Introducción
The term prosthesis comes from the Greek words pro, meaning forward or in front of, and thésis, denoting placement. Thus, this word refers to a component that replaces an absent or affected part of the body. Orthopedic prostheses are used to partially or totally replace a segment of a missing or deficient limb and their main obj ective is to provide the possibility of restoring functional capabilities to people with amputations; ideally they become extensions of the user's body. 1,2 In general, prostheses can be classified according to the level of amputation, as detailed in Table 1. 2-4
Table 1 Nomenclature for lower limb prosthesis and orthoses.
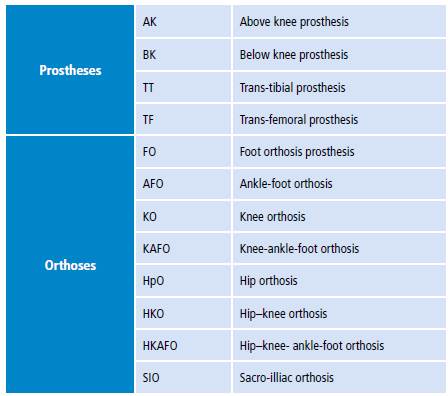
Source: Own elaboration based on Rajt'úková et ai.3 and Hsu et al.5
On the other hand, orthoses are externally applied devices that are used to modify the structural and functional characteristics of the neuromuscular and skeletal system. 1 These devices are classified based on a nomenclature system in English and according to the anatomical segments and joints they cover. Table 1 presents the most common classifications. 1
The sockets and their liners are the main components of orthoses and prostheses, and are elements of interest for this review article.
For ]prostheses, there are rigid and soft concave sockets. Rigid sockets must distribute the loads generated during gait on the residual limb 6, while soft sockets (also called prosthetic liners) are systems that cover the residual limb and are designed to properly fit the prosthesis; they provide greater freedom of movement, proper control and transfer of loads, and diffusion of uniform pressure over the entire surface of the affected limb. 7-10 These devices have allowed the elimination of additional external fixation systems and are also divided according to the type of prosthesis. 8
On the other hand, orthoses may consist of a rigid socket that allows achieving the clinical goals of patients, and a soft interface to cushion and distribute the efforts and pressures generated during the gait cycle. 5 In all cases, they should be manufactured according to the degree of mobility required and the shape of each patient. 11 It should be stressed that both the soft prosthesis liners and orthoses interfaces are in permanent contact with the skin of the affected limb and are crucial for patient comfort. 6 Table 2 presents the different types of liners.
External orthoses and rigid prosthetic sockets are usually made from plastic materials, which are solid polymers in their final state. 5
Because of the use conditions, the design and the materials of sockets and interfaces, there may be consequences related to skin problems and infections on patients. 12,13 Therefore, conducting a literature review is important to gather relevant information that allows identifying publications on the materials used for the manufacture of liners and sockets for orthoses and prostheses, as well as possible skin problems of the affected limbs in contact with these devices.
This article aims to document the variety of polymers used in the development of lower limb sockets and external prosthetic and orthotic interfaces, their functional requirements and the possible skin problems generated by their use. For this purpose, the present paper reports the findings of a literature review on the basic requirements of materials and polymers used to manufacture sockets and interfaces for lower limb prostheses and orthoses, the advances in current devices and the most frequent skin problems generated by the use of such devices.
Materials and methods
For this literature review, a search was carried out on polymers used for the manufacture of prosthetic and orthotic lower limb interfaces and sockets, their functional requirements and the skin problems caused by their use; publications made between 1989 and 2017 were taken into account. The search was made in the EBSCO, Embase, LILACS, SciELO, ScienceDirect and Scopus databases, and other publications found in Google Scholar were also considered. The review was made in March 2017.
The search keywords used were materials, orthoses, prosthesis, polymers, dermatologicalproblems, interfaces, socket, observational study and clinical study, with their equivalents in Spanish. In addition, similar search combinations were designed according to each database or information bank, in which search equations were used with the Boolean terms AND and OR.
