Introduction
Staphylococcus aureus is a widely known microorganism responsible for a wide range of illnesses, from minor skin conditions to invasive infections such as sepsis, as well as toxin-mediated syndromes. Complications such as glomerulonephritis, thrombophlebitis, and pulmonary embolism are less common. 1,2 Although mortality associated with these conditions has decreased, host immunosuppression and antibiotic resistance have favored the emergence of invasive conditions. The prevalence of disseminated disease in children and why their prognosis is better than in adults is still unknown. 3
Two cases of previously healthy patients with disseminated methicillin-sensitive Staphylococcus aureus (MSSA) infection, glomerulonephritis, and thrombosis treated at a pediatric hospital are presented below, as well as a literature review.
Case presentation
Case 1
Mestizo, male patient of 13 years of age, previously healthy, with no relevant history and of urban origin, who was referred after six days of pain in the left ankle without local inflammation, fever of 38.3°C, diarrhea, lower limb edema, oliguria, skin rash and signs of shock. His laboratory results reported leukocytosis (18 700/uL), neutrophilia (89%), creatinine of 1.35 mg/dL, urea nitrogen of 33.3 mg/dl and urinalysis with proteinuria 3+ (equivalent to 300 mg/dL).
On admission, a new blood test was performed under the same clinical conditions, with a similar result: C-reactive protein of 192 mg/dL, ureic nitrogen of 40.5 mg/dL and creatinine of 1.65 mg/dl with glomerular filtration rate of 45 mL/min/m2. The patient was considered to be in septic shock secondary to cellulitis of the lower limb with associated kidney injury, for which Linezolid was started on the first day. Abscess in the leg was ruled out by ultrasound and osteomyelitis was confirmed by bone biopsy.
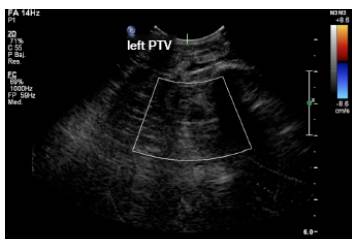
At 48 hours, MSSA was isolated in bone and blood cultures, and antibiotic therapy was redirected to oxacillin 160 mg/kg/day; however, four days after admission, the patient presented with reappearance of fever, increase in lower limb edema and elevation of acute phase reactants with persistent isolation in blood cultures, so the search for the foci of the disseminated infection was initiated. Since deep vein thrombosis in one of the posterior tibial veins was observed in the Doppler ultrasound of the lower limb (Figure 1), anticoagulation with dalteparin was initiated and management with oxacillin continued for 42 days with satisfactory evolution and recovered renal function upon discharge.
Case 2
Mestizo, male patient of 12 years of age, previously healthy, from an urban area and with no relevant history. He was admitted to the emergency department after four days of fever, diarrhea, hematuria and testicular pain, in addition to inflammatory signs on the instep of the left foot. The results of the blood test were as follows: leukocytosis (16 600/uL), neutrophilia (77%), urinalysis with proteinuria (75 mg/dL) and erythrocytes (150 x field); the patien did not show signs of urinary tract infection, and had received unknown outpatient management.
Due to the persistence of the symptoms, the patient consulted the emergency department of the institution due to having fever of 39°C, left testicular pain, erythema, heat, edema and pain in the left foot. Testicular ultrasound reported hydrocele, and blood test reported leukocytosis (13 080/uL), neutrophilia (87%), C-reactive protein at 192 mg/dL, proteinuria at 75 mg/dL, urea nitrogen at 10.6 mg/dL and creatinine of 0.77 mg/dL with preserved glomerular filtration rate. Considering that the patient had cellulitis on his foot, it was empirically managed with clindamycin.
At 72 hours, evolution was torpid. The patient presented with respiratory distress, increased edema in the limb, cough, chest pain, ventilatory failure with need for invasive support, procalcitonin of 1.94 ng/dL and positive blood cultures for MSSA. Therefore, oxacillin therapy (200 mg/kg/day) was initiated and extension studies were performed.
