Introduction
The gynecological surgery service is responsible for surgical procedures in the female genital tract. It also treats breasts and pelvis and carries out procedures related to the uterus, its appendages and correction of urinary incontinence. 1 The most common gynecological procedure is hysterectomy, with an incidence in the USA of 510 per 100 000 inhabitants reported in 2004, in Denmark of 173 per 100 000 inhabitants in 2011 2, and in Brazil of about 300 000 per year. 3 Other gynecological procedures include tubal ligation, curettage, cystectomy and salpingectomy. 1,4
All surgical procedures may have complications; indications of unsafe care derived from medical care include complications, adverse events and incidents. A complication is any undesirable and involuntary outcome derived from the surgery that affects the patient, which would not have occurred if the surgery had been performed following the corresponding procedures. 5-7 An adverse event is an injury or unintentional damage caused by the intervention and not by the pathology. 5-7 Finally, an incident is defined as an event or circumstance that could have caused or caused unnecessary harm and may originate from unintentional or involuntary acts. 5-7 Surgical complications are considered a relevant issue from a clinical, legal and public health point of view due to the cost they generate to the health system.
Expenses related to health care have been increasing around the world. In 2007, the total hospital care expenditure in the USA was estimated at 696.5 million dollars, which corresponds to 31% of total health cost. In 2013, these costs in Switzerland were 69 million dollars, of which 28% were allocated to surgical departments. This situation is similar in most European countries. 8,9
Surgical complications are, in part, responsible for this increase. The average hospital cost for all patients without complications is USD 27 496, but when there is at least one surgical complication of any severity, the amount increases to USD 62 392. 10 The cost of complications depends on their classification. Volanthen et al.10 report that, according to the Clavien-Dindo classification -the most widely accepted-, a grade I complication generates a cost of USD 2 793 and a grade IV, a cost of above USD 130 000. Complications classified as grade IIIb or higher lead to a significant increase in care costs compared to procedures without post-operative complications. 10
The prevalence of surgical complications in gynecological surgery varies depending on the population. After reviewing 22 214 gynecological procedures, the American College of Surgeons found 3.7% complications 11; Brazil reports a higher percentage with 8.9% 1, while Colombia reports 12.5%. 4 Many studies focus on the rate of complications related to hysterectomy because it is the most frequent gynecological surgical procedure.
In 5 279 procedures, Brummer et al.12 reported a higher complication rate related to laparoscopic, abdominal and vaginal hysterectomy of 4.3%, 4.0% and 2.3%, respectively, and an overall complication rate of 15.4%, 19.2% and 11.7%, respectively. In turn, McPherson et al.13 reported a frequency of severe complications of 3% in 37 512 women. However, the results of research on surgical complications vary widely and depend on the type of route used; thus, regarding laparoscopic hysterectomy, other investigations report global complication rates ranging between 0.2% and 10.3%. 14 These non-homogeneous reports were corroborated in another study. 15
In a series of 3 190 women undergoing hysterectomy through different routes, Donnez et al.15 reported a prevalence of complications for laparoscopic subtotal hysterectomy of 1.36% (CI95%: 0-3.15) and for total hysterectomy of 1.59% (CI95%: 0.013.1), which was statistically similar to the values of vaginal and abdominal procedures found in this research with 1.10% (CI95%: 0.013-1.2) and 1.22% (CI95%: 0.16-2.3), respectively.
Sociodemographic conditions, comorbidities, medical history, indications of the procedure, equipment and experience of the surgeon are characteristics that also affect the outcome of the surgery. 11 The risk increases with the complexity of the surgical procedure and the experience of the surgeon, hence the accumulation of surgical experience with the help of preventive maneuvers is useful to significantly reduce the rate of complications. 16
Martino et al.17 reported that patients undergoing robotic-assisted laparoscopic hysterectomy have a significantly lower probability of re-admission when compared to laparoscopic, abdominal and vaginal hysterectomy; furthermore, the robotic technique has a lower rate of hospital stay and generates less bleeding, as well as cost savings due to re-admission.