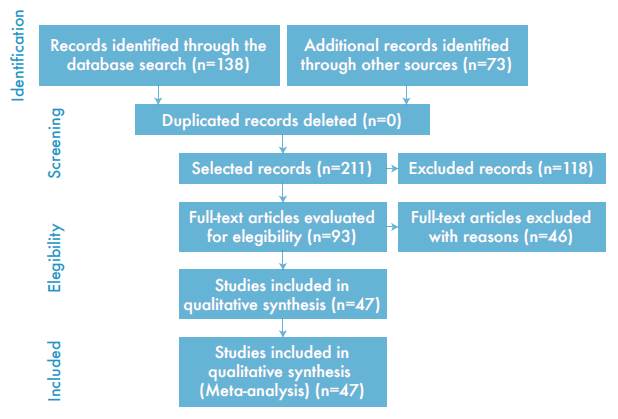
The initial inclusion criteria taken into account to incorporate the data obtained in this study was the agreement between the subject matter of the review and making reference to polymers used to produce lower limbs orthoses, interfaces, sockets or prosthetic and orthotic liners, their requirements or conditions for use, and skin problems associated to the use of these devices. Incomplete texts that were not original studies or reliable were excluded because they were not supported by academic databases, were not approved by an author or organization, or did not present bibliographic references. The search was conducted in English and Spanish, obtaining 211 references from which 164 records or articles were excluded. Figure 1 presents the flowchart of the studies included in the review and then presents the results based on 47 references.
Results
Basic requirements for materials used in lower limb sockets and prosthetic and orthotic interfaces
Depending on the clinical treatment goals and functional requirements, the materials used in the construction of orthoses and prostheses have different properties. Clinical goals of orthoses include relieving pain, controlling deformities, preventing excessive range of joint motion, increasing range of joint motion, compensating for abnormalities, protecting tissues, and promoting healing. On the other hand, the purpose of prostheses is to replace an absent or deficient limb. These objectives are achieved through functional requirements, such as preventing, reducing, or stabilizing a deformity; limiting the mobility of a joint; or reducing or redistributing a load on specific tissues. Thus, some materials used for the construction of prosthetic and orthotic devices are flexible to adapt to the body and absorb the energy generated during the gait cycle, or rigid to control the bending generated by the loads. 1,14-16 Similarly, prosthetic and orthotic devices must be safe and durable, and have sufficient strength to withstand the maximum stresses expected from being subjected to normal pressure by the action of weight and gait, which generate tensile and compressive stress, in addition to tangential stress that occurs when prosthetic and orthotic interfaces and the affected limbs interact. 5,16-19
Materials with high tensile strength improve the suspension and adjustment of the devices by reducing pistoning or slipping during the gait cycle. However, it is important to clarify that this phenomenon depends not only on the mechanical characteristics, but also on the presence of friction in the contact area, which depend, in turn, on the adhesion and deformation properties of the materials. 7,8,19 Moreover, the stiffness of the material should be considered, as it depends on the state of the soft tissues in the affected limb: individuals with little bone end covering require coatings with low compression stiffness, while those with abundant soft tissue can achieve a better sense of control from interfaces with a little more stiffness. 7
These parts must allow for shape variability and must adapt to fluctuations in the volume of the lower limbs, while maintaining their overall structure, thickness, complete contact with the skin and tolerance to pressures generated during the gait cycle. 8,20 Thus, the prosthetic and orthotic sockets and interfaces must allow for the damping of the stresses generated and adequate adjustment to correctly transfer the pressures when using them, taking into account the clinical requirements of each patient.
Materials used for manufacturing sockets and liners for orthoses and prostheses
External orthoses and prosthetic rigid sockets are developed from thermostable or thermoplastic polymers. The former are hard and rigid polymers, even at high temperatures, and it is not possible to melt them with heat, which makes their manufacturing processes complex. 21-23 The latter have a high molecular weight and can be plasticized by pressure or temperature 23; among the most commonly used of this type are high and low-density polyethylene (PE) and polypropylene (PP). 22
PE is characterized by its flexibility, ease of vacuum forming, and low weight, so it is commonly used in orthoses and artificial limbs requiring flexibility. 5,23 PP is the lightest of the plastics used in orthopedics and is characterized by its high tensile strength, stiffness, and hardness; however, it is sensitive to deformation, and its surface can easily deteriorate with heat. PP is commonly used in the manufacture of sockets for prostheses, splints, and orthoses requiring high rigidity 5,23; thermoforming has replaced some traditional materials in prosthetic and socket practice, reducing processing and manufacturing times. 5,21,23
Orthoses and prosthetic sockets have been built from composite materials, in other words, they have a matrix and one or more reinforcements joined by an interface to improve the properties of the parts. 23,24 The matrices are the body of the material and must guarantee the stability of the pieces in the environment. 23,24 Some of the most common for rigid sockets are unsaturated polyester resins, epoxy and vinylester. The reinforcing agents fundamentally define the mechanical properties of the composite material and can be particles or fibers.
