Introduction
Bile duct diseases are highly prevalent worldwide and may be asymptomatic or turn into neoplasms with poor prognosis. Some studies report that one of the most common disorders is cholelithiasis, which affects up to 20% of the world population1 and 15% of the inhabitants of Europe and North America. Symptoms may worsen by the presence of cholangitis or pancreatitis, 3 so a large number of people with these conditions require some surgical procedure, either for diagnostic or therapeutic purposes. The bile ducts can also be affected by injury or iatrogeny, which can be simple or complex with destruction of the bile duct wall.5
The increase in the population's health coverage has made it possible to identify a greater amount of people with biliary diseases. To achieve this, it has been necessary to explore the anatomical features of the bile duct by means of endoscopic sphincterotomy, endoscopic retrograde cholangiopancreatography (ERCP), intraoperative cholangiography, laparoscopic or open cholecystectomy, clinical assessment and liver function tests. 7
Nowadays, bile duct surgeries, with their different modalities, are essential procedures to guarantee the adequate state of health of the people. In addition, echoendoscopy allows obtaining better gallbladder cancer diagnoses.8,9 Although this type of surgical procedure has been perfected, complications during surgery remain a concern for surgeons. The most frequent causes of these adverse events are the lack of expertise of the surgeon and the failure to perform a careful procedure; 10,11 however, the presence of anatomical variations unbeknownst to professionals also plays an important role for their occurrence.
The most common setbacks in bile duct surgery are bleeding, infection and injury to the bile ducts, which occur because anatomical variations are unknown. In Colombia, Ramos-Pachón et al.12 conducted a follow-up study of patients with biliopancreatic diseases, finding that surgical complications occurred in 7.43% of ERCPs, the most frequent being acute cholangitis (3.34%), with mortality of 1.86%. In Latin America, there is little reported research explaining the features and anatomical variations of the bile ducts and, particularly, in Colombia there are no published studies regarding these variations.
Therefore, the aim of this research was to carry out a study on the features and possible anatomical variations of the bile ducts in the Colombian population. This characterization will allow morphologists, surgeons, radiologists and other medical specialists to have a better understanding of the possible biliary variations and their classifications, to analyze their morphometry and to contribute to the decrease of surgical complications derived from the lack of knowledge. This characterization will also allow a better interpretation in cases where such variations are present.
Materials and methods
A descriptive analytical cross-sectional study was conducted on 60 human gastrointestinal tracts comprising the liver, extrahepatic bile ducts, pancreas, and small and large intestines. The tracts were taken from corpses available at the amphitheater of the Medical program offered by the Universidad de Ciencias Aplicadas y Ambientales - U.D.C.A.; specimens that did not have any disease or previous surgeries of the bile ducts were included.
The bile ducts were dissected from the cadavers as follows: the gender of each body was established by identifying the ovaries and uterus in women or the prostate and testicles in men; the bile ducts in the gastrointestinal tract were identified and the peritoneum and omentum were removed; then, the distal intrahepatic bile ducts were dissected, along with a fraction of the liver, as well as the extrahepatic ducts, which were measured to obtain their length and caliber; finally, the anatomical features were described and a photographic record was taken.
The information obtained was analyzed and recorded in the Microsoft Excel 2013 program, and the statistical data was processed in the SPSS program, version 21, using the classification proposed by Blumgart as a parameter13 (Figure 1).
A: usual confluence; B: triple confluence; CI: right anterior duct draining into RHD; C2: right posterior duct draining into the RHD; Dl : right posterior duct draining into the LHD; D2: right anterior duct draining into the LHD; El and E2: absence of hepatic duct confluence; F: drainage of the right posterior duct into the cystic duct and absence of RHD. Ih: left hepatic; ra: right anterior; rp: right posterior, RHD: right hepatic duct; LHD: left hepatic duct; CHD: common hepatic duct; I, II, III and IV: segmental ducts. Source: Own elaboration based on Hahn & Blumgart.13
Figure 1 Main variations of the hepatic duct confluence according to Blumgart.
For the present study, the information was obtained based on the regulations for performing a medico-legal necropsy contained in Decree 786 of 1990 of the Colombian Ministry of Public Health.14 Likewise, the principles contained in the Declaration of Helsinki15 for treating the information derived from cadavers were followed, guaranteeing the confidentiality of the data of the deceased patient, his or her dignity and integrity. The regulations of Resolution 8430 of 1993 of the Colombian Ministry of Social Protection and Health were applied.16 Similarly, this research was submitted for approval by the Ethics Committee of the Faculty of Health Sciences of the U.D.C.A., through unnumbered minutes of November 28, 2017.