Regarding the socioeconomic situation, women with scarce resources and unemployed have a much higher probability of complications after hysterectomy when compared with employed women (OR: 1.20, CI95%: 1.06-1.36), which is similar for women with low educational attainment (OR: 1.18, CI95%: 1.05-1.33). These differences may be explained, in part, by an unhealthy lifestyle and the presence of comorbidities in women of low socioeconomic status. 18,19
Individual characteristics such as age, comorbidities, functional status and unintentional weight loss are also related to complications. 20 Barbosa & Garnica 4 found diabetes mellitus (OR: 75.5, CI95%: 4.84-117), chronic anticoagulation (OR: 24, CI95%: 2.73-214.59) and myomatosis (OR: 35.1, CI95%: 3.85-298.87) as associated factors. Likewise, Erekson et al.11 reported an age of >80 years (OR: 1.91, CI95%: 1.22-3.00), malignant disease (OR: 2.98, CI95%: 1.77-5.01) and obesity (OR: 1.95, CI95%: 1.57- 2.41) as influential factors for complications.
Some of the complications associated with gynecological surgery are urinary tract injury (0.3-1%), bowel injury (0.4%), ureteral injury (0.25%), fever (0.47%), bleeding (0.06%) and rectal perforation with very low frequencies (0.09%). 4,15 The most common complication is surgical site infections, which occur between 2.2% and 10% 1,4,21,22, followed by transfusion (4%), pelvic abscesses (1.5%), reoperation (2 %) and wound dehiscence (1.5%). 4,22
The topic of surgical complications is widely studied worldwide, but this is not the case locally; in Colombia, limited research hinders its efficient assessment. Consequently, in addition to its clinical relevance, the costs to the health system and the legal implications of surgical complications, this research was proposed to determine the prevalence of surgical complications of gynecological surgery at the Hospital Universitario San José of Popayán (HUSJ), Colombia, in 2015 and explore possible associated factors.
Materials and methods
This was a cross-sectional study in which the clinical records of patients who undwent gynecological surgery at the Hospital Universitario San José (HUSJ) between January and December 2015 were included.
The HUSJ is an institution that provides tertiary care services, and is a reference center of the department of Cauca, located in southwestern Colombia, which treats population enrolled in the contributory insurance scheme, as well as patients subsidized by the State through the social security system.
All clinical records of patients undergoing scheduled gynecological surgical procedures were included in the research, and patients who presented incomplete data in more than 10% of the variables analyzed, were pregnant or underwent emergency procedures were excluded. Outcome variables include a surgical complication reported within 30 days after the procedure, which was defined as any undesirable, involuntary outcome that results from surgery, affects the patient and would not have occurred if the surgery would have been performed following the established procedures. 5-7
Complications were obtained from institutional records, both from the outpatient clinic and the emergency department. The presence of a complication was reported according to the program for improvement of institutional quality. The members of this program were in charge of analyzing the possible complications and defined whether the analyzed case was a complication or not. The different types of complications were also considered and were classified according to the literature as major (reoperation, bladder injury, nosocomial urinary infection, transfusion, bleeding, postoperative ileus) or minor (surgical site infections, hematoma, wound hemorrhage and wound dehiscence). 11,15
It should be noted that the protocols for antibiotic prophylaxis and antithrombotic prophylaxis in all surgical procedures were the same and followed the institutional guidelines. On the other hand, and in compliance with the safe surgery institutional program, at the time of discharge, both the patient and the family were informed in writing about the post-surgical follow-up that must be performed in the institution by external consultation and on warning signs that, if necessary, should lead the patient to visit the emergency gynecology service of the HUSJ. The whole universe of patients was considered for the sample size in the period under study.
