Introduction
In Colombia, the Ministry of Health has acknowledged, on the one hand, the impact that malnutrition has on health care and, on the other, the usefulness of nutritional screening to prevent and reduce the prevalence of malnutrition in hospitals.1
The American Dietetic Association defines nutritional screening as the "process of identifying characteristics known to be associated with nutrition problems. Its purpose is to pinpoint individuals who are malnourished or at nutritional risk." 2, p1 With this in mind, screening is considered as an indicator of quality of healthcare services in the hospital setting. 3,4 However, nutritional screening is not routinely applied in pediatric hospitals since there is no accepted screening tool for these patients, leading to an underestimation of hospital malnutrition. 5,6 Currently, malnutrition rates are still considerable in Europe and Canada, as well as in Colombia, with a prevalence in pediatric populations between 7% and 16.6% for acute malnutrition, and 2.5% and 22.4% for chronic malnutrition.7-12
The American Society for Parenteral and Enteral Nutrition defines malnutrition in pediatrics as "an imbalance between nutrient requirements and intake, resulting in cumulative deficits of energy, protein, or micronutrients that may negatively affect growth, development, and other relevant outcomes".13, p19 It should be noted that while malnutrition harms hospitalized patients of all ages,14 children are at greater risk13 since it is associated with inadequate growth and development, poor school performance and possibly having long-lasting impacts in adulthood.15
Colombia currently has evidence of the need to make recommendations on tools that allow, first, to identify pediatric patients with malnutrition or at risk of malnutrition and, second, to do nutritional screening.5 All this becomes relevant taking into account that children are a population that is vulnerable to hospital malnutrition due to their physiological characteristics since they have greater energy requirements due to other processes such as growth, development and the severity of diseases that require hospital admission (acute diarrhea, primary malnutrition, celiac disease, obesity, dyslipidemias, among others). 16,17 Therefore, this research work presents a literature review and comparative analysis of nutritional screening tools used in pediatrics and validated in Europe and Canada to provide a set of guidelines and recommendations to expand their use in Colombian institutions. It also seeks to improve, in the future, healthcare services and manage the prevalence of malnutrition in pediatric hospitals.
In summary, this review aims to find whether the institutional use of nutritional screening tools in pediatrics allows the timely identification of patients with malnutrition or at risk of malnutrition, as well as the timely referral of patients to nutritional therapy.
Materials and methods
The present investigation followed the PRISMA (Preferred Reporting Items for Sistematic Reviews and Meta-analyses) statement, which provides guidelines for conducting systematic reviews and meta-analyses of studies that evaluate health interventions in biomedical sciences. 18
The PICO procedure (patient or problem, intervention, comparison and outcomes) was used to define the research question,19 and also allowed defining the criteria for the selection of the studies.
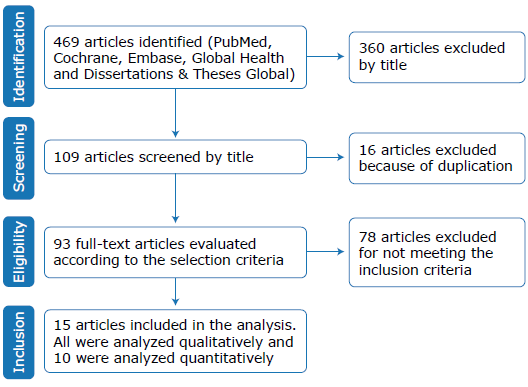
The following types of articles were excluded: 1) those without available full texts; 2) those that were not original researches, that is, letters to the editor, book chapters, systematic reviews, case reports and position papers, and 3) those that evaluated only excess weight and included extensive nutritional assessment parameters (such as biochemical analysis), or that did not employ a method of comparison. In view of the above, and as shown in Figure 1, all original studies in English, French or Spanish published between 2002 and 2017 that validated a nutritional screening tool in Europe or Canada and had a method of comparison were included. The search was carried out in May 2017 on the PubMed, Cochrane, Embase, Global Health and Dissertations & Theses Global databases using the search equation (Nutritional Screening) AND (paediatric OR child) AND malnutrition AND hospital.
