Introduction
Today, metabolic syndrome (MS) is one of the biggest public health concerns worldwide. 1 The International Diabetes Federation states that the frequency of this syndrome is high in the global context, and is also parallel and congruent with the high frequency of type 2 diabetes and cardiovascular disease in the general population. 1,2 MS is also known as plurimetabolic syndrome, insulin resistance syndrome, or metabolic X syndrome and is defined as the presence or coexistence ofhigh blood pressure, dyslipidemia, insulin resistance, glucose intolerance and visceral obesity. 3 This set of risk factors significantly increases the likelihood of long-term cardiovascular disease. 4
In the past years, university students have shown higher obesity figures. 4,5 Young adults starting college are at a transition age, which is critical to the consolidation of health-related behaviors or habits. 6 For example, first-year college students experience faster weight gain than the average adult at another stage of life. 7 This relates to lifestyle choices, including poorly balanced diet, lack of physical activity or regular exercise, tobacco use, and excessive consumption of alcoholic beverages. 8 It has been fully established that these factors, together with obesity, contribute to increased risks of suffering from MS, regardless of age and educational or vocational level. 9
Early detection of MS in young adults in the university context may guide the design of preventive programs or specific interventions to reduce the onset of the syndrome and associated medical and psychosocial complications that often become chronic. 10
It is important to know the prevalence of MS in university students in order to take measures from a public health perspective and design strategies for early identification. This design is done using different screening techniques of possible cases in the academic context, and aims to reduce or minimize the problems associated with MS and the subsequent deterioration in the quality of life once current students are part of the country's productive system. 11,12
To date, there is no systematic review summarizing the observed prevalence of MS in university students in different contexts. Systematic reviews in other age groups showed striking values and a systematic review including obese adolescents revealed a mean prevalence of 31.2% ranging from 2.1% to 58.3%. 13 A similar review, including adults aged between 18 and 65 years, apparently healthy, from Latin American countries, found an adjusted prevalence of 24.9%, with a range between 18.8% and 43.3%. 14
The objective of this systematic review was to establish the prevalence of MS in the university population as reported in studies published between January 2000 and January 2016.
Materials and methods
A systematic review of studies published in the PubMed, LILACS, ScienceDirect, UpToDate, Imbiomed, SciELO and Google Scholar databases between January 2000 and January 2016 was carried out to review the prevalence of MS in university students.
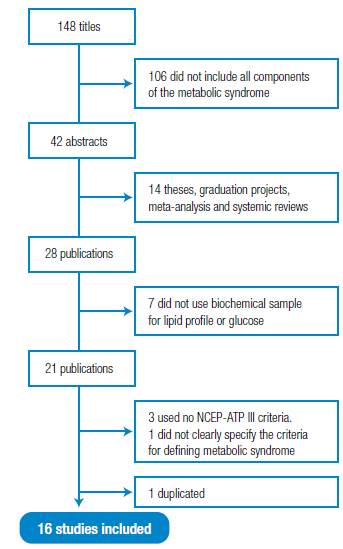
"Metabolic syndrome", "Cardiovascular risk factors", "University students" and "Students" were included as keywords. In order to ensure the largest number ofpublications, different word combinations were used in Spanish, English and Portuguese. This process was complemented by a manual review of the references of articles initially identified in the database search. Studies that evaluated the presence of MS according to the criteria of the National Cholesterol Education Program and the Adult Treatment Panel III (NCEP-ATP III) were included. 15 Figure 1 presents the flowchart of the selection of the reviewed studies.
NCEP-ATP III defines MS as the coexistence of at least three of the following factors: increased abdominal perimeter (≥102cm in men and ≥88cm in women), hypertriglyceridemia (≥150 mg/dl), decreased HDL (<40 mg/dl in men and <50 mg/dl in women), fasting hyperglycemia (≥110 mg/dl) and altered blood pressure (systolic blood pressure ≥130 mm Hg or diastolic blood pressure ≥85 mm Hg). (15,16) Narrative reviews, graduation projects, theses and studies carried out in the university context in which professors or administrators were mixed and the prevalence in the student group that could not be discriminated were excluded.
First, the titles were reviewed, then the abstracts and finally the full version of the articles that met all the inclusion criteria. A descriptive analysis of the publications was carried out and the country in which the study was conducted, year of publication, sample size, major/program, academic level of the population studied, and observed prevalence of MS in percentages were specified. For a more accurate observed prevalence, 95% confidence intervals were found for each of the frequencies reported in the articles.