Process
Once the institutional ethical approval was obtained through Minutes 6 issued on May 13 2016 by the HUSJ ethics committee, a first filter was applied: searching for all surgical procedures performed in the institutional databases. Then, a second filter allowed identifying all the scheduled gynecological procedures; once this was done, the medical records that met the inclusion criteria were analyzed and the information was collected by means of a semi-structured instrument designed by the researchers, reviewed by experts and adjusted through a pilot test.
Variables
Clinical, biological and sociodemographic variables were collected including age, origin (urban, rural), marital status (stable, not stable), gynecological and obstetric history, presence and type of comorbidities (obesity, diabetes mellitus, smoking, hypothyroidism, adherence syndrome and the remaining were classified as other) 11,15, type of surgical procedure and indication thereof, surgical time (> or <3 hours), surgical route (laparoscopic, abdominal or vaginal) and type of pathology (malignant or benign).
Statistical analysis
To determine the prevalence of surgical complications, the total number of surgical complications found in women undergoing gynecological surgical procedures was taken as the numerator, and the total number of records reviewed as the denominator. The variables were analyzed individually and from an exploratory point of view to verify the normality of their distribution and identify extreme and lost values that could affect the result. Student's t-test was used for continuous variables with normal distribution, after analyzing the variance, and Mann-Whitney U for non-normal distribution variables, following the Shapiro-Wilk normality test and chi-square or Fisher's, as appropriate. To explore the factors possibly associated with surgical complications, a bivariate analysis was performed, where the OR with its respective CI95% was used as a measure of association between the different variables, thus generating a contingency table. Records with complications reports were taken as a case and those that do not have this report as controls. For this analysis, age was categorized in <39 years (reference category), from 40 to 49, and >50 years. The study was endorsed by the HUSJ Ethics Committee (approval act number 6) and the analysis was carried out using the Stata 10.0 program.
Results
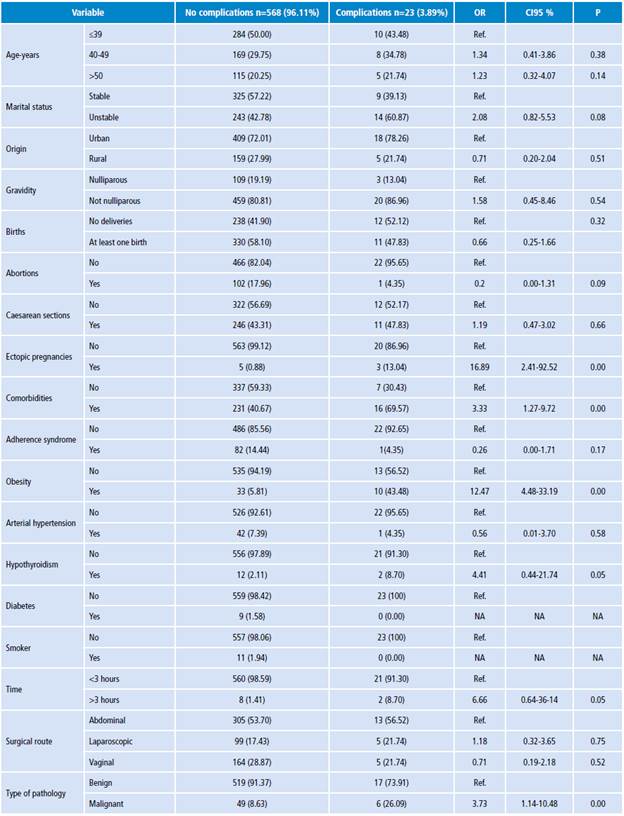
During 2015, 593 scheduled gynecological surgical procedures were performed in the HUSJ, of which two were excluded due to incomplete data, so 591 were included in the final analysis. The average age of the population under study was 39.99 years with a standard deviation of 12.17 years; 72.25% came from urban areas, 81.05% had at least one birth, 43.49% had a cesarean section and 1.35% had a history of surgical management due to ectopic pregnancy.