The checklist of items from the Cochrane Handbook was used for data extraction.20 First, the screening tools found were analyzed according to the guidelines of the European Society for Clinical Nutrition and Metabolism (ESPEN) 2002,21 which state that the use of these tools should consider 4 variables that impact nutritional risk: current nutritional status, stability, expected progression and influence of the disease. Moreover, it clarifies that the first 3 variables must be part of all the instruments, while the fourth is included depending on the relevance defined by each institution; each one must be assigned a score in order to quantify the degree of risk, thus allowing the choice of the appropriate path to follow according to the categories established in the care protocols.21,22
Regarding methodology, it has been established that the usefulness of screening tools is usually based on the aspects of predictive validity, concurrent validity, reproducibility and practicality.23 For this reason, in this review the statistics issued by the studies that were carried out to validate the screening tools were analyzed; the selected parameters were sensitivity and specificity, contained in concurrent validity and reproducibility, respectively. Concurrent sensitivity was understood as the proportion of individuals at risk of malnutrition correctly identified by the screening tests and concurrent specificity was understood as the proportion of individuals not at risk correctly identified by the nutritional screening tool. Sensitivity and specificity, as well as reproducibility, corresponded to data calculated in each study considering the selected method of comparison.
Finally, the quality of evidence was assessed following the recommendations of the U.S Preventive Services Task Force, a tool developed by the Canadian Task Force on the Periodic Health Examination to evaluate preventive measures and to help researchers extract information from clinical studies in the form of evidence-based medicine recommendations.24,25 To achieve this, the design of the studies analyzed was considered first in order to establish the level of certainty of each study; then, the nutritional screening tools with the same level of certainty were grouped and the degrees of the recommendations were established according to the level of certainty assigned and the net benefit (greater number of benefits over the number of harms) of their use (Table 1).
Table 1 Degrees of recommendation according to level of certainty and net benefit.
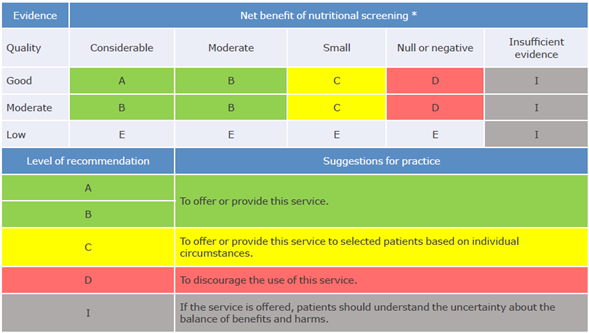
* The net benefit of screening was measured in terms of concurrent validity (sensitivity) and reproducibility. The net benefit was deemed considerable when sensitivity values were >85%, moderate >75% and low >50%. The net benefit was deemed considerable with avalué k>0.81, moderate with k>0.61 and low with k>0.41.
Source: Own elaboration based on Primo.24
Results
Search results
The search yielded 469 articles in the PubMed, Cochrane/ EBM Reviews, Embase, Global Health and Dissertations &Theses Global databases. 360 studies were excluded according to their title, 16 because they were duplicated and 78 for not meeting the selection criteria -32 were conducted outside Canada or Europe, 27 did not evaluate any screening tool, 11 were secondary studies (reviews), 4 included adult patients and 4 were incomplete or in another language. The final sample consisted of 15 studies.
Table 2 compiles and integrates the information from the 15 studies included in the literature review according to the PICO characteristics of the research. 26-40 It should be noted that, although the search included original studies published between 2002 and 2017, the selected articles were released between 2010 and 2017 (67% of them were published between 2012 and 2017), thus indicating that the results are up-to-date. All studies were developed in European countries.
Table 2 PICO characteristics of the included studies.