Arun & Kanagaraj 22 enhanced the performance of prosthetic sockets made from epoxy resins, smooth glass fabric and between 2 and 10 bales of elastic fabric by incorporating 0.3% (w/w) of carbon particles called multi-walled carbon nanotubes. Flexural strength and thermal conductivity were found to increase by 11.38±1.5% and 29.8±1.3%, respectively, in compounds with 4 to 10 layers of elastic tissue; flexural modulus in compounds with 2 to 10 layers of elastic fiber increased by 4.5±1.4% compared to epoxy resin compounds without nanotube reinforcement. This also reduces the weight and heat generated by rigid prosthetic interfaces.
In contrast, fibers are more used in sockets for prostheses and orthoses, as they considerably increase mechanical properties such as strength, stiffness, hardness, and dimensional stability of polymeric compounds. 5 Fiber arrangement and the variation in the fraction of fibers volume allow varying the characteristics of the materials. 5,24 Aramid fibers are so resistant that they can surpass steel or aluminum; however, they are not ideally compatible with matrices like glass or carbon fibers. Fiberglass reinforcement improves most of the mechanical properties of plastics, so they have been used in prostheses with polypropylene and high-density polyethylene matrices; still, a decrease in the mechanical performance of the device and patient comfort has been reported. 24 Carbon fiber, on the other hand, considerably increases the mechanical properties of thermoplastic composites, adds stiffness and high resistance to the material (up to 35 000 psi), and reduces the weight of the reinforced material. 23-26 However, unlike some plastics, carbon fiber cannot be reheated to allow reshaping and, therefore, its adaptation processes must be accurate. 27
Soft interfaces for prosthetic and orthotic devices have been developed from shock-absorbing foams and interface systems designed to provide filling and cushioning in the affected limbs. Cushioning foams can be designed from urethane and can be rigid, soft or elastic and extremely vary in density according to their cells, so they are widely used for the keel of prosthetic feet and internal coatings of orthosis and prosthetics with hypoallergenic properties. 21 Also, latex, polyurethane and polyethylene cushioning foams -such as plastazote and pelite- have low weight and good capacity to recover and support compression loads. These foams are generally used along with denser foams to achieve smoother interfaces and slower load compression. 5
For lower limb prostheses, it is common to find liners for the patient's residual limb. These are mostly made from silicone gels, silicone thermoplastic elastomers (TPE) and some additives. 7,20 Silicone gel interfaces contain slightly crosslinked polysiloxane networks, with high polydimethylsiloxane (PDMS) free fluid content, thus allowing liquid extension under load. 7 However, they have lower compressive strength, shear and tensile stiffness than silicone elastomer liners, which are quite crosslinked and, unlike gels, contain little PDMS-free fluid, allowing them to keep their liquids under pressure. 7 The viscoelastic nature of silicone allows the flow of high pressures towards low-pressure areas under heavy loads and increased walking performance by reducing the use of additional aids and improving the suspension of prostheses. 21,28,29 Figure 2 presents a summary of the polymers used for external lower limb prosthetic and orthotic devices.

Source: Own elaboration.
Figure 2 Polymers used for external lower limb prosthetic and orthotic devices.
Datta et al.30 have reported greater control of prostheses and decreased abrasion and skin irritation in transtibial amputees using silicone interfaces. The positive effects of the use of silicone liners can be attributed to the way the material adheres to the stump and its properties. 29 This type of liner has an excellent shape memory and a minimum hardness of 30, average hardness of 40, and high hardness of 40 to 50 on the Shore 00 scale. In addition, they do not require much thickness to absorb the efforts of a prosthetic socket, and it is possible to produce them from a catalyst and a resin, but its shape cannot be modified. 20
Sanders et al.31 subjected 15 types of commercial liners to compression, friction, shear and tension tests. Silicone gel liners were the softest during compression trials, suggesting that they may be the most appropriate for cushioning bony prominences, but had less resistance to compression, shear, traction and stiffness than silicone elastomer.