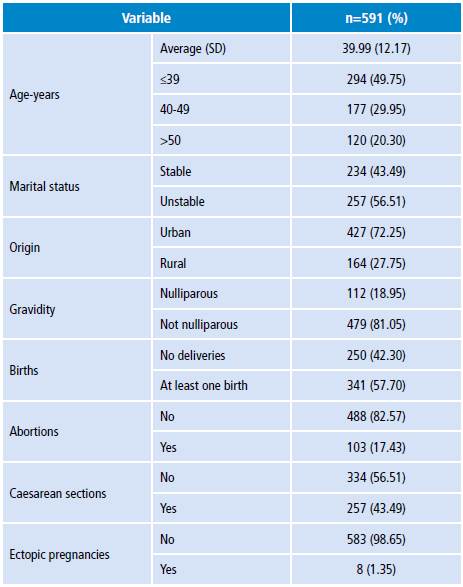
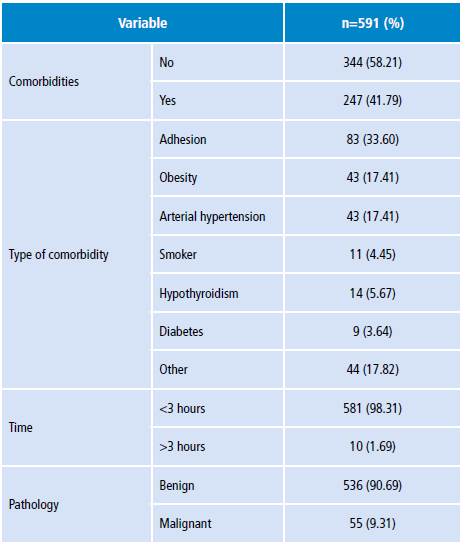
Regarding comorbidities, 58% presented at least one of them, the most frequent being adherent syndrome (33.6%), obesity and high blood pressure (17.4%). The most frequent surgical procedure was Pomeroy tubal ligation (29.10%), followed by hysterectomy (22.34%) and curettage (15.74%). Regarding the indication of the procedure, having enough children was the most frequent (29.10%), followed by abnormal uterine bleeding (13.37%), complex adnexal mass (12.86%) and myomatosis (10.83%). 98.31% of the surgical procedures lasted less than 3 hours. The most used surgical route was the abdominal with 53.81%, followed by vaginal and laparoscopic with 28.60 and 17.60, respectively. Benign pathology was the most frequent (90.69%) (Tables 1, 2 and 3).
Table 1 General characteristics of the study population with gynecological surgery complications at the Hospital Universitario San José of Popayán, Colombia. 2015.
SD: standard deviation.
Source: Own elaboration.
Table 2 Comorbidities, surgical time and type of pathology found in the Hospital Universitario San José of Popayán, Colombia. 2015.
Source: Own elaboration.
Table 3 Type, indication and route of the procedure conducted at the Hospital Universitario San José of Popayán, Colombia. 2015.
AUB: abnormal uterine bleeding.
Source: Own elaboration.
With respect to the main objective, it was found that the prevalence of complications was 3.8% (95% CI: 2.3-5.4); after classifying them, major complications pralence was 1.8% (CI95%: 0.76-2.9), while for minor complications it was 2% (CI95%: 0.8-3.1). Major complications included reoperation (0.51%), bladder injury (0.34%) and nosocomial urinary tract infection (0.34%), while minor complications were infection of the operative site (1.52%), hematoma (0.17%), wound hemorrhage (0.17) and wound dehiscence (0.17%) (Table 4). It should be noted that there were no deaths during the period studied.
Table 4 Type of gynecological surgery complications in the Hospital Universitario San José of Popayán, Colombia. 2015.