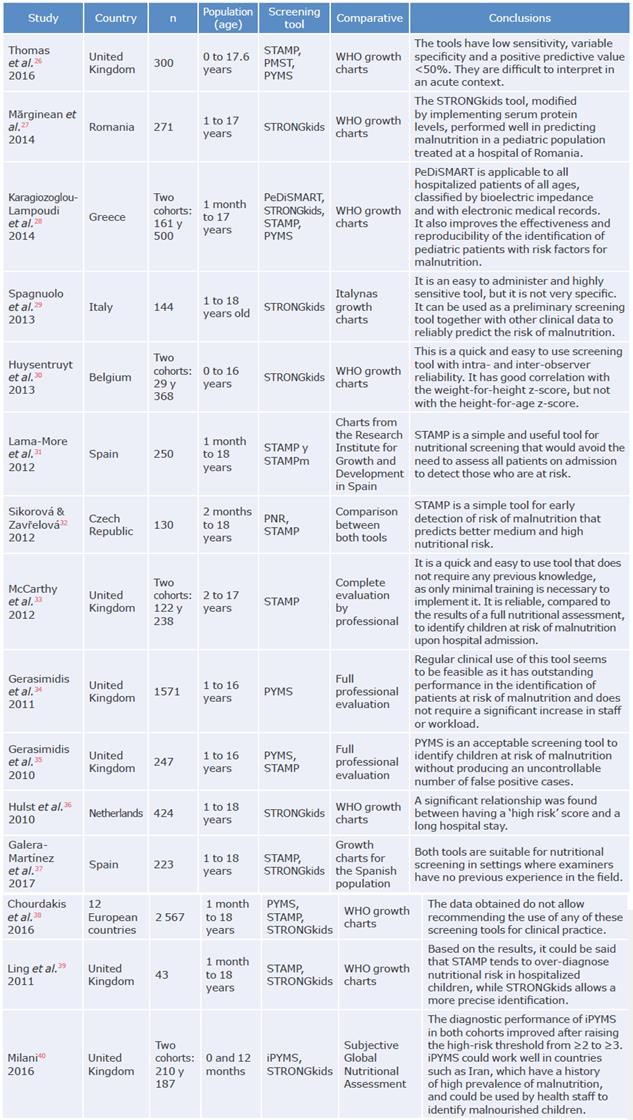
STAMP: Screening Tool for the Assessment of Malnutrition in Paediatrics; STAMPm adaptation of the original STAMP tool, in which the UK growth charts were replaced by the Spanish growth charts; PMST: Paediatric Malnutrition Screening Tool; PYMS: Paediatric Yorkhill Malnutrition Screening; WHO: World Health Organization; STRONGkids: Screening Tool for Risk of Impaired Nutritional Status and Growth; PeDiSMART: Pediatric Digital Scaled Malnutrition Risk Screening Tool; PNR: Paediatric Nutritional Risk; iPYMS: Infant Paediatric Yorkhill Malnutrition Score; TPH: tertiary pediatric hospital; DGH: district general hospital.
Source: Own elaboration.
Description of the identified screening tools
Seven tools have been validated in European countries for the identification of pediatric patients at nutritional risk: Paediatric Yorkhill Malnutrition Screening (PYMS), Infant Paediatric Yorkhill Malnutrition Score (iPYMS), Pediatric Digital Scaled Malnutrition Risk Screening Tool (PeDiSMART), Paediatric Nutritional Risk (PNR), Screening Tool for the Assessment of Malnutrition in Paediatrics (STAMP), Paediatric Malnutrition Screening Tool (PMST) and Screening Tool for Risk of Impaired Nutritional Status and Growth (STRONGkids). All were designed to be used during hospital admission and, except for PNR, have the possibility of being used again after the first week of hospital stay.
Table 3 shows a comparison between the different nutritional screening tools, taking into account the four variables that must be incorporated to correctly identify the nutritional risk of hospitalized patients.21,22
Table 3 Comparison of screening tools according to the European Society for Clinical Nutrition and Metabolism guidelines.
