastrointestinal tract with catastrophic repercussions for the patient such as hypertension and pulmonary fibrosis. Etiologically, it is considered a multifactorial disease where the interaction between the environment, genetic predisposition and infections condition its onset. 69-72
This disease occurs in the soft tissues, hands and face. In the hand, the main manifestations are DUs, RP, calcinosis and joint contractures; in the face, microstomia, coup de sabre and progressive facial hemiatrophy; finally, in the soft tissues, chronic ulcers in the lower limbs, which are difficult to manage and have a long evolution. 71-73
Treatment approach to SSc should prioritize pharmacological therapy, while a surgical approach should be considered in severe cases or cases refractory to medication, always bearing in mind possible complications inherent to the pathology such as delayed healing. Patients with RP, calcinosis, facial atrophy or chronic ulcers are susceptible to management by plastic surgery.
This article addressed the consequences of this condition in the skin and soft tissues, which could be handled by plastic surgery. However, other approaches must be taken into account, since there may be other reasons that, if not treated, may lead to death; in this way, SSc should be regarded as a pathology of multidisciplinary approach.