Introduction
According to the World Health Organization, sedentary lifestyle is one of the leading risk factors for developing noncommunicable diseases. It is presumed to be the fourth leading cause of death, accounting for 6% of deaths worldwide, and is also considered as a leading cause of 21-25% of breast and colon cancers, 27% of diabetes cases and 30% of the burden of ischemic heart disease. Furthermore, estimates are that 60% of the world's population is not physically active (PA), which is a major public health problem for the general population. 1
In university students from Colombia, high values of sedentarism, ranging from 57% to 82%, have been reported 2,3; these values coincide with other reports around the world and even exceed the average. In this regard, Prieto-Rodríguez 4 observed that the level of sedentary lifestyle was close to 83% at Universidad Nacional de Colombia, Bogotá Campus, students. However, the study by Rodríguez et al.5 established that about 70% of the evaluated students did not perform the recommended PA level, a figure that is significantly inferior; nevertheless, levels of inactivity are alarming.
That said, it has been observed that a sedentary lifestyle has a negative impact on lung function and maximal oxygen consumption (VO2max); likewise, an average decrease of VO2max of 0.26 mL/min/ kg per year and of 0.23 mL/min/kg per year in men and women, respectively, has been described 6, which represents ~7% less in comparison with physically active subjects. 7 On the other hand, significant reductions have been reported (p<0.05) in relation to respiratory muscle strength (RMS), volume and lung capacity as representatives of the functionality of the respiratory system, leading to an alteration of the ability to generate pressure mediated by the modification of the relationship between length and contraction velocity; the former depends on the change of amplitude, which causes lower total lung capacity (TLC), while the latter relates to muscle fatigue during effort, which represents a decrease in pulmonary function and low tolerance to physical activity. 8
In response to alterations in respiratory muscle and VO2max decrease caused by a sedentary lifestyle, a hypothesis has proposed that the application of respiratory muscle training (RMT) improves RMS parameters, lung function and VO2max. However, the use of this methodology in this population has not been widely described; on the contrary, it has been studied in clinical and sports settings in order to improve health condition and physical performance, finding significant changes in muscle strength (-10-55°%) 9,10 and VO2max (~1-4 mL/kg/min in patients). 11 These results correlate with possible adaptive changes, including an increase in the percentage of Type I fatigue-resistant fibers and an increase in the size of Type II fibers in respiratory muscles. 12 Therefore, the aim of this study is to determine the effect of an RMT program on RMS, lung function and resting oxygen consumption in sedentary subjects. 5,13-16
Materials and methods
Type of study
This is a prospective, longitudinal, experimental study with pre and post-intervention measurements.
Participants
Students attending the Universidad Nacional de Colombia were included; they were aged between 15 and 35 years, sedentary and with a PA level <150 minutes per week, presenting associated risk factors such as overweight, unbalanced diet and consumption of alcohol and tobacco. Subjects who reported any type of previously diagnosed neurological, osteomuscular, metabolic or cardiopulmonary pathology and respiratory trauma that compromised the integrity of the rib cage were excluded. Subjects with a high or moderate level of PA according to the International Physical Activity Questionnaire (IPAQ), short version, were also excluded. The sample was probabilistic and the software G Power 3.1.9.2 for Windows was used (d=0.9; statistical power 1-β=0.99; probabilistic error a=0.05), n=21+4 (10% expected follow-up losses). 17,18
Anthropometric variables and physical activity level
Sociodemographic variables were recorded and the short IPAQ and the FANTASTIC questionnaire were applied to measure PA level and lifestyles, respectively. If the interview met the criteria of the study, anthropometric characteristics were measured according to the International Standards for Anthropometric Assessment (ISAK). The measurements were taken between 08:00 a.m. and 4:00 p.m. in a comfortable place at the right temperature. A stadiometer was used to measure height (20-205cm, 1mm precision), body weight was measured with a digital scale (Kenwell®, 100g precision) and body mass index (BMI) was determined by using the Quetelet index. The measurements were taken twice and the average score was recorded for statistical analysis.
Respiratory muscle strength
RMS was determined by measuring maximal inspiratory pressure (MIP) and maximal expiratory pressure (MEP) using a Dwyer Series 477 meter (±300mmHg), and following the American Thoracic Society/European Respiratory Society (ATS/ERS) protocol and what has been previously described by other authors. 5,8,19,20 Participants started the test in a seated position without further support and were instructed to exhale in a controlled manner as much air as possible to obtain inspiration from the residual volume (RV); then, they were instructed to put on a mouthpiece and nose clip and to take vigorous air through the mouth during the circuit. For the MEP, participants took in the largest amount of air in a controlled manner until they reached TLC and then exhaled vigorously through the meter. Three measurements were taken for MIP and three for MEP, spaced by 1-minute rest periods; the highest value obtained was recorded.
