Introduction
Cutting is a behavior in which the patient injures his own body with a cutting object to relieve a negative feeling or cognitive state, resolve an interpersonal difficulty, or induce a state of positive feelings. This practice is one of the nonsuicidal self-injurious behaviors1 that were first considered in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).2
Cutting injuries usually do not lead to fatal outcomes. However, this behavior can be a risk factor for developing suicidal behaviors,3-5 especially if the number of episodes is greater than 20, if 3 or more self-injury methods are used, and if there is a reported absence of pain and feelings of emotional relief immediately after the injury.6
In children and adolescents, the most common self-injuries are cuts, followed by scratches and blows.7 Their distribution in the body varies according to age. In school children, they are more frequent in the face, chest, and genitals, while in adolescents, they predominate in the upper limbs.7 This practice is considered a consequence of attempted dysfunctional emotional regulation driven by poor inhibitory control and disproportionate responses. Moreover, cutting is associated with other psychiatric disorders, borderline personality disorder being the most often described.8
In a study on adolescents, Swannell et al.9found four factors that may be associated with nonsuicidal self-injury, namely, emotion regulation, self-punishment, attention-seeking, and thrill-seeking. Thus, the identified underlying mechanisms include negative reinforcement (through the reduction of emotional distress), positive reinforcement (through the increase of endorphins and attention to the environment), and modeling (through social contagion).9
The incidence and prevalence of cutting have not been described in developing countries such as Colombia, since health professionals do not recognize it usually as a risk behavior, resulting in low diagnostic suspicion.10 In this regard, Albores-Gallo et al.11 state that only between 13% and 21% of patients go to the hospital to seek care for this reason, and only 27% of health workers ask the patient about this behavior. In developed countries, it has been found that the prevalence in adolescents can vary from 10% to 23.2%,3,12-14 and this condition is more common in females (up to 4 times more)10 and is often associated with depressive disorder.7
Estimates are that by 2020 between 15 and 30 million young people worldwide will be engaged in self-harming behaviors, which is equivalent to 3% of the disease burden on young people aged 10-19. These figures would overcome pathologies such as asthma, tuberculosis. and acquired immunodeficiency syndrome, and the cutting scenario would be comparable to the use of psychoactive substances and the disease burden produced by physical violence.11 Some studies have established that between 6% and 8% of adolescents and young adults have any of these behaviors, and that frequency has increased by at least 20% in adolescents between 11 and 19 years of age.5 Self-injurious behavior is rare in the pediatric age, especially in children under 12, and the literature on this subject is scarce.
Risk factors for cutting are diverse and include the presence of a mixed state of depression and anxiety (Hazard Ratio (HR) 3.7; 95%CI: 2.4-5. 9), alcohol use (HR 2.1; 95%CI 1.2-3.7), smoking (HR 1.8; 95%CI 1.0-3.1), cannabis use (HR 2.4; 95%CI 1.4-4.4) and antisocial behavior (HR 1.9; 95%CI 1.1-3.4).7 On the other hand, the onset of this practice has been associated with characteristics such as impulsivity,14 low self-esteem,15 a history of domestic abuse1 and a history of family members attempting suicide.16
The study by Ulloa-Flores et al.,1 conducted on a sample of 556 adolescents who attended a child psychiatric hospital between 2005 and 2011 in Mexico, found that the predominant characteristics were being female, having a low socioeconomic level, suffering from domestic violence, and having a history of sexual abuse; it should be noted that this population has similar social characteristics to those of Colombia.1
Although the reporting of self-injurious behavior in youth and adolescents is increasingly common, information on behaviors specifically classified as cutting and its characteristics in the pediatric age is scarce. This knowledge gap, which has been reported in other countries,17 is also evident in Colombia, where there are no studies on the prevalence of this behavior in pediatric population.
Considering the urgent need to identify and provide care for patients who self-injure, this study aimed to describe the sociodemographic and clinical characteristics and risk factors of the pediatric population with a diagnosis of cutting treated at a quaternary care center in Bogotá D.C., Colombia, between 2011 and 2017.