Results
60 gastrointestinal tracts were analyzed, of which 4 corresponded to women and 56 to men. They were classified according to Blumgart13 (Table 1 and Figures 2, 3 y 4).
Table 1 Frequency of bile duct variations according to Blumgart in a sample of cadaveric specimens in Colombia.
| Type | A | B | C1 | C2 | D1 | D2 | E1 | E2 | F |
| Cases | 44M+3F=47 | 3M | 0 | 2M | 0 | 1M | 1M | 4M+1F=5 | 1M |
| % | 78.3 | 5 | 0 | 3.3 | 0 | 1.7 | 1.7 | 8.3 | 1.7 |
A: usual confluence; B: triple confluence; C1 : right anterior duct draining into RHD; C2: right posterior duct draining into the RHD; D1: right posterior duct draining into the LHD; D2: right anterior duct draining into the LHD; E1 and E2: absence of hepatic duct confluence; F: drainage of the right posterior duct into the cystic duct and absence of RHD; M: Male, F: Female; CHC: common hepatic duct; LHD: left hepatic duct; RHD: right hepatic duct.
Source: Own elaboration.
GB: gallbladder; ra-RHD: right anterior branch of the right hepatic duct; rp-RHD: right posterior branch of the right hepatic duct; CA: cystic artery; CD: cystic duct; BD: bile duct; LHD: left hepatic duct; CHC: common hepatic duct; LHA: left hepatic artery; RHA: right hepatic artery Source: Document obtained during the study.
Figure 2 Hepatic duct type C2.
ra-RHD: right anterior branch of the right hepatic duct; rp-RHD: right posterior branch of the right hepatic duct; GB: gallbladder; CA: cystic artery; CD: cystic duct; I, II, III and IV: segmental ducts; CHC: common hepatic duct; BD: bile duct. Source: Document obtained during the study.
Figure 3 Hepatic duct type E2.
GB: gallbladder; ACC: anterior cystic duct; PCC: posterior cystic duct; CC: cystic conduct; rp-RHD: right posterior branch of the right hepatic duct; ra-RHD: right anterior branch of the right hepatic duct; LHD: left hepatic duct; BD: bile duct. Source: Document obtained during the study.
Figure 4 Hepatic duct type F.
With regard to the path of the bile ducts, four portions were found in all gastrointestinal tracts:
A supraduodenal portion extending from the formation of the common hepatic duct to the crossing behind the first portion of the duodenum.
A retroduodenal portion extending behind the first portion of the duodenum and separating from the portal vein, which was pulled to the left of the bile ducts after being divided. This portion had two anatomical relationships: one through its back side with the inferior cava vein, from which it was separated by the retroduodenal fascia, and another through the left side with the retroduodenal artery.
A retropancreatic portion crossing the lower border of the duodenum was located behind the head of the pancreas; it then followed a downward path to the right, and ended up on the anterior/internal part of the second portion of the duodenum, in conjunction with the main pancreatic duct.
An intramural portion leading to the major duodenal ampulla.
It is worth noting that the three first portions had an anatomical relationship, through their back side, with the inferior cava vein.
The features of each duct analyzed are described below (Table 2).
The right hepatic duct was measured in only 47 gastrointestinal tracts since it did not form in the remaining tracts due to their anatomy. The length varied between 3.1mm and 18.5mm, with an average of 10.64mm; it was ≤9.05mm in 25% of the samples. The diameter varied between 2.1mm and 5.9mm with an average of 3.62mm, and ≤3.2mm in 25% of the samples.
The left hepatic duct was measured in 54 gastrointestinal tracts, since it did not form in the remaining tracts due to their anatomy. The length varied between 3.2mm and 35.1mm, with an average of 10.74mm, being ≤8.85mm in 25% of the samples. As for the diameter, it varied between 2.4mm and 5.5mm, with an average of 3.66mm, being ≤3.2 in 25% of the samples.
The length of the common hepatic duct varied between 5mm and 58.5mm, with an average of 25.59mm, being ≤16mm in 25% of the samples. Its diameter varied between 3.7mm and 7.9mm, with an average of 4.9mm, being ≤4.3mm in 25% of the samples.
The length of the bile duct varied between 11.9mm and 81mm, with an average of 38.58mm, being ≤32.25mm in 25% of the samples. Regarding the diameter, it varied between 3.5mm and 6.0mm, with an average of 4.79, being 4.3mm in 25% of the sample.
