Introduction
There is a heated debate on the efficiency and effectiveness of using aggressive treatments for achieving health outcomes at the end of life. On the one hand, there is clinical evidence of cost-effective treatments that add years of life. 1 On the other hand, some state that the intensity of treatments provided in the last months of life can be considered as an indicator of the propensity health professionals have to use highly expensive technologies. 2 For example, it has been reported that in USA the use of intensive care units by Medicare beneficiaries experienced a dramatic increase in the last decade, rising from 24.3% in 2000 to 29.2% in 2009. 2 Likewise, in the USA higher health spending levels in the last six months of life is not correlated with higher survival rates in patients who have suffered heart attacks, cardiac arrest, or gastrointestinal bleeding. 3
The interaction between physicians' beliefs and patients' preferences have also been questioned in the available literature. In this sense, Cutler et al.4 reported that 36% of health care spending at the end of life and 17 % of total health expenditures in the USA are associated with physicians' beliefs unsupported by clinical evidence. 4 In this regard, Meier 5, in a case study, describes the existing tension between a palliative care physician who is helping a cancer patient coping with her coming death and her oncologist, who opposes to the idea of quitting the treatment. 5 Similarly, in another study, Meier 6 argues that overtreatment in patients near their death is a major cause of low-value care. 6
In recent years, several studies focusing on quantifying payments made by third party payers for the provision of health care to patients in their end of life phase have been published in order to illustrate this debate, in particular those made by Medicare in the USA. Some of these studies indicate that payments made by Medicare for the provision of care to patients in their last year of life (LYOL) account for 25% of its total expenditure involving the provision of health care to the elderly (aged 65 or older). 7-9 Somehow, studies addressing this topic in other developed countries are scarce 10-12, and nonexistent in Latin-American countries.
The purpose of this study is to estimate the proportion of payments made in health plans for the provision of health care to people in their LYOL in Colombia by using data on health expenditures from two health plans in the elderly and other age groups.
This is a topic of great importance for Colombian policymakers for at least two reasons. First, Colombia is a middle income country in which the proportion of people aged 65 or older is rapidly increasing. According to population projections made by the Colombian government, by 2020, 8.5% of the total population will be ages 65 or older, which almost doubles the 4.4% reported in 1985. Likewise, in terms of gender, by 2020, 9.4% of all women and 7.6% of all men in Colombia will be part of the elderly population (aged 65 or older). 13 In addition, according to the 2015 Colombian National Survey on Health, Wellness and Aging, 28% of the elderly need help in their activities of daily living (ADLs), including eating, taking a shower, or walking, while 2% are bedridden. 14 These data suggest that disability and chronic illness prevalence in the elderly in Colombian is increasing, and that both conditions are correlated. Besides, higher rates of hospitalization of elderly population and elder abandonment represent higher healthcare spending for the Colombian health system, which is worsened by the lack of trained caregivers for this population. 14.
The second reason is that in 2009 the Colombian health system was declared in a social emergency state by the Colombian government 15 due to a serious financial crisis that has not yet been resolved.
Although the present study addresses this issue in Colombia, its results cannot be used to characterize the general situation in the country for several reasons. First, people enrolled in the health plans analyzed here are employees or self-employed individuals who can afford being in the health care contributory regime, as opposed to those who are in the subsidized regime. Second, there are 12 health care plans in which Colombian employees can be enrolled, but the data analyzed here were obtained from only two of these health plans. Third, health plans in Colombia are free to structure their own provider networks and health care models, and therefore they are able to set certain limits to physicians and organizations that tend to overtreat patients.
Materials and methods
Medical costs were allocated in terms of survivors and decedents. 8 The reference period was from 2011 to 2013. Total health expenditure per year, which was used to estimate LYOL health costs, was distributed between survivors and decedents according the following rules:
Health costs associated with individuals whose status was reported as alive on the 31st day of December of the year in which the expenditure took place were assigned to the survivors group.
Health costs associated with any individual whose dead was reported in any day of the year in which health spending occurred were assigned to the decedents group.
Health costs associated with patients that were alive in the year in which health care provision payments were made, but then died during the following year, were assigned to both groups by using the difference between the date of death and the date of the health service provision. For example, when a person died on June 30th of the year following the year in which health spending happened, health care costs between January 1st and June 30th were assigned to the survivors group, while health expenditure between July 1 st and December 31st was assigned to the decedents group. Per capita payments were estimated by dividing total cost for decedents or survivors by the total number of person-days for decedents or survivors.
Data from 2011 to 2013 were used in this study. The following fields were available in each claim: location (department and municipality), ICD-10 diagnosis code, date of service, service code (CUPS, for its acronym in Spanish), type of service (outpatient, diagnostics, inpatient, emergency), type of payment made to the provider by the health plan (i.e., capitation, fee-for-service), units of services provided, payment amount, copayment amount, type of service (procedures or medicines) and service provider code. The following information of all members enrolled in both health plans was available: encrypted unique identifier, sex, date of birth. The date of death of individuals who died in 2011, 2012, and 2013 was also available. Costs were calculated in Colombian pesos (COP), but these amounts are presented in tables in USD currency using an average exchange rate of 1 838 COP/USD so that international comparisons are easier to make.