Materials and methods
Population and sample
A search for cutting diagnosis was performed on the medical records of patients under 15 years of age (age limit for pediatric care at the study institution) treated between January 2011 (the year since when the electronic medical records are available at the study institution) and December 2017 at the emergency department of a quaternary care hospital in Bogotá D.C. To retrieve these records, the diagnostic codes of the following diseases were screened according to the tenth edition of the International Classification of Diseases (ICD-10):18 personal history of self-harm (Z91.5); major depressive disorder, single episode (F32); major depressive disorder, recurrent (f33); mental disorder, not otherwise specified (F99); other psychoactive substance related disorders (F19); other anxiety disorders (F41); adjustment disorders (F43.2); sexual abuse, confirmed (T742); and intentional self-poisoning by and exposure to nonopioid analgesics, antipyretics and antirheumatics (X60).
Medical records that met the inclusion criteria, i.e., the criteria for nonsuicidal self-injury as defined in the DSM-5, were analyzed:2
1. Nonsuicidal self-injury in the past year, for at least 5 days, that caused bleeding, bruising, or mild to moderate physical pain and damage.
2. Self-injury associated with at least two of the following:
Negative thoughts or feelings (depression, anxiety, tension, anger, generalized grief, or self-criticism) in the period immediately preceding a self-injurious act.
Inevitable feelings of concern about the act to be performed just before engaging in the self-injurious act.
Frequent urge to self-injure.
Performance of self-injury with a purpose: relief of a negative cognitive feeling/state or interpersonal difficulty, or induction of a positive emotional state. The patient predicts that this will occur, either during or shortly after the act.
3. The self-injurious behavior and its consequences caused clinically significant distress or functional impairment in the interpersonal, academic areas, among others.
4. The behavior did not occur exclusively during states of psychosis, delirium or intoxication and it cannot be accounted for by another mental or medical disorder.
For each case, information about the following aspects was obtained:
Characterization of the event diagnosed in the emergency department according to the assessment made in the psychiatry service and reported in the medical records of the patients: Was it a suicide attempt?; did the patient express suicidal thoughts, feelings of satisfaction and reduced anxiety after the injury?; what was the main injured body part?; was cutting the reason for consultation?; was hospitalization required?; was it necessary to discharge the patient with follow-up by the psychology and/or psychiatry service?
Personal details and history: age, sex, personal and family history of psychiatric illness, family history of attempted suicide or suicide, and history of use of psychoactive substances and/or alcohol; history of sexual, physical, or psychological violence; and follow-up by the psychology and/or psychiatry service.
Social characteristics: health care system scheme, level of schooling, academic performance, history of domestic violence, family composition, leisure activities and notification to the ICBF (Colombian Family Welfare Institute) during emergency care of the child's self-injury.
Analysis
A descriptive analysis of the data was performed using the STATA V.13 software. The variables of interest were analyzed according to their nature: measures of absolute and relative frequency were used for qualitative variables, while measures of central tendency and dispersion were used for the quantitative variables according to the distribution of normality of the data. Prevalence was calculated per interest group: the pediatric population in general and the pediatric population with a history of psychiatric disorder. All data were presented with 95% confidence intervals.
Ethical considerations
This study followed the principles established by the Declaration of Helsinki for research on human beings.19 Furthermore, according to resolution 8430 of 1993 of the Colombian Ministry of Health,20 this was a risk-free research because no intervention was made on the biological, psychological, or social variables of the target population. Likewise, the study was approved by the Ethics Committee of Fundación Universitaria Sanitas, according to Act No. 014-18 of April 24, 2018.
Results
Between 2011 and 2017, 54 622 patients were treated at the pediatric emergency department of the healthcare institution included in the study. The medical records were screened according to the selection criteria, and 85 were finally selected since they contained information of interest for the study.
The sample consisted of 22 boys and 63 girls under 15 years of age (range 10-14 years). The prevalences of cutting in the study population and in the subgroup with a history of psychiatric disorder were 0.15% (95%CI:0.1-0.2) and 26.7% (95%CI:21.9-31.6), respectively. 95.2% (n=81) of the patients were students and 30.6% (n=26) had low school performance (Table 1).