Oxygen consumption
Energy expenditure, VO2 and carbon dioxide (CO2) production at rest were measured by means of indirect calorimetry using the Vmax Encore 29C® calorimeter (Calorimetry Laboratory of the Department of Human Nutrition of the Faculty of Medicine of the Universidad Nacional de Colombia). The subjects, in a seated position, were coupled to the flow sensor using a MicroGardR® disposable filter, a conventional FreeFlow™ mouthpiece and a nasal clip, and then breathed normally through the mouth avoiding inspirations or forced exhalations and changes of position for a period of 20 minutes, during which the system recorded the variables mentioned in real time. In order to avoid alterations during the measurement, participants were not allowed to see the recording monitor, so that they could not control the respiratory rate or volume per minute at any time. 21
Pulmonary function tests
After the previous procedure was done, participants rested for 5 minutes and continued with lung function measurements, including forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1) and FEV1/FVC ratio, which were recorded using the same equipment (Vmax® Encore PFT system). Forced spirometry was performed following the ATS/ERS parameters described by Miller et al.22 Three phases were considered during the maneuver carried out with the closed-circuit method: maximal inspiration, "forced" exhalation and continuation of exhalation until the end of the test.
Maneuver, posture, inhalation, placement of mouthpiece and nose clip and exhalation were instructed and demonstrated; participants were coupled to the circuit where they performed maximal inspiration with a pause of less than one second of TLC (phase 1), followed by exhalation until reaching the RV (phases 2 and 3).
During the whole process, participants were encouraged and the flow/volume curve was monitored in order to guarantee an ideal layout. An acceptable maneuver was required to meet the following criteria: 1) recording a satisfactory expiration; 2) not coughing, especially in the first second; 3) avoiding Valsalva maneuvers that could interrupt air flow; 4) preventing air leaks or losses; 5) not obstructing the circuit with the tongue or teeth or deforming the mouthpiece with a bite; 6) disregarding early termination; and 7) preventing re-inspiration. The test was repeated until three usable curves were achieved (meeting at least criteria 1 and 2), without exceeding eight repetitions, each with a rest period <1 minute. 22
Training plan
An RMT period of 8 weeks was established. The initial load corresponded to 50% of the total resistance in cm of H2O in the Threshold IMT system. Participants performed three sets of 10 repetitions a day and the weekly load progression was 7%. The performance was valid when the membrane was mobilized and maintained for at least 2 seconds during inspiration. Training sessions of each participant were recorded and follow-up was carried out every week in person, via email or telephone.
Statistical analysis
Data had a normal distribution, therefore, they are presented as means and standard deviation (σ). Mann-Whitney U test was used to confirm the heterogeneity of the pre- and post-intervention measurements. The level of significance was set at 0.05. R software, version 3.1.2, was used for statistical analysis.
Ethical considerations
The study was approved by the Ethics Committee of the Faculty of Medicine of Universidad Nacional de Colombia, through Minutes 16-155-15 issued on September 22, 2015. Its implementation took into account the guidelines established in the Declaration of Helsinki 23 and the Resolution 8430 of the Ministry of Health of Colombia 24 for biomedical research on human beings, thus this study can be considered as a minimum risk research for its participants, who signed an informed consent prior to their participation. Confidentiality and proper handling of personal data were preserved at all times.
Results
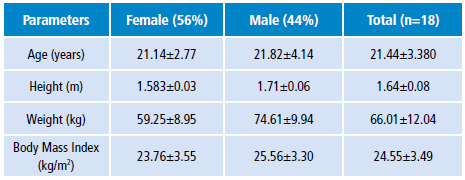
During the pre-intervention phase, 18 subjects were evaluated and, according to IPAQ, were classified as sedentary; of these, 56% were women. The age of the participants ranged between 17 and 32 years; the average body weight was 66.01kg, height 164cm, and BMI 24.55 kg/m2 (Table 1).
For the post-intervention assessment, a sample of 15 subjects completed the 8 weeks training protocol+, of which 60% were women, with an average weight of 65.05kg, height of 1.64m and BMI of 24.14 kg/m2.
