Introduction
Insulin resistance (IR) is defined as a decreased response to the effect of the hormone, mainly on the liver, skeletal muscle and adipose tissue, and its pathophysiology has been strongly associated with the etiology of obesity. 1 IR has been described as a major risk factor for type 2 diabetes mellitus and cardiovascular disease, conditions that have high morbidity and mortality rates, which explains its diagnostic importance. 2
To this end, the standard method used is the euglycemic clamp, which evaluates fasting glucose regulation based on insulin concentrations in vivo 3; however, this method is costly and invasive, and this hinders the frequency of its use in clinical practice. Other methods have been developed to determine IR indirectly, including Homeostatic Model Assessment Insulin Resistance (HOMA-IR), Quantitative Insulin Sensitivity Check Index (QUICKI) and the McAuley Index. 4 The first two use fasting glucose and insulin levels to establish a diagnosis, and the third is based on a relationship of fasting triglyceride and insulin levels. 5
The use of HOMA-IR in routine clinical diagnosis has allowed observing that reference values range from 2.6 to 3.8 in adult and pediatric populations in different regions of the world 6-9; therefore, determining reference values for specific populations is highly suggested. 10-13
The state of Chiapas has a total population of 5 217 908 inhabitants, of whom 74.7% live in poverty and 33.5% lack access to health services. 14,15 Regarding overweight and obesity, a combined prevalence in adolescents from urban areas of the state of 33% has been reported 16, with a HOMA-IR range for the capital between 0.4-7.5 and 21% in obese adolescents. 17 These is relevant when taking into account that more than 80% of deaths from noncommunicable diseases such as type 2 diabetes occur in low- and middle-income countries such as Mexico. 18
The objective of this work was to determine HOMA-IR values and their correlation with the body mass index (BMI) for age percentiles in children and adolescents from the Soconusco region of Chiapas, Mexico.
Materials and methods
A cross-sectional study was conducted on individuals who used the clinical laboratory of the Tapachula Regional Hospital, Chiapas, from May to July 2015. The protocol was approved and filed on June 29, 2010 by the Research Committee of the General Directorate of Research and Graduate Studies of the Universidad Autónoma de Chiapas under code 02/QUI/RPR/290/10. This work complied with the ethical principles of the Declaration of Helsinki 19 and all participants and parents/guardians signed an informed consent. Children and adolescents of both sexes, between 5 and 19 years of age, presenting signs of metabolic control without presumptive diagnosis of the disease, were included in the study.
For biochemical determination (glucose and fasting insulin), a 6mL sample of peripheral blood without anticoagulant was taken from each study subject, with an 8-10 hour fast. The variables age, sex, height, weight and body mass index (BMI) were obtained by applying a physical examination questionnaire and taking anthropometric measurements with trained personnel at the Tapachula Regional Hospital. To measure weight and height, a clinical scale with a stadiometer was used (Clínica-160, Básculas Nuevo León®, México) and the Centers for Disease Control and Prevention (CDC) BMI percentiles were used to determine obesity and overweight 20; BMI between the 5th and 85th percentile was taken as normal weight, and BMI ≥85 was considered as obesity and overweight.
Glucose was determined using glucose oxidase-peroxidase (Glicemia enzyme AA, Wiener Lab., Argentina) and insulin was determined using the ELISA immunoassay (Insulin ELISA test, Diagnostic Automation, INC., USA); the automated ChemWell® 2910 (Awareness Technology Inc., USA) was used for both determinations. The HOMA-IR calculation was performed by adapting the formula proposed by Matthews et al.21:
Fasting glucose (mg/dL) x fasting insulin µU/ml)/405 The SPSS 21.0 software was used for statistical analysis, with 95% confidence. Data was described based on the following three parameters: frequencies, mean ± standard deviation, or median (interquartile range). For the comparison of the variables between groups, student's t and Mann-Whitney U tests were used according to the normality of the data, and Spearman's rank correlation coefficient was used to determine the correlation between variables.
Results
The study sample consisted of 112 subjects, 55 girls (49%), with a median age of 12 9-13 years. Average weight, height and BMI were 47.0±12.8kg, 1.4±0.1m and 21.9±3.8 kg/m2, respectively. Regarding the comparison by sex, both weight and height, and BMI were homogeneous (p=0.473, p=0.190 and p=0.696). The general population showed a combined prevalence of overweight and obesity of 66%: 70% for males and 62% for females (p=0.350). The analysis of the biochemical variables revealed a mean glucose concentration of 80.5±8.4 mg/dL, an insulin median of 7.7 μU/mL (4.8-15.02), and an HOMA-IR of 1.6 (0.90-3.06). The three variables presented homogeneity between sexes (Table 1).