Table 1 Sociodemographic characteristics of the study population.
| Socio-demographic characteristics | Total n=85 | Female n=63 | Male n=22 | |||||
| n (%) | 95%CI | n (%) | 95%CI | n (%) | 95%CI | |||
| Insurance regime | Contributive | 78 (91.7) | 85.9-97.6 | 56 (88.9) | 78.4-95.4 | 22 (100) | 18.6-39.5 | |
| Subsidized | 1 (1.2) | 00-3.5 | 1 (1.6) | 0.04-8.5 | 0 (0) | 00 | ||
| Prepaid medicine | 6 (7) | 1.6-12.5 | 6 (9.5) | 3.6-19.6 | 0 (0) | 00 | ||
| Currently | Yes | 81 (95.2) | 3.2-15.6 | 61 (96.8) | 78.8-100 | 20 (90.9) | 92.5-100 | |
| attending school | No | 4(4.8) | 0.2-9.2 | 2(3.2) | 00-7.5 | 2(9.1) | 00-21.1 | |
| Low | 26 (30.6) | 20.8-40.4 | 15 (24.9) * | 14.4-37.2 | 11 (55) * | 31.5-76.9 | ||
| Academic performance | Regular | 14(16.4) | 8.6-24.4 | 11 (18) * | 8.1-26.8 | 3 (15) * | 00-28 | |
| Good | 10 (11.7) | 4.9-18.6 | 6(9.8)* | 2.3-16.8 | 4 (20) * | 2.1-34.3 | ||
| Excellent | 2(2.3) | 00-5.6 | 2(3.2)* | 00-7.5 | 0 (0) * | 0 | ||
| No information | 29 (35.8) | 25.4-47.2 | 27 (44.2) * | 31.5-77.5 | 2 (10) * | 1.2-31.7 | ||
| Report to the | Yes | 23(27) | 17.6-36.5 | 18 (28.6) | 18.9-41.3 | 5 (22.7) | 7.8-45.3 | |
| ICBFt | No | 62(73) | 63.5-82.4 | 45 (71.4) | 58.6-82 | 17 (77.3) | 54.6-92.1 | |
* These values correspond to calculations made on the sample currently attending school (n=81).
† Notice to the Colombian Institute of Family Welfare about the child’s self-injury during treatment at the emergency department.
Source: Own elaboration.
52.9% of the patients had a history of psychiatric illness (63.6% of boys and 49.2% of girls). The most common disorder was major depression (15.2%), followed by moderate depression (7.1%), anxiety disorder (7.1%), conduct disorder (5.9%), adjustment disorder (4.7%), attention deficit hyperactivity disorder (3.5%), mild depression (3.5%), substance abuse (2.3%), bipolar affective disorder (2.3%), eating disorder (1.2%) and oppositional defiant disorder (1.2%) (Table 2). 11.8% of the cases used some type of psychoactive substance (22.7% of boys and 7.9% of girls), with marijuana being the most common in both sexes. As for alcohol consumption, there were no significant findings.
On the other hand, it was found that 25.8% of the patients had been victims of psychological violence, with no significant difference in terms of sex. This category included abuse by the family unit and bullying by peers (Table 2).
Table 2 Clinical features of the study population.