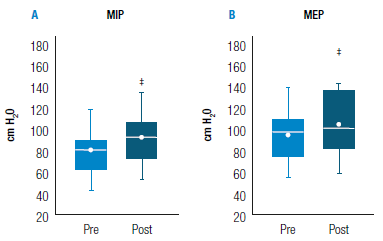
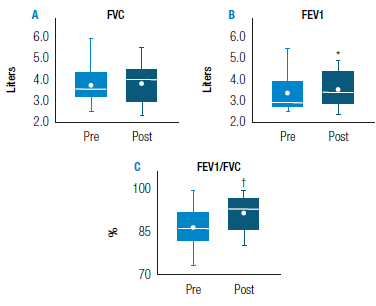
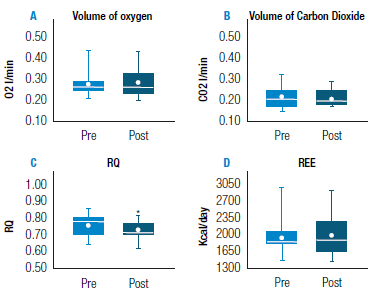
The comparison of pressure, spirometry and pre-intervention calorimetry measurements is summarized in Table 2. Statistical analysis allowed establishing statistically significant differences in the following variables: MIP (p<0.001), RQ (p<0.01) and MEP, FEV1 and FEV1/FVC (p<0.05); on the other hand, measurements of FVC, VO2, VCO2 and resting energy expenditure (REE) did not show significant differences after performing the 8 RMT during 8 weerks.
Table 2 Comparison of changes in pre- and post-training pressure, spirometry and calorimetry measurements.
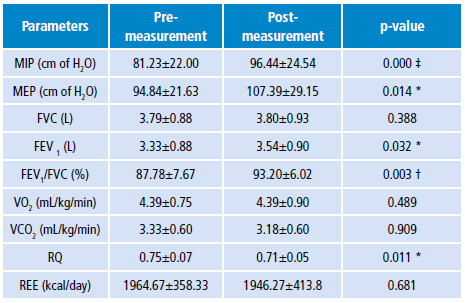
MIP: maximal inspiratory pressure: MEP: maximal expiratory pressure; FVC: forced vital capacity; VEF1: forced expiratory volume in 1 second; VO2: resting oxygen consumption; VCO2: resting carbon dioxide production; RQ: respiratory quotient; REE: resting energy expenditure.
* p<0.05.
† p<0.01.
‡ p<0.001.
Source: Own elaboration.
Measurement of respiratory muscle strength
Clinically and statistically significant increases in MIP values from 81.23±22.00cm to 96.44±24.54cm H20 (p<0.001) and in MEP values from 94.84±21.63cmto 107.39±29.15 cmH20 (p<0.05) were observed (Figure 1).
Pulmonary function
No change in FVC values were observed after the intervention with the Threshold IMT system. In contrast, participants' ability to exhale the greatest amount of volume in the first second (FEV1 increased significantly from 3.33±0.88 to 3.54±0.90 liters (p<0.05); FEV1/FVC ratio went from 87.78±7.67% to 93.20±6.02% (p<0.01). In Figure 2, the dot represents the median, which is very similar in these variables to the mean of the majority, with the exception of pre-intervention FEV1 where the mean is 0.47 liters greater.
V02, C02, RQ and REE at rest
Resting oxygen consumption and carbon dioxide production during the respiratory cycle remained the same after the RMT. Energy expenditure was similar during the pre- and post-intervention phases, while the respiratory quotient (RQ) showed a significant decrease, going from 0.75±0.07 to 0.71±0.05 (p<0.05) (Figure 3).
Discussion
The level of PA was determined using the IPAQ; 18 participants were classified as sedentary and were included in the study. Significant changes were observed in the RMS of MIP (from 81.23±22.00cm to 96.44±24.54cm of H20; p<0.001), MEP (from 94.84±21.63cm to 107.39±29.15cm of H20; p<005) and FEV1 (from 3.33±0.88 to 3.54±0.90 liters; p<0.05).
RMT is one of the strategies used around the world in people with cardiopulmonary impairment or healthy individuals. The prescription of this procedure varies depending on the characteristics of the population and the presence or absence of deficiencies. For this study, the RMT period was established in accordance with previous investigations conducted in non-pathological populations. Enright et al.25 established an 8-week training program with a 80% resistance of maximal inspiratory effort and a fixed volume of 36 repetitions; muscle recruitment intensity was defined by gradually shortening rest times between repetitions. With this form of prescription, statistically significant results were achieved for MIP, lung volumes and TLC.