Skin problems caused by the use of external lower limb orthoses and prostheses
The use of prostheses and orthoses requires a suitable fit with the affected residual limb or stump; in this process, it is also necessary to exert forces that correct or stabilize a segment of the body over a long period of time. Nevertheless, a device that does not fit correctly to the conditions of the body or residual limb, that has insufficient resistance, or is used for long periods of time, can cause trauma to the limbs and induce skin problems. 32-34
Skin problems can occur throughout the life cycle of the devices and are caused by various circumstances. These disorders include those induced by pressure, friction, shear, tension and stress. 35 Friction between the skin and the device can cause tissue ischemia and skin breakdown, while shear injuries can cause damage to the deep layers of the skin. 35 Moreover, mechanical stress on the skin in contact with orthoses and prostheses results in the destruction of the dermis and in lesions that stimulate tissue proliferation. 12,13,35,36 For example, prosthetic liners must be adhered to the skin to promote proper suspension; however, these components pull a small amount from the limb in each phase of the oscillation, generating vertical movements called pistoning, which are produced by the elasticity of the material and cause damage to subcutaneous tissues. 37 It has also been hypothesized that hidradenitis suppurativa is caused by mechanical stress accompanied by a warm and humid occlusive microclimate in people with lower limb amputation, which also favors the presence of bacteria. 35
Another circumstance that affects the skin of users is related to the tight fit that generates excessive pressure on the skin, especially in bony protuberances or irregular residual limbs. 37 Sbano et al.38 reported a case of dermatitis clinically similar to verrucous hyperplasia on the residual limb of a patient with lower limb prosthesis due to the rigid suction socket of the device; the authors associated the presence of that disorder to the type of socket and the poor adaptation of the residual limb to the prosthesis as a result of the need for adaptation of the skin by the technical aid.
Furthermore, the heat generated by the prosthesis or orthosis socket causes a tendency for the skin to perspire, so the increase of humidity causes injuries and infections. 39 Folliculitis and similar inflammatory conditions may be more recurrent in people with hairy extremities or sensitive skin. 40 Other problems are also caused by hypersensitivity to the material, lack of hygiene, or presence of bacteria or fungi. 38 Some of the bacteria species that usually populate residual limbs or affected legs when using prosthetic and orthotic devices are Staphylococcus epidermidis and Staphylococcus aureus. Moreover, the constant interaction of the skin with orthoses and prostheses also provides an ideal environment for the growth of dermatophytes and Candida albicans.36,41 Also, due to the presence of microorganisms, pre-existing skin disorders may recur or cause allergic reactions caused by ointments used for skin care. 21,22 These problems can be exacerbated by the device over time. 36 Table 3 shows the skin problems associated with the use of external lower limb orthoses and prostheses, and their main causes.
In the mid- 1980s, Össur Kristinsson developed the Icelandic roll on silicone socket (ICEROSS) with the aim of offering more comfortable sockets that would provide better suspension and alleviate the skin problems associated with the previous designs. This type of socket has become a standard for the treatment of transtibial amputees. 47 However, in 2008, Hall et al.47 conducted a study to determine the prevalence of skin problems in people using this type of coating, and found that 90.9% of subjects reported problems in their medical history and 78% during the study, regardless of the cause of amputation. Common problems included excessive sweating, itchy skin, and redness.
Literature shows that, since 2000, there has been little research on the incidence of skin problems associated with the use of external lower limb prostheses and orthoses. In 2001, Dillingham et al.48 found that about a quarter of the amputees surveyed reported skin irritation problems, wounds, or constant pain in the residual limb; Hagberg & Brånemark 49, when studying individuals who used transtibial prosthesis, found that the most frequent problems that led to a decrease in quality of life were heat and sweating in the prosthetic socket (72%), factors that favor the presence of skin problems.