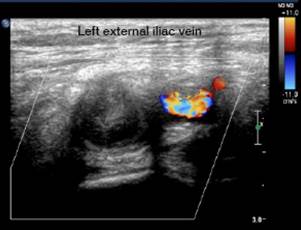
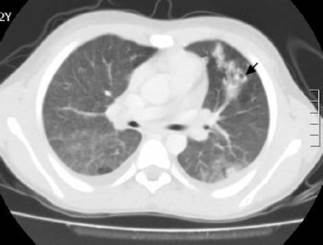
The Doppler ultrasound of the lower limb showed thrombosis of the external iliac and left common femoral veins (Figures 2 and 3). The chest x-ray, performed due to suspicion of septic pulmonary embolism, showed acinar nodule lesions (Figure 4). The CT scan showed pulmonary and subpleural nodules (Figure 5), and a D-dimer value of200-00 ng/dL was determined (reference <200). Consequently, it was confirmed that the patient had venous thromboembolism and septic pulmonary embolism. Echocardiogram and abdominal ultrasound were normal. The treatment with oxacillin was continued and the new blood cultures, taken after five days, were negative. The patient completed 42 days of antibiotic and anticoagulant treatment, and was discharged with satisfactory evolution.
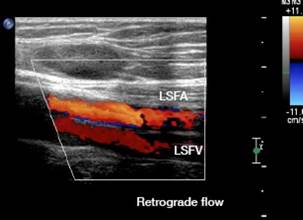
LSFV: left superficial femoral vein; LSFA; left superficial femoral artery. Source: Document obtained during the study.
Figure 2 Doppler ultrasound of the left lower limb: superficial femoral vein thrombosis with retrograde flow.

Source: Document obtained during the study.
Figure 4 Chest x-ray: diffuse parenchymal/alveolar opacities.
Discussion
Although disseminated S. aureus infection has been better described in adults than in children -therefore data in this population are limited-, it is known that it occurs more frequently in children under one year of age. Some studies consider that the incidence of S. aureus bacteremia has not increased; however, at the community level, MSSA has produced more invasive pictures 4, which is consistent with the cases reported in this article. Moreover, McMullan et al.5, in 2016, collected data from other studies and found that community-acquired S. aureus infection is more frequent in males and by MSSA 5, characteristics found in the patients described here.
As observed in one of the cases presented here, osteomyelitis is the most frequent initial focus of disseminated disease, as it is the starting point in 32.4%-62% of patients according to the reviewed series. 5 The incidence of osteomyelitis due to resistant microorganisms has increased since 2000, which explains the initial management used in the cases described here based on the risk of major complications. 6
Other rare manifestations in children are renal failure related to staphylococcemia and septic thrombosis. In 2015, Glassock et al.7 described that staphylococcal glomerulonephritis is directly associated with the septic process, so management is different from post-infectious or immunological glomerulonephritis, that is, antibiotic therapy is the basis of treatment instead of corticoids. In adults, hematuria, proteinuria and self-limited acute renal failure are more frequent 8, although these symptoms were observed in one of the pediatric cases described here.
In previously healthy children with no family history of hypercoagulability, deep vein thrombosis and pulmonary septic embolism are rare and their occurence is more associated with methicillin-resistant S. aureus (MRSA) infection, with an overall incidence of 0.07/10 000 patients presenting with bacteremia, which is higher in individuals with osteomyelitis. 9,10 Skin manifestations of soft tissue infection, osteomyelitis and thrombosis may be similar; therefore, the rate of suspicion should be high when the patient's condition deteriorates. Imaging studies should be used for confirmation 11, which was the case of the two reported patients.
Likewise, in a patient presenting with staphylococcemia with acute respiratory distress, septic pulmonary embolism associated with deep vein thrombosis of the limbs should be suspected, since it may occur in up to 65% of cases. Computerized axial tomography helps to diagnose pulmonary involvement by thromboembolism. 12
Despite the increase in resistant strains, MSSA remains an important etiological agent of disseminated disease, and the treatment of choice involves beta-lactams such as oxacillin. Early treatment has a positive effect on prognosis. First-generation cephalosporins are used as an alternative for spectrum and lower the risks of side effects, but the rate of therapeutic failure in endocarditis and invasive infection is higher 13; consequently, oxacillin remains the first choice, as in the reported cases, which had favorable evolution.
Conclusions
The disease disseminated by MSSA is the result of the great invasion capacity of different tissues of this microorganism. In children, it should borne in mind that complications due to dissemination may be multiple: some are frequent such as cellulitis, osteomyelitis/arthritis and pneumonia, and others are rare such as thromboembolism and glomerulonephritis, which should be suspected when atypical or torpid clinical courses are presented in order to carry out the diagnostic process and early management in search of sources of dissemination and thus improve the prognosis. The role of oxacillin is highlighted as the treatment of choice when the microorganism is sensitive.