In contrast, other authors have suggested that RMT at low intensities, such as 40% MIP, can generate significant changes. 11 In this regard, the intensity of the RMT used in the present study, which was implemented for 8 weeks, coincides with reports on the effects on RMS. Volume and training intensity allowed observing changes in respiratory pressure variables, although no significant changes in spirometric parameters and V02 were found.
The effect on RMS observed in each subject varied (Figure 1); in 50% of the participants MIP increases were <20%, while for the remaining participants, they were higher (20-59%). This was also observed in the MEP variable, although changes did not exceed 32%. Differences between subjects may be associated with lack of maintenance of muscle overload during the training period; authors have suggested that a person can reduce the training load by altering inspiratory flow between repetitions, leading to differences in strength. 25
In spite of these differences, the changes in pressure values obtained here coincide with what other studies have reported. 13,14 In this study, with a progressive intensity that reached 60%, improvements were achieved, representing 16% for MIP and 11% for MEP on average. Such changes may be associated with respiratory musculature, which is skeletal, responding to training in the same way as any muscle of the musculoskeletal system according to the theory of training: if intensities between 60% and 80% are applied, maximum effective strength or resistance is gained, and that condition can be maintained. 26
Some authors have described that the adaptive mechanism to training depends on the increase in the proportion of Type I fibers and the size of Type II fibers that directly change the length-tension relationship on which force-generating mechanics of the respiratory system depends. 8,12,23 In addition, greater neural activation of the diaphragm and recruitment of the chest wall muscles are observed during a training program such as the one proposed here. 9
Regarding spirometric parameters, their average values correlate with the reference values described for the Bogotá population. 27 In this study, no significant changes regarding FVC were observed after the intervention; this finding is not unexpected, since they were considered as normal values in the initial assessment considering the participants' anthropometric composition, therefore no major modifications were expected unless a significant decrease in pulmonary function was observed. 28 Another important change was seen in FEV1, which also determines mathematically a better FEV1/FVC ratio. This correlates with the marked improvement of muscle strength parameters, where expiratory muscles are able to generate more power and exhale about 90% of the FVC.
VO2 is related to kinetics of oxygen transport (O2), muscular work and the efficient use of O2 by mitochondria; it is assumed that sedentarism can accelerate the reduction of O2 intake, oxidative capacity and expenditure itself. 29 In this research, no significant differences were observed, which agrees with previous studies in which no increase in VO2 was reported after the completion of an RMT program because the increase of this variable is related to adaptation during long periods of training and is directly proportional to the intensity of the activity, capillary density in the muscle, and number, size and increase of mitochondrial enzymes in the cells of large muscle groups, reaching improvements of up to 50% of VO2 and only 15% in RMT. 30,31
On the other hand, VCO2 values show a 5% decrease, which may depend on the type of food consumed, body or environmental temperature and hormonal activity. RQ ranges from 0.71 to 0.75, indicating that resting energy expenditure occurs by metabolism of fatty substrates. 32 REE represents the number of calories needed for a 24-hour period in which no significant PA is performed. It has been found that, in sedentary people, EER accounts for most of the total caloric intake (60-70%). In indirect calorimetry, this variable depends on the values of O2 and CO2 gases, therefore, the absence of RMT effects, especially on O2 consumption, reported in this study, explains the stability of energy expenditure. 33,34
Conclusions
The 8-week RMT protocol using the Threshold IMT System improved RMS and FEV1 parameters; however, no significant changes were observed in VO2. The adaptive mechanisms that may interfere in the changes observed in muscle strength probably depend on the morphological adaptations of the muscle fibers and the optimization of the recruiting capacity of the chest wall muscles.
It is necessary, on the one hand, to apply RMT programs in combination with other modalities of physiotherapeutic intervention, such as the prescription of multimodal physical activity, to allow greater adherence to this type of treatment and, on the other, to carry out studies with a larger sample size to achieve a greater effect.
Some of the limitations of this study include the lack of follow-up of the participants (three in total), the fact that the Threshold system has a maximum resistance of 41cm H2O -limiting the prescription of higher loads in participants with MIP values >90cm H2O-, and that the training period can influence patterns of adaptation and improvements of lung function parameters. Despite this, this research is expected to provide information that will help further studies in this area.