In 2005, Dudek et al.36 reported the frequency of skin problems in 745 lower limb amputees using prostheses through a 6-year retrospective review, finding that 40.7% of the cases had at least one skin problem. Similarly, Meulenbelt et al.50 identified the determinants of skin problems in lower limbs or prosthesis of amputees through a survey in 2009; out of 805 people, 63% reported at least one skin problem, and the biggest determinant was the use of antibacterial soap, followed by smoking and frequent washing of the residual limb.
The following year, Ghoseiri & Bahramian 51 evaluated the satisfaction of 172 women and 121 men wearing prostheses and orthoses in Iran. When asked whether the skin was free of irritation and abrasion, the result yielded an average of 2.0 with a standard deviation of 1.1, where the overall satisfaction score ranged from 0 to 100 (the lowest and highest possible score, respectively). 51 That same year, Meulenbelt et al.13 reported a cross-sectional survey consisting of a questionnaire and a clinical evaluation in order to estimate the prevalence of skin problems in the residual limb of patients; of 124 subjects, 36% reported having skin problems, including cold skin and excessive perspiration, skin problems that usually trigger pain, affecting people's performance. 37 Furthermore, between 2014 and 2015 a study was conducted in Colombia with 150 people who used lower limb prostheses, finding that 78% of the sample had presented some discomfort or condition in the residual limb, having irritation as the painful condition with the highest incidence. 52
These studies show that skin conditions are frequent complications in people who use prosthetic and orthotic devices (Table 4), with prostheses being the most common cause of these conditions. The risk of skin problems differ from one device to another and depend on each individual. 40
Table 4 Summary of selected studies regarding skin problems associated with the use of orthoses and prostheses.

SP: skin problems; P: people; O: observed by specialists; R: reported by patients; M: males; F: females
Source: Own elaboration based on Meulenbelt et al.13, Dudek et al.36, Hachisuka et al.39, Hall et al.47, Dillingham et al.48, Meulenbelt et al.50, Ghoseiri et al.51, Quintero-Quiroz et al.52, Dudek et al53.
Discussion
It has been found that the basic requirements of external lower limb prostheses and orthoses depend on the clinical objectives that these devices have for each patient. In addition, they should comply with mechanical, safety and durability requirements, and not generate problems in the skin of the users that may result in injuries or destruction of the dermis. Similarly, allergic reactions on patients should be avoided, and variables such as temperature and humidity in the residual limb or lower limb should be controlled through sockets and interfaces. 12,36
Sockets and liners for orthoses and prostheses are manufactured from a large number of materials, and can be classified according to the stiffness and strength required, both for external orthoses and prosthetic rigid sockets, as well as for prosthesis liners and prosthetic and orthotic soft sockets. Materials used include some thermostable or thermoplastic polymers and some composite materials; the latter have achieved a great boom in orthoses and prostheses applications thanks to their ability to achieve unique physical, chemical, or mechanical properties by joining different materials that would not work individually. However, one possible disadvantages of a greater use of this type of materials is price, given that the processes for obtaining them could make the rigid composite parts more expensive. In order to compensate, the possibility of developing new materials from the combination of recyclable components and creating new processes for the combination of elements that do not involve high-cost equipment could be considered; also, the outstanding mechanical properties obtained may, somehow, overcome the disadvantages.
On the other hand, cushioning foams are commonly used to develop soft prosthetic and orthotic sockets, while silicone gels and elastomers are often used to obtain lower limb prosthesis liners. One drawback of foams is the loss of elasticity over time and the possibility of being affected by moisture, so they must be replaced regularly; body heat must also be isolated, as it increases transpiration in contact areas. 5 For their part, silicone elastomers, being highly crosslinked, have a greater capacity to support applied loads and internal efforts, and have greater shape recovery and thickness when subjected to compression tests with respect to silicone gel coatings and cell foams. The physical explanation for this is associated with the ability of silicone elastomers to deform when impacted by loads and to align their polymer chains perpendicular to the direction of the load, and then harden as they withstand stress. 31 Studies have shown that the difference between the tensile stiffness of coatings with and without fabric reinforcements is minimal; however, fabric reinforcements could increase the tension at which the coating fails and reduce the shear stress applied to the skin, favoring sliding at the liner-socket interface.