Results
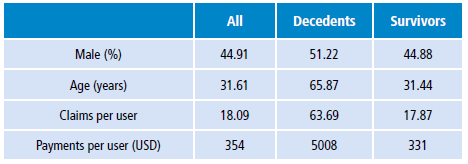
Descriptive statistics of the analysis period are shown in Table 1. A higher death rate was observed in men, and approximately 65% of them died aged 65 or older. Concerning the average number of claims, the following values were found: 18 claims per user, 63 claims per decedent, and 17 per survivor. Finally, on average a survivor represented an average spending of USD 331, while a decedent, an average of USD 5.008.
LYOL average health spending by age group and sex based on pooled data from 2011 to 2013 is shown in Table 2. If all age groups are considered, LYOL health spending accounts for 6.25% of total spending. Average health costs associated with users who died were 15.11 times higher than those associated with survivors. Regarding age groups, the highest proportion of LYOL health spending was observed in those aged 65 or older (17.93%), followed by those in the 60 to 64 ages range (9.18%), which can be explained by the high risk of dying these age groups have.
Table 2 Average 2011-2013 expenditure by sex and age (US dollars).
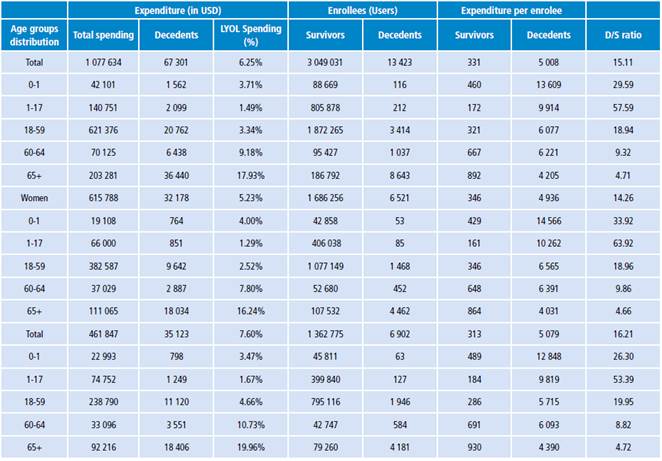
D/S: Decedent/Survivor.
Source: Own elaboration.
Finally, LYOL health spending in members aged 65 or older based on gender is as follows: 16.2% in women and 20% in men; in addition, in this age group, health care costs associated with decedents were on average 4.7 times higher than those reported for survivors.
Discussion
LYOL health spending represents around 25% of total Medicare expenditure in the USA. 8 In addition, several authors argue that a part of this expenditure cannot be supported by clinical evidence and does not provide a better quality of life for terminally ill patients. 2-4,6.
To the best knowledge of the author of the present study, currently there are no studies addressing LYOL health care costs in any Latin American country, so this is the first one providing LYOL health spending estimations in Colombia based on the data of more than 3.7 million users enrolled in two different health plans and living in some of the most populated urban areas of the country (Bogotá, Medellin, Cali). According to the results reported here, LYOL health spending in Colombia regardless of age (6.25%) is higher than what other studies have reported for countries like South Africa (5.4%) 12 and the Netherlands (5%). 10,11 Regarding LYOL health care costs in people aged 65 or over, it accounted for a 17.9% of the total expenditure for the provision of health care to this population, which is significantly lower than the percentage reported by some authors for Medicare beneficiaries aged 65 or older in the USA. 7-9
Results reported here are of great importance in Colombia, since this study addresses a rarely discussed topic in the literature, in particular in Latin America. Somehow these results are limited, as the data used in this study comprise near 3.7 million users, out of approximately 20 million, of the Colombian health system contributory regime, who were enrolled in two health plans, so they can't be extrapolated to all users of the contributory regime, or those enrolled in the subsidized regime. Also, there is risk selection from health plans trying to avoid very ill patients, and, adverse selection from very ill patients to try to enroll in health plans that have better health care models.
Conclusions
The fact that a higher amount of money is spent in the provision of care to patients in their LYOL is not surprising at all, but it raises the question of whether there are more efficient and more humane ways to provide care at the end of life period. Health systems financial stability in developing countries is very weak, as there are other sectors in which already scarce financial public resources are also required. Findings reported here suggest the necessity to start discussing the role of palliative care in developing countries, including home care and advanced directives. Likewise, based on the findings described here, health insurers should focus on the prevention and early detection of disability in the elderly, as well as on the implementation of alternative ways to provide patients in their LYOL with a better quality of life. For example, in the USA, Medicare program allows all terminally ill patients (with a six months of life prognosis) to decide whether they want to quit curative care and rather being give home care based treatments focusing on being comfortable in the final moments of their life by means of services that include physical, emotional, social, and spiritual care for both, patients and their relatives, or not.