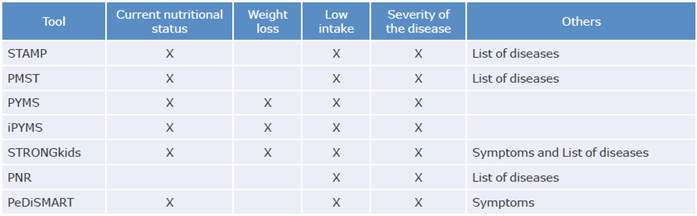
STAMP: Screening Tool for the Assessment of Malnutrition in Paediatrics; PMST: Paediatric Malnutrition Screening Tool; PYMS: Paediatric Yorkhill Malnutrition Screening; iPYMS: Infant Paediatric Yorkhill Malnutrition Score; STRONGkids: Screening Tool for Risk of Impaired Nutritional Status and Growth; PNR: Paediatric Nutritional Risk; PeDiSMART: Pediatric Digital Scaled Malnutrition Risk Screening Tool.
Source: Own elaboration based on Kondrup J et al.21
Concurrent validity and reproducibility
Considering the statistical data extracted from the included studies, concurrent validity and reproducibility were the basis of the analysis of the nutritional screening tools validity since they are commonly found in most studies. This allows comparing most of the identified nutritional screening instruments.
Table 4 presents the included studies that evaluate the concurrent validity of 5 pediatric nutritional screening tools (STAMP, PMST, PYMS, iPYMS and STRONGkids). In turn, Table 5 depicts the studies that included results on concordance among observers where it was considered sufficient for Kappa values >0.41.41
Table 4 Concurrent validity (sensitivity and specificity) of the screening tools.
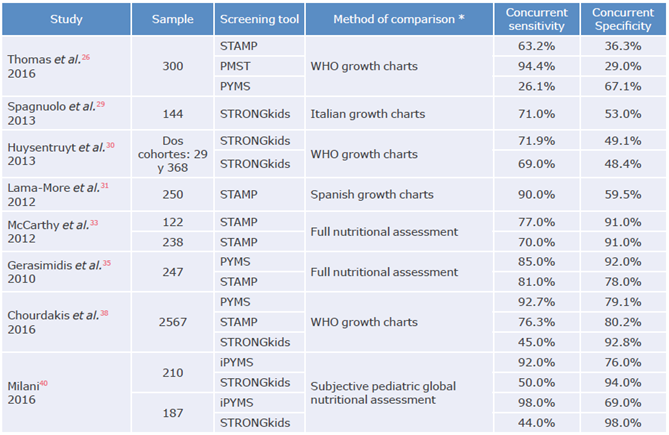
STAMP: Screening Tool for the Assessment of Malnutrition in Paediatrics; PMST: Paediatric Malnutrition Screening Tool; PYMS: Paediatric Yorkhill Malnutrition Screening; STRONGkids: Screening Tool for Risk of Impaired Nutritional Status and Growth; iPYMS: Infant Paediatric Yorkhill Malnutrition Score; WHO: World Health Organization.
* Concurrent validity (sensitivity and specificity) was estimated and extracted from the primary studies.
Source: Own elaboration.
Table 5 Concordance (Kappa) between observers of the screening tools.
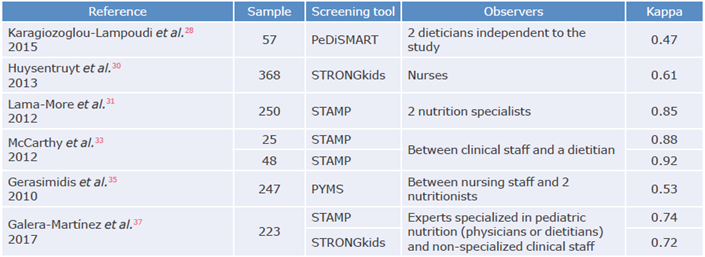
PeDiSMART: Pediatric Digital Scaled Malnutrition Risk Screening Tool; STRONGkids: Screening Tool for Risk of Impaired Nutritional Status and Growth; STAMP: Screening Tool for the Assessment of Malnutrition in Paediatrics; PYMS: Paediatric Yorkhill Malnutrition Screening.
