Introducción
Acute abdominal pain (AAP) is a frequent reason for consultation in pediatrics, is difficult to diagnose and constitutes a medical emergency. Semiologically, its onset may be sudden and insidious, and may progress rapidly or intermittently. It is associated with alterations in intestinal motility, oral intolerance and systemic symptoms such as fever.
The causes of AAP may be inflammatory, ischemic or obstructive, and include closed or penetrating abdominal trauma. Clinical diagnosis should be timely to avoid complications that endanger the patient's life, since incarcerated inguinal hernias and testicular and gynecological pathologies are entities that may present similar clinical characteristics of extra abdominal origin.
Clinical case
A 14-year-old adolescent with no relevant history attended the General Medicine Service due to abdominal pain of 20 minutes of evolution, of sudden onset and rapid progress, located in the hypochondrium and right iliac fossa, irradiated to the ipsilateral lumbar area, associated with emesis, diaphoresis and hypotension. Physical examination revealed mucocutaneous pallor, pain and abdominal guarding in right hemiabdomen with positive costovertebral angle tenderness. Initially, medical management was directed to treat possible urolithiasis. Paraclinical examinations showed mild leukocytosis with neutrophilia, while abdominal ultrasound described anechoic free fluid in the right iliac fossa that did not rule out an appendiceal process. Renal etiology was ruled out.
The patient was assessed by pediatric surgery after eight hours due to persistent pain, generalized involuntary guarding and peritoneal irritation. A peptic ulcer was suggested and endoscopy of the upper digestive tract and H2 antihistamine were requested. An emergent surgery was performed considering the clinical deterioration of the patient, signs of shock and generalized peritonitis.
Management
A diagnostic laparoscopy was performed, obtaining the following findings: seropurulent fluid with duodenal and biliary content of 100cc, perforation on the anterior wall of the pyloric region of about 0.8cm in diameter (Figure 1), localized serositis, edema and fibrin. Due to technical difficulties, the procedure was converted to mid-suprainfraumbilical laparotomy, and dieresis by planes until the cavity, revision of the entire duodenum, perforation raffia with absorbable suture (vicryl 3) omentum patch, cavity washing and cleaning, synthesis by planes with absorbable suture (vicryl) 0) and skin with PDS 4.0 were performed without complications.
Source: Own elaboration based on data obtained during the study.
Figure 1 Intraoperative: Perforated duodenal ulcer on the anterior wall of the pyloric region.
Follow-up
The patient was transferred to the intensive care unit with proton pump inhibitor and antibiotics. After five days, intestinal restitution began and discharge was indicated without complications after eight days.
One month after discharge, an endoscopy of the digestive tract with biopsy was performed confirming the presence of Helicobacter pylori. Eradication treatment was indicated according to the guidelines established by the Colombian Society of Gastroenterology.
Discussion
AAP in pediatrics is a syndrome constituted by different pathologies that require timely diagnosis and emergent surgery for proper management. 1,2 This entity occurs between 5-15% of patients aged 5 to 15 years. 3 Clinical diagnosis is not easy to achieve, thus becoming a challenge for general practitioners in emergency services. Clinical manifestations are unclear and diagnostic aids are sometimes inconclusive or unspecific. 4 This situation causes a high percentage of diagnostic errors and masks abdominal surgical processes, as in the case of this patient, who was treated with complete analgesia because the first diagnostic impression was urolithiasis. The way to approach a child or adolescent and their family allows learning about the onset of symptoms and guide the diagnosis; in consequence, developing an adequate clinical history and a good physical examination is highly important. 5
Bearing in mind that surgical abdominal pain may be caused by multiple causes, and that such causes vary according with pediatric age distribution, allows obtaining differential diagnoses to make relevant decisions 6,7 (Table 1).
Table 1 Distribution of AAP causes according to age ranges in pediatrics.
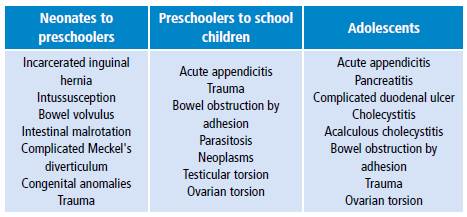
Source: Own elaboration based on Reust & Williams. 9
The most frequent infectious cause in Colombia, according to the Colombian Society of Pediatrics, is acute appendicitis, prevalent in 25 cases per 10 000 school children and adolescents. 8,9 Traumatic causes are considered of great importance due to the increase in the last decades of child abuse and accident rates in the country. 10 In turn, obstructive causes are frequent in toddlers and preschool infants, as well as poor rotation, intussusception, Meckel's diverticulum and bowel volvulus, among others. 11
The initial approach to a patient with acute abdominal pain should begin with a general assessment of the child, including appearance, food intake, diuresis and level of activity, through eye contact or interviewing a relative. Special attention should be paid to abdominal pain history, which should include associated symptoms, previous episodes of abdominal pain, and pain intensity. Some of the clinical manifestations that lead to suspect AAP are absence of bowel sounds, bilious vomiting, involuntary abdominal guarding, rebound tenderness, abdominal rigidity and fever, when it appears after the onset of abdominal pain and emesis. Acute chronic intermittent abdominal pain is less likely to be related to a surgical cause than to a first episode of acute pain. 9
Duodenal peptic ulcer (DPU) is relatively rare in pediatrics. In Colombia, an incidence rate of 4.4 per 10 000 children has been reported. 12 It is classified into primary and secondary; primary ulcers present along with infection by H. pylori, bacteria related to socioeconomic conditions and found in 2/3 of the world population, in 80% of the adults of developing countries. 13,14 In Japan, a 20-year follow-up study was conducted with a sample of 52 patients, of whom 90% were adolescents with acute abdominal pain, predominantly male, with family risk factors for DPU such as smoking, alcohol consumption, use of chronic drugs, and in all cases H. pylori infection was identified as the main cause. 15
Secondary ulcers are related to causes such as burns, exogenous drugs (NSAIDs or steroids), stress, hypergastrinemia, causes of central origin due to trauma or neoplasms, low weight and prematurity in neonates, and gastrin hypersecretion of parietal cells due to maternal or spontaneous influence. The latter has been reported in isolation in these age ranges. 16,17
It should be borne in mind that other ulcers may be silent until they manifest as a perforation with shock in patients with acute abdomen, since laparotomy is the only diagnosis method of this disease, as in the case presented here. 18,19
Conclusions
Complicated duodenal peptic ulcer should be considered in differential diagnoses of acute surgical abdomen in children and adolescents. In Colombia, a developing country with a high rate of H. pylori infection, its existence is well documented except for pediatrics. For this reason, it is important to promote prevalence studies in the Colombian population that allow developing eradication protocols to avoid complications.