The quality of the studies was evaluated using the questionnaire for observational analytical studies proposed by du Prel et al.17. This instrument consists of 12 points that collect the most important aspects of the design and non-experimental observational studies analysis, as proposed by the instrument Strengthening the Reporting of Observational Studies in Epidemiology.18
Results
148 titles were identified, of which 120 were discarded since 106 did not include all the components of the MS and 14 were theses, graduation projects, meta-analyses or systemic reviews. Of the 28 pre-selected abstracts, 7 investigations that did not use biochemical tests to define MS were eliminated, as well as 3 that used criteria other than NCEP-ATP III, finally 1 study that did not clearly specify the criteria used to define MS, and 1 duplicated were also excluded. 16 studies met all the criteria for this review. 19-34 Regarding the quality of study reports, all met at least 11 of the 13 criteria assessed (10 met 13, 5 met 12, and 1 met 11). The articles with the lowest scores usually had smaller samples.
In general, studies conducted in different parts of the world, most of them from Latin America or Brazil, were included. In terms of the major or program to which the students were enrolled, the largest selection was made randomly from all programs (10 studies). The age of the participants ranged approximately between 17 and 26 years, and both men and women participated. The prevalence range of MS ranged from 0% to 19.2%. Table 1 summarizes the information on the findings of the studies in chronological order.
Discussion
This study shows a high variation in the prevalence of MS in university students, which is between 0% and 19.2% according to the NCEP-ATP III criteria. In this sense, 10 studies found a prevalence of MS of <5.0%, 3 between 5.1% and 15%, and 3 of >15%, and this is somehow different from what has been reported in other systematic reviews in children, adolescents and adults.
Friend et al.35 made a systematic review with 85 published studies in children and adolescents between 2003 and 2010 and found an average prevalence of MS of 3.3%. Other systematic reviews of findings in adult populations show a substantially higher prevalence. For example, Oguoma et al.36, in 32 published studies between 2002 and 2013 worldwide, with a total sample of 10 854 subjects, found that the average prevalence is 27.9% according to NCEP-ATP III. De Carvalho-Vidigal et al.37 reviewed 10 articles in Brazilian subjects, published until May 2013, with a total participation of 8 505 people, and found an average prevalence of MS of 28.9% according to the same criteria.
Table 1 Prevalence of metabolic syndrome in university students (NCEP-ATP III).
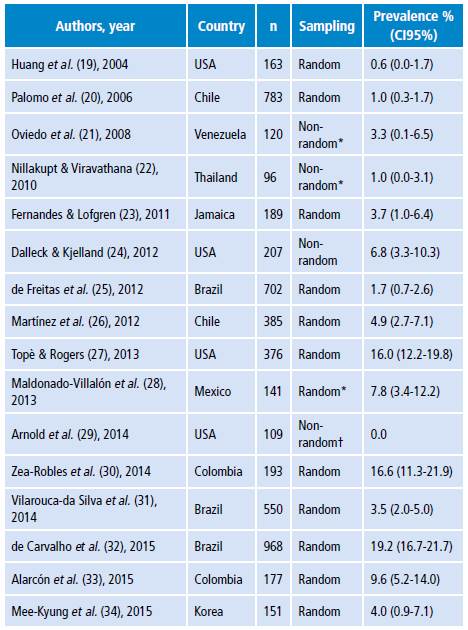
Source: Own elaboration.
* Medical students only.
† African-American students only.
Certainly, the differences in the prevalence percentages and variables associated with MS observed between the studies reviewed in this research and previous systematic reviews may be explained by the variety of demographic and cultural characteristics of the participants. 38 Likewise, social and economic inequalities should be considered, not only those that occur between countries, but also those that are found in different regions of the same country. The prevalence of obesity and, consequently, of MS tends to be higher in developed or high-income countries. 4
It is relevant to know the prevalence of MS in university youth, both for education and public health. This information about the frequency in university institutions is fundamental to encourage, based on the best evidence, the promotion of healthy lifestyles that include non-pharmacological measures such as diet and exercise at this stage of life. 39 Moreover, these measures may need to be implemented at elementary and secondary education levels 40-42 due to the increasing prevalence of obesity in the early years of life, which is the main component of MS. 43-45
From a public health perspective, this prevalence is relevant for promoting metabolic disorders, and control and reducing associated long-term morbidity and mortality. 46 It is important to promote preventive actions based on a healthy lifestyle that include a balanced diet -for example, the Mediterranean diet, which has demonstrated to be helpful to reduce and prevent metabolic disorders- and habits such as regular physical activity. 47 These actions can be included in the curricular and extracurricular components of vocational training programs as ways to promote self-care. 48,49 Similarly, it is necessary to work for the promulgation of public policies more aligned with a healthy lifestyle from the early stages of life. 50-52 The strength of this systematic review is that it summarizes the research done in the university population of the last years to date, which were not included in any systematic review. The search also included articles in Spanish and Portuguese that are not usually considered in English-language publications. However, there are some limitations, including that the participating populations showed high heterogeneity in their characteristics and in the quality of the studies, which greatly limits the generalization of any conclusion.
Conclusion
Prevalence of MS in university students is high when compared to that observed in children and adolescents; therefore, further research with more representative or stratified samples is needed to know the frequencies in different sectors or subgroups of university populations, which will allow the design of specific interventions for high-risk groups in the university context.