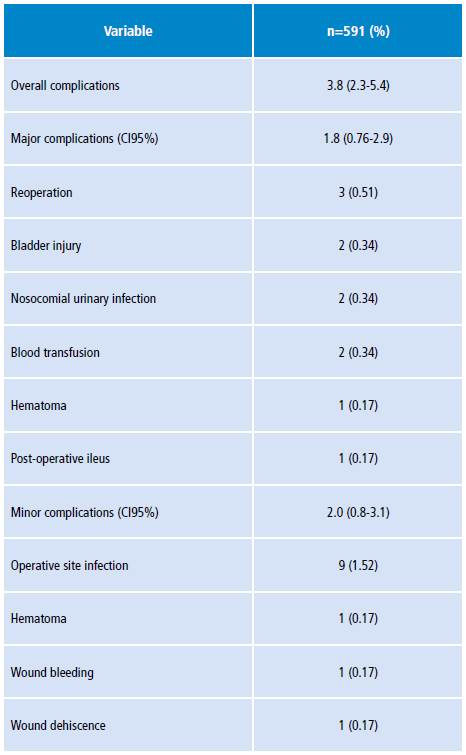
Source: Own elaboration.
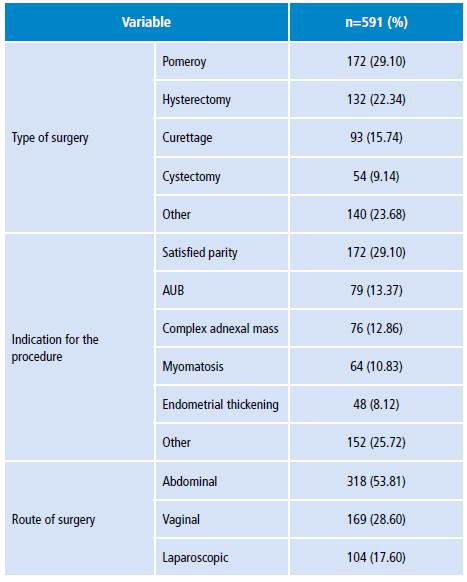
The bivariate analysis showed that having a history of surgical management of ectopic pregnancy was positively associated with complications (OR: 16.89, CI95%: 2.41-92.52); the same happened with having at least one comorbidity (OR: 3.33, CI95%: 1.27-9.72), of which only obesity had statistical significance (OR: 12.47, CI95%: 4.48-33.19). It was also found that malignant pathology was positively associated with complications (OR: 3.73, CI95%: 1.14-10.48), but with respect to surgery routes, no statistical significance was found for laparoscopic route (OR: 1.18, CI95%: 0.32-3.65) and vaginal route (OR: 0.71, CI95%: 0.19-2.18). The other variables analyzed did not show statistical significance (Table 5).
Discussion
The final analysis was carried out in 591 clinical records, finding a general complications prevalence of 3.8%, a figure that coincides with that described by Erekson et al.11, who report 3.7%, but which contrasts with the figures of Coelho et al.1 and Barbosa & Garnica 4, who report 12.5% and 8.9%, respectively. This figure also differs from Putz et al.9, who report 2.8% for laparoscopy. These differences can be explained by the fact that only scheduled surgeries were considered in this study, and it was assumed that the patients would be in better shape, which does not happen with patients undergoing an emergency procedure, as they have greater probability of complications. Another explanation for this difference in prevalence could be that the most frequent type of procedure found in this study, which is Pomeroy tubal ligation (29.10%), is less complex and therefore less likely to lead to complications. 16
Regarding the major and minor complication classification, a 1.8% and 2% prevalence, respectively, was found for each case, which differs from the figures reported by Barbosa & Garnica 4, where the values were 7.5% and 12%, respectively. Regarding the type of complications, bladder injury was one of the most studied due to its frequency, anatomical relationship and clinical relevance.
It is estimated that injuries in the genitourinary tract (bladder and ureter) occur between 1-2% of all major gynecological surgeries 23. The present study found a frequency of 0.34%, which agrees with Lee et al.24, who report 0.28%; slightly higher figures are reported by Valle et al.25 with 0.5%, and Teeluckdharry et al.26 with 0.8-1%. Likewise, Vakili et al.27 and Ibeanu et al.28 report a frequency of 3.6% and 2.9%, respectively, for this same type of injury in patients undergoing hysterectomy, figures higher than those found here and that could be explained due to the fact that hysterectomy represented 22.34% of the total procedures included in this study and because this is a more complex procedure, and therefore it has a higher risk of complications.