Source: Own elaboration.
Levels of certainty of the studies
The level of certainty was estimated for 67% of the studies, as they included results assessing concurrent validity (in terms of sensitivity and specificity) and reproducibility (in terms of inter-observer agreement). The remaining 33% yielded other results such as predictive validity and intra-rater reliability, which were not analyzed because of the total number of articles with data, time and resources. 27,32,34,36,39
Among the 10 studies for which the level of certainty was calculated, the Chourdakis et al38 study had the highest level of certainty, mainly because it was carried out in 12 countries throughout Europe with a sample of 2 567 patients and because the results were consistent. In contrast, the level of certainty of the study by Thomas et al.,26 which was carried out in the United Kingdom, was considered low, particularly because it was a unicenter research with convenience sampling and inconsistent results. The remaining 8 studies were classified at a moderate level since they were multicenter studies, with randomized, systematized or consecutive sampling and generally consistent results that allow, to some extent, the generalization of findings to clinical practice.28-31,33,35,38,40
Recommendations for the use of nutritional screening tools in pediatrics
Of the seven tools identified in this systematic review, quality assessment was only possible in six of them, namely, PYMS, iPYMS, STAMP, PMST, STRONGkids and PEDISMART. A complete quality analysis -i.e. concurrent validity and reproducibility- was conducted only for the STAMP, PYMS and STRONGkids, while in the case of iPYMS and PMST only concurrent validity was evaluated, and for the PEDISMART tool, only reproducibility was assessed.
The partial evaluation of the PEDISMART, PNR and iPYMS tools does not mean that they are not useful in other contexts or situations; it means that there is no information on the characteristics that were considered of greater relevance in those reviews. Table 6 presents recommendations for the use of validated nutritional screening tools in European children according to concurrent validity and reproducibility characteristics.
Table 6 Recommendation for the use of screening tools.
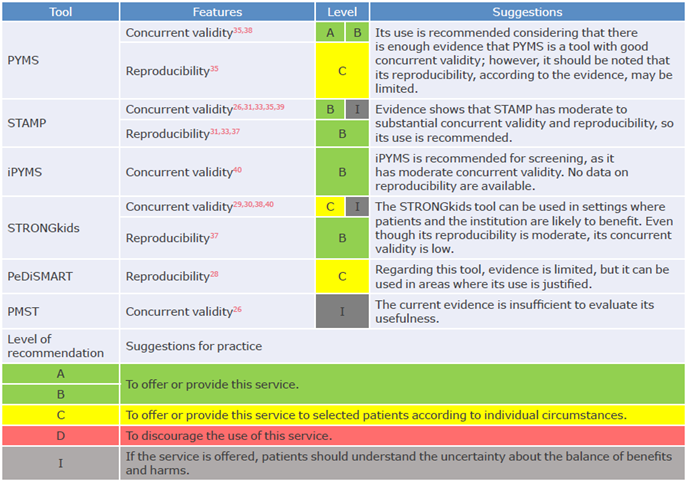
PYMS: Paediatric Yorkhill Malnutrition Screening; STAMP: Screening Tool for the Assessment of Malnutrition in Paediatrics; iPYMS: Infant Paediatric Yorkhill Malnutrition Score; STRONGkids: Screening Tool for Risk of Impaired Nutritional Status and Growth; PeDiSMART: Pediatric Digital Scaled Malnutrition Risk Screening Tool; PMST: Paediatric Malnutrition Screening Tool.
Source: Own elaboration based on the information of the U.S. Preventive Services Task Force. 25
Discussion
Description of the identified screening tools
Based on the ESPEN guidelines described in Table 3, only the PYMS tool for screening patients between 1 and 16 years of age hospitalized in floors and surgical areas, the iPYMS for the same type of population but under 2 years of age, and the STRONGkids for the same type of population with ages between 1 month and 18 years of age, evaluate all the variables that are considered to have a nutritional impact. To this end, they assess current nutritional status, weight loss, reduced intake and severity of disease (Table 2). (21
Thus, the PYMS, iPYMS and STRONGkids tools can be considered as the most suitable tools for nutritional screening. However, these are not the only criteria that must be considered to state that a tool is appropriate since any screening tool can be used to identify children with or at risk of malnutrition, as long as the results translate into early intervention and improved clinical outcomes.