| Clinical features | Total n=85 | Female n=63 | Male n = 22 | ||||
| n (%) | 95%CI | n (%) | 95%CI | n (%) | 95%CI | ||
| History of psychiatric illness | Yes | 45 (52.9) | 42.3-63.6 | 31 (49.2) | 36.9-61.6 | 14 (63.6) | 43.5-83.7 |
| No | 34 (40) | 29.6-50.4 | 27 (42.8) | 30.6-55.1 | 7 (31.8) | 12.4-51.3 | |
| No data | 6(7.1) | 1.6-12.5 | 5(7.9) | 1.3-14.6 | 1 (4.5) | 00-13.2 | |
| Type of psychiatric illness * | Major depression | 13 (15.2) | 7.6-22.9 | 8 (12.6) | 4.5-20.9 | 5 (22.7) | 5.2-40.2 |
| Moderate depression | 6(7.1) | 1.6-12.5 | 3 (4.8) | 00-10 | 3 (13.6) | 00-28 | |
| Anxiety disorder | 6(7.1) | 1.6-12.5 | 4(6.3) | 0.3-12.4 | 2 (9) | 00-21.1 | |
| Conduct disorder | 5(5.9) | 0.9-10.9 | 5(7.9) | 1.3-14.6 | 0 (0) | 00 | |
| Adjustment disorder | 4(4.7) | 0.2-9.2 | 3(4.8) | 00-10 | 1 (4.5) | 00-13.2 | |
| ADHD | 3(3.5) | 00-7.5 | 1 (1.6) | 00-4.7 | 2 (9) | 00-21.1 | |
| Mild depression | 3(3.5) | 00-7.5 | 3(4.8) | 00-10 | 0 (0) | 00 | |
| Use of psychoactive drugs | 2(2.3) | 00-5.6 | 1 (1.6) | 00-4.7 | 1 (4.5) | 00-13.2 | |
| Bipolar affective disorder | 2(2.3) | 00-5.6 | 1 (1.6) | 00-4.7 | 1 (4.5) | 00-13.2 | |
| Eating disorder | 1 (1.2) | 00-3.5 | 1 (1.6) | 00-4.7 | 0 (0) | 00 | |
| Oppositional defiant disorder | 1 (1.2) | 00-3.5 | 1 (1.6) | 00-4.7 | 0 (0) | 00 | |
| Occasional use of psychoactive drugs | Yes | 10 (11.8) | 4.9-18.6 | 5 (7.9) | 1.3-14.6 | 5 (22.7) | 5.2-40.2 |
| No | 27 (31.8) | 21.9-41.7 | 20 (31.7) | 20.3-43.2 | 7 (31.8) | 12.4-51.3 | |
| No data | 48 (56.4) | 45.9-67 | 38 (60.3) | 48.2-72.4 | 10 (45.4) | 24.6-66.3 | |
| Alcohol consumption | Yes | 8 (9.4) | 3.2-15.6 | 5(7.9) | 1.3-14.6 | 3 (13.6) | 00-28 |
| No | 4(4.7) | 0.2-9.2 | 3(4.7) | 0.5-10 | 1 (4.5) | 00-13.2 | |
| No data | 73 (85.8) | 78.5-93.3 | 55 (87.3) | 79.1-95.5 | 18 (81.8) | 65.7-97.9 | |
| Victim of sexual violence | Yes | 9 (10.6) | 4-17.1 | 7 (11.1) | 3.4-18.9 | 2 (9) | 00-21.1 |
| No | 8 (9.4) | 3.2-15.6 | 6(9.5) | 2.3-16.8 | 2 (9) | 00-21.1 | |
| No data | 68 (80) | 71.5-88.5 | 50 (79.3) | 69.4-89.4 | 18 (81.8) | 65.7-97.9 | |
| Victim of physical violence | Yes | 6 (7) | 1.6-12.5 | 4(6.3) | 0.3-12.4 | 2 (9) | 00-21.1 |
| No | 8 (9.4) | 3.2-15.6 | 5(7.9) | 1.3-14.6 | 3 (13.6) | 00-28 | |
| No data | 71 (83.6) | 75.6-91.4 | 54 (85.7) | 77.1-94.4 | 17 (77.2) | 59.8-94.8 | |
| Victim of psychological violence | Yes | 22 (25.8) | 16.6-35.2 | 17 (26.9) | 16-37.9 | 5 (22.7) | 5.2-40.2 |
| No | 3(3.6) | 00-7.5 | 2(3.2) | 00-7.5 | 1 (4.5) | 00-13.2 | |
| No data | 60 (70.6) | 60.9-80.3 | 44 (69.8) | 58.5-81.2 | 16 (72.7) | 54.1-91.3 | |
ADHD: Attention Deficit Hyperactivity Disorder.