Discussion
According to Blumgart's classification, type A duct was the most common (78.3%) in the present study, which coincides with the findings by Hribernik et al.17 (82%) and Cova & Louis18 (78.7%); in contrast, type A was less frequent in the study by Tolino et al.19 (41%). The second most common variation in this study was duct type E2, which differs from what was reported by Cova & Louis,18 where type B was the second most common. Furthermore, the prevalence of type A found here is higher than that described by Al-Jiffry20 (57%) and Brunicardi et al.21 (59%), with type C1 duct being the second most frequent in these two studies.
On the other hand, Chaib et al.,22 who used a different classification (type A1, A2, A3 and A4 for right hepatic ducts and B1, B2, B3, B4 and B5 for left hepatic ducts) reported a frequency of 61.3% and 76.2% for types A1 and B1, respectively (which would correspond to Blumgart's type A), and 14.5% and 15% for A2 and B2, respectively (which would correspond to Blumgart's type B). This means that the prevalence of type A is >60% and coincides with the results of the present study and most of the literature on the subject (Table 3).
Table 3 Reported bile duct variations.
| Study | Cases | Type A | Type B | Type C1 | Type C2 | Type D1 | Type D2 | Type E1 | Type E2 | Type F | Country |
| Cova & Louis18 2015 | 232 ERCP | 78.9 % | 10.77% | 7.75% | 0.862% | 0.862% | 0 | 0 | 0.43% | 0 | Venezuela |
| Tolino et al. 19 2010 | 690 ERCP | 41.16% | 25.8% | 15.94% | 5.51% | 1.16% | 3.33% | 2.6% | 3.9% | 0.58% | Argentina |
| Al-Jiffry20 2015 | 117 ERCP | 59% | 10.70% | 11.3% | 6.7% | 4% | 2.2% | 2.7% | 0 | 1.1% | Saudi Arabia |
| Brucardi et al. 21 2015 | No reported number | 57% | 12% | 16% | 4% | 5% | 1% | 2% | 1% | 2% | United States |
| Quijano (present study) 2019 | 60 gastrointestinal tracts | 78.3% | 5% | 0 | 3.3% | 0 | 1.7% | 1.7% | 8.3% | 1.7% | Colombia |
ERCP: endoscopic retrograde cholangiopancreatography.
Source: Own elaboration.
The F-type variation, one of the less frequent in this study and in the existing literature, has a higher risk of being injured during cholecystectomy due to the proximity to the cystic duct outlet.
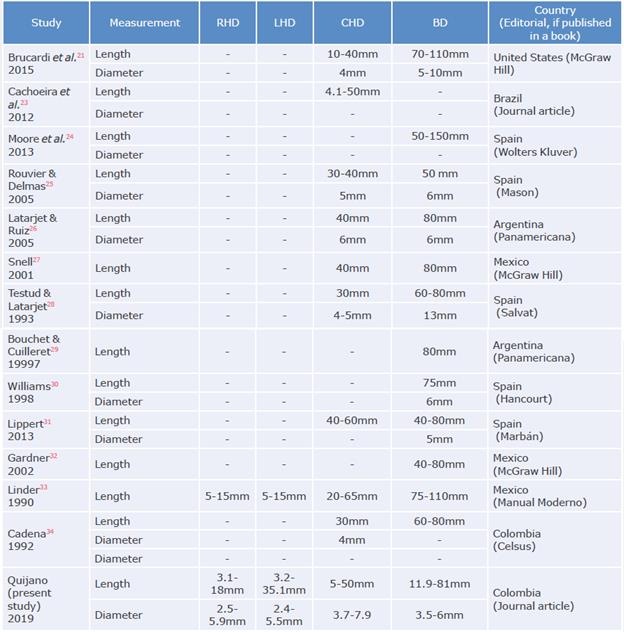
No studies on the length and diameters of the bile ducts are reported in Colombia, but similar averages are reported worldwide and are consistent with the bile duct paths of most of the data recorded in anatomy and surgical texts. However, some books do not measure or describe the dimensions of all ducts 23-34 (Table 4).
Conclusions
The usual anatomy of the bile ducts was observed in 78.3% of the cases; anatomical variations were frequent (21.7%). This prevalence should encourage morphologists, forensic scientists and surgeons to consider the variants during the study and management of biliary diseases in order to prevent complications and injuries.
The length, diameter, features and path of the extrahepatic bile ducts analyzed were within the average reported in the existing literature.