Concurrent validity and reproducibility
Nutritional screening is a tool that is classified into the same category of diagnostic tests, which means that it is an instrument that allows obtaining additional information about a patient in order to adequately define the care plan to be followed. 42 Moreover, the use of nutritional screening tools is relevant for care centers since their routine use allows the optimization of economic and human resources and the reduction of costs derived from hospital malnutrition. 21,43 In this sense, and given that a highly sensitive tool is designed to correctly detect a greater proportion of patients at real nutritional risk -i.e. those who require greater monitoring of their nutritional status-, the most important statistic is sensitivity. 44
Although the screening tools were validated using different reference methods (Table 2), if sensitivity (ability to detect true positives) >85% is considered as acceptable, the PYMS, iPYMS and PMST tools may be the best options for screening, followed by STAMP with adequate but less consistent sensitivity according to the studies analyzed. However, if good specificity (ability to detect true negatives) is also considered as a desirable characteristic, only the PYMS tool meets these two characteristics of concurrent validity. 35,39
It should be noted that these results are not consistent across studies, 26 partly because sensitivity and specificity tend to be inversely related. 45 In this regard, the meta-analysis by Huysentruyt et al.,46 by including gold standards to validate the tools, shows that there is a marked variation among the studies included. Consequently, in order to have more consistent results, it is necessary to establish a gold standard to assess sensitivity and specificity and to obtain results with greater comparability between studies.
Reproducibility was also assessed, as good agreement between raters in a nutritional screening tool is desirable. The results showed that the PeDiSMART, STRONGkids, STAMP, and PYMS tools have acceptable inter-observer agreement when assessing reproducibility across a broad spectrum of health professionals (Table 5). This is relevant given that a good nutritional screening tool should require little training of clinical staff to complete the instrument and should be quick to use and interpret thanks to a simple scoring system. 23
Recommendations for use
Table 6 presents recommendations for the use of the PYMS, STAMP, iPYMS, STRONGkids, PeDiSMART and PMST tools according to desirable characteristics such as concurrent validity and reproducibility. Nevertheless, it should be remembered that these are not the only characteristics to consider; ease of use, the time required, and predictive validity should also be considered, 23 although that was not the case of this paper due to the limited information available. Even so, it is expected that the results reported here will help health staff choose the best option for nutritional screening in pediatrics from the tools available for implementation in institutional protocols.
The present review is limited by geographical demarcation to only Canada and Europe, so this work should be complementary to other reviews carried out outside the proposed context. 22,47 Another limitation is that this study focuses on screening tools that determine the risk of malnutrition; however, these tools can be modified (especially the current nutritional status variable) to detect overweight, which can also have negative consequences in hospitalized children.
On the other hand, although the quality of the included studies was evaluated, bearing in mind that this review aims to summarize the available evidence, it is not exempt from the systematic errors of the designs of the original studies; therefore, the work was carried out according to the PRISMA statement to include all the available studies and minimize selection bias. 48,49 Finally, due to the lack of international consensus on the definition of malnutrition, there is no standard reference for assessing the validity of nutritional screening tools with the same method; this makes the results of the tools closely linked to the classification of malnutrition in each study. Therefore, once a universal diagnosis for malnutrition is established, it is expected that tool validation studies will yield more consistent results.
Conclusions
Currently, in Colombia there are no recommendations on the use of nutritional screening tools in pediatrics due to the lack of consensus on which is the most appropriate tool to be used in this population, especially considering the difficulties for their possible validation and comparison. The studies included here demonstrated that, with respect to concurrent validity and reproducibility, the PYMS, iPYMS and STAMP tools offer greater certainty and net benefit; however, based on the findings of this review, PYMS could be used in clinical practice, while each institution should make an assessment to consider the use of STAMP and iPYMS.