Table 1 Anthropometric and metabolic description of 112 children and adolescents in the Soconusco region of Chiapas, Mexico.
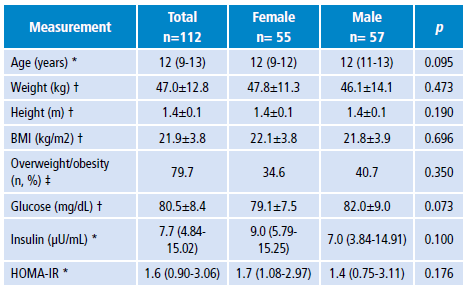
BMI: body mass index; HOMA-IR: homeostatic model assessment insulin resistance.
* Description with median. Contrast: Mann-Whitney U
† Description with median ± standard deviation. Contrast: Student's t
‡ Description of frequency. Contrast: Chi square
Source: Own elaboration.
According to the body weight diagnosis, the mean glucose concentration was homogeneous between groups (normal weight = 79.9±8.1 mg/dL vs. overweight/obesity = 80.9±8.6 mg/dL, p=0.1456). The overweight/ obesity group presented insulin and HOMA-IR medians of 9.16 μU/mL (5.5-15.99) and 1.8 (1.0-3.2), respectively, which were significantly higher than the values of the normal weight group at 5.9 μU/mL (3.5-12.7) (p=0.010) and 1.3 (0.67-2.50) (p=0.015), respectively.
The correlation analysis found that HOMA-IR is positively and significantly related to the increase of the BMI percentile (r=0.198, p=0.037) (Figure 1) .

Source: Own elaboration.
Figure 1 Correlation analysis of HOMA-IR with age, weight, height and body mass index percentile in 112 children and adolescents from the Soconusco region of Chiapas, Mexico. A) age; B) weight; C) height; D) BMI percentile. Log HOMA-IR: logarithm of homeostatic model assessment insulin resistance; BMI percentile: body mass index percentile.
Discussion
The combined prevalence of overweight and obesity (66%) of the study population is higher than the prevalence values reported at state and national level for adolescents by the 2012 National Health and Nutrition Survey (29%) 16 and by the 2016 National Health and Nutrition Survey of Medio Camino (36%). 22 This fact is highly relevant when considering that the prevalence found is close to that reported in Mexican adults (72%). 22 Finding such high values in early ages lead to infer early development of complications such as atherosclerosis and type 2 diabetes mellitus, the two diseases of greatest concern in Mexico. 23
The glucose and insulin values found showed homogeneity between sexes. Glucose concentration (80.5±8.4 mg/dL) coincides with previous studies conducted on adolescents in the states of Chiapas (85.8±11.8) and Coahuila (73.2±8.7) 17,24, while insulin levels 7.7 (4.8-15.02) μU/mL and HOMA-IR 1.6 (0.90-3.06) are below what has been reported in those two states(13.0±7.9y 13.2±10.5 μU/mL, and2.3±1.4 and 2.9±2.5, respectively).
Even though the populations studied in Tuxtla Gutiérrez, Coahuila and Tapachula are mestizo, they have a different food culture. Consequently, insulin concentrations and HOMA-IR values of the former are probably higher because insulin levels become a compensatory mechanism for high glucose levels after consuming foods with high sugar content. 25
On the other hand, the correlation of HOMA-IR with the BMI percentile (r=0.198; p=0.037) found in this study is lower than that reported with anthropometric parameters in adolescents from Jalisco, Mexico (BMI: r=0.27; p<0.001), Brazil (BMI: r=0.366; p=0.031) and Chile (BMI: r=0.327; pO.0001). (26-28)According to the body weight analysis, the overweight and obese group had higher insulin and HOMA-IR levels than the normal weight group (p=0.010 and p=0.015), trend that has been reported in adolescents from Peru and Venezuela. 29,30
For several years, IR has been described as a high impact factor for the alteration of the level of triglycerides and HDL cholesterol, lipids closely related to the development of metabolic syndrome in both adult and adolescent population. 31-34
Conclusions
In the study population, the HOMA-IR presented a moderately significant correlation with the increase of the BMI percentile, reason why the present study can serve as evidence to propose the early diagnosis of IR as a preventive measure for the development of diabetes mellitus type 2 and cardiovascular disease in the adolescent population of Chiapas.