The most frequent major complication was reoperation (0.51%), but this figure is still lower than that reported by Barbosa & Garnica (2%) 4 and by Valle et al. (1.3-1.6%). 25 With regard to minor complications, surgical site infection was the most frequent with 1.52%; Coelho et al.1 and Barbosa & Garnica 4 also report this complication as the most frequent, but with figures higher than those described here: 4.5% and 2.2%, respectively. 1,4
Regarding possible associated factors, no significance was found in the socioeconomic stratum, unlike Daugbjerg et al.19, who reported that this factor was significant (OR: 1.20, CI95%: 1.061.36). With regard to obstetric history, a relationship was found between surgical complications and history of ectopic pregnancy with surgical management (OR: 16.89), but no studies were found for this specific variable; however, taking into account that this is an abdominal surgical procedure, the studies by Barbosa & Garnica 4 and Brummer et al.12 did not find any difference with respect to a history of previous abdominal surgery.
Unlike Brummer's study, which reports that bladder injury was associated with cesarean section history (OR: 4.01, CI95%: 2.06-7.83) 12, this research did not find any association. In relation to individual characteristics, it was found that the presence of at least one comorbidity (OR: 3.33) was associated with complications. Specifically, in the present study, obesity had an OR: 12.47 for a body mass index (BMI) >30kg/m2; for this same BMI, Erekson et al.11 reported an OR: 1.77 (CI95%: 1.45-2.17), which is lower but significant. On the other hand, Olsen et al.29 reported an OR: 3.0 (CI95%: 1.0-9.6) for BMI=30-35 kg/m2 and an OR: 5.7 (CI95%: 2.1-15.6) for BMI >35 kg/m2. 29 Unlike other studies, other comorbidities were not significant. 4,11
In relation to malignant disease, a significant association was found, coinciding with Erekson et al.11 for gynecological cancer (OR: 1.60, CI95%: 1.27-2.0) and for dissemination (OR 2.57; CI95%: 1.64-4.03). 11 Age and surgical time reported in this study were not significant, but Brummer et al.12 found a negative association for women >55 years who underwent vaginal hysterectomies (OR: 0. 45. CI95%: 0.30-0.68), while Erekson et al.11 reported an OR: 1.8 (CI95%: 1.25-2.58) for women >80 years. In this study, surgical time was associated with complications, contrary to Erekson et al.11 (OR: 2.91; CI95%: 2.18-3.89). No statistical difference was found regarding the route used for surgery, contrary to the study by McPherson et al.13, where laparoscopic surgery presented an OR: 1.9 (CI95%: 1.5-2.5) when compared with abdominal surgery.
The strengths of this research include a good sample size, little loss of data and a definition of standardized complication provided by a multidisciplinary team of the program for improvement of institutional quality. In addition, the institutional guidelines for antibiotic prophylaxis and thrombosis prophylaxis were met. There is also a low probability of underreporting, since complications were extracted from institutional records of both external consultation and emergency services, a process that was facilitated by compliance with the patient follow-up program. One of the weaknesses of this study is that it did not consider the history of previous abdominal surgery -hence this variable could not be analyzed-, as well as time of discharge, days of re-admission and type of anesthesia. Another possible weakness is that surgeries such as tubal ligation or curettage have a lower risk of complications than surgeries such as abdominal or vaginal hysterectomy; this may generate a lower overall prevalence, although the objective of the present study was to determine the prevalence of surgical complications related to gynecological surgery.
Conclusions
A low prevalence of complications was found, which is similar to the results reported in most studies. Some of the possible associated factors include history of surgical management of ectopic pregnancy, obesity and gynecological surgery due to malignant pathology. New studies regarding this topic are suggested to find out the actual situation of these procedures and their associated factors and, in the same way, expose care costs according to the type of classification of the complication.