As shown by the results, interfaces developed from polymers are widely used because they are lighter and have structural differences that allow obtaining a wide variety of properties thanks to their chemical and physical structures. In spite of this, some of the materials commonly used for these devices do not meet the best performance criteria, as they have limited durability and not so favorable weight-resistance ratio, not to mention that some of them, such as carbon fiber and nylon 6, are expensive and have to be imported, which increases production costs.
It was also found that the use of external lower limb prosthetic and orthotic devices can generate skin problems that affect the health and well-being of users, preventing proper gait cycle, and leading to the decision of restricting or completely abandoning these support elements. However, some studies do not directly relate skin conditions to the different designs and types of materials of the prosthesis or orthosis. Although there are many proven cases of difficulty in adapting to these devices, the problems generated are not easily attributable to a single cause such as the materials, because, even though the theory explains it, the bibliographical references are not conclusive since they do not provide sufficient scientific evidence regarding the direct relationship between skin problems, materials and designs of the sockets and prosthetic and orthotic interfaces.
Nevertheless, for the moment, it is necessary to take into account some general recommendations to prevent rapid deterioration of the devices and prevent skin problems in users. Cleaning the plastic components of the devices with cold water and making sure to remove all residual moisture without using heat is highly recommended, as they deform polymers, especially thermoplastics. Any substance that is applied over the interfaces must not have irritating components, as they would come into direct contact with the skin. 40 To minimize problems of skin intolerance, it is recommended to start using them gradually; for users with sensitive skin, preventive measures related to the use of interspatial foam or silicone coatings can be applied, and adequate hygiene of the contact areas should be performed. 40 Early treatment and the support of specialists are relevant to deal with any manifestation of skin disorder or irritation, as well as avoiding home treatments that can damage the skin, making it even more susceptible to the aforementioned disorders. 37 Finally, the importance of educating device users and their families regarding cleanliness, hygiene and skin care is especially emphasized, as well as the relevance of having specialists with adequate knowledge that can help choosing the correct device according to the needs and conditions of each patient.
Conclusions
Safety, durability and fulfillment of clinical objectives without harming the patient are some of the basic functional requirements that lower limb orthosis and prosthesis interfaces and sockets must have. The literature demonstrates the importance of the mechanical properties of the sockets and interfaces to support the efforts generated by the gait cycle, and to avoid failures and ruptures that negatively affect the use of prosthetic and orthotic devices.
It is evident that one of the most commonly used polymers for the manufacture of orthoses and prosthetic rigid sockets is high-and low-density polyethylene, which is flexible, easy to vacuum mold and lightweight, which favors the manufacture of devices that require flexibility for users with little residual limb coating. Using polypropylene is also common for this type of applications due to its high tensile strength, hardness and rigidity, which in turn is useful for the manufacture of orthoses or prostheses with clinical requirements of greater stability, like in individuals with abundant soft tissue in their affected limb. However, these thermoplastic polymers can easily be deteriorated by heat and have a very short service life. For this reason, polymeric compounds have become a useful alternative, since they allow obtaining unusual properties that are not possible with primary materials; they also allow incorporating additives that contribute to avoiding skin problems caused by externally applied devices.
Furthermore, the soft interfaces for prostheses and orthoses are largely designed with silicone gel or elastomer, urethane, polyurethane and latex. They have shock-absorbing properties, and favor an adequate fit to the device, achieving a proper transference of the efforts and the generated pressures, and granting well-being to the patients. However, these same interfaces can generate skin alterations such as excessive perspiration, wounds, irritation, among other conditions.
Studies estimate that between 32% and 90.9% of the population with lower limb amputations or requiring an external modification in their structure or function develop at least one skin problem due to the contact with prosthetic and orthotic devices. Until now, no direct relationship has been identified between the incidence of skin problems and the materials and designs of the sockets and prosthetic and orthotic interfaces, but some of the main causes for the presence of skin problems in this population include the mechanical loads exerted on the limbs, the increase of temperature, and the generation of humidity or the presence of microorganisms when using external lower limb orthosis or prosthesis. There is evidence that collaborative work is relevant to investigate the development of durable and resistant composite materials that have the ability to prevent or control damage to users' skin, high temperatures, or humidity at the sites of contact with the devices.