* The reported psychiatric illnesses are not mutually exclusive, as the same patient may have more than one.
Source: Own elaboration.
With regard to family characteristics, it should be noted that 62% of the patients did not have a nuclear family composition, i.e., they did not live with both parents, but most were part of an extended, reconstituted, single-parent family or of divorced parents (Table 3).
Table 3 Characteristics and family history of the study population.
* Nuclear family: consisting of two adults, male and female, with their children; single-parent family: children that live only with a parent who is single, widowed or divorced; extended family: nucleus integrated by a big family with grandparents and other relatives;21 reconstituted family: consisting of a legally married couple, where at least one of the spouses was previously married and has a child from their previous marriage.22
Source: Own elaboration.
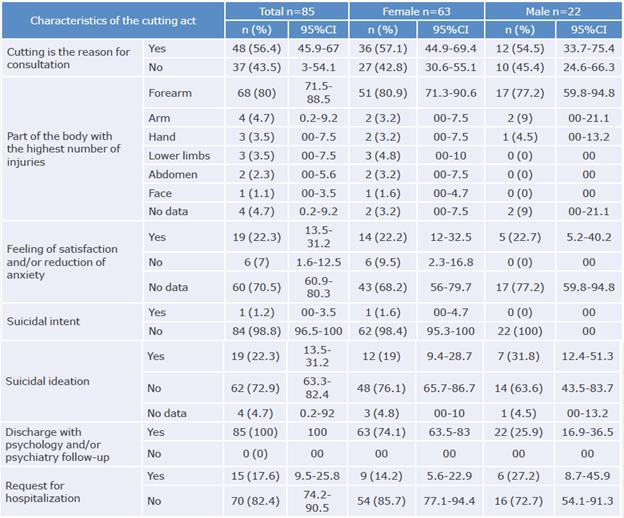
A history of family psychiatric illness was found in 17.6% of the medical records reviewed, with major depression and bipolar affective disorder being the most frequent. The characteristics associated with cutting are variable and are described in Table 4.
Table 4 Characteristics associated with the cutting act in the population studied.
Source: Own elaboration.
Cutting was not the reason for consultation in 43.5% of cases. It was discovered incidentally during the physical examination in patients who were mostly consulting for suicide attempts, drug intoxication, suspected sexual abuse, decompensation of underlying psychiatric illness, etc.
The most frequently injured body part was the forearm (80%), followed by the arm (4.7%), hand (3.5%), lower limbs (3.5%), abdomen (2.3%), and face (1.1%). In 22.3% of the cases, cutting generated a feeling of satisfaction and/or reduction of anxiety, without significant differences according to sex.
On the other hand, 72.9% of the population did not have suicidal ideation during the interview or psychiatric service assessment. However, it is striking that this type of idea was present in 31.8% of boys and only in 19% of girls.
According to the care protocol of the study institution, all patients diagnosed with cutting were admitted to an outpatient program for treatment and follow-up by the psychology and psychiatry services.
Discussion
The prevalence of cutting found was lower than what has been reported in other scenarios.1,12,13,23,24 This could be due to factors such as the poor knowledge that health workers have about this pathology; the fact that the literature reports the prevalence of all nonsuicidal self-injury disorders without quantifying the prevalence of cutting as a single entity, perhaps overestimating it, and the fact that only patients admitted for pediatric care in the emergency department were included in this study and not the pediatric population in general.
According to Martorana,25 most patients (72.3%) engage in self-injurious behaviors between the ages of 12 and 16, which coincides with the present study, where the average age of occurrence of cutting was 14 years. The male: female ratio was 3:1, much higher than that reported by Albores-Gallo et al.11 in Mexico and Geulayov et al.24 in England, where the ratio was close to 1:1. However, our results are similar to those reported by Laukkanen et al.12 in Finland and Frías-Ibáñez et al.15 in Mexico, where the ratio was 2.7:1 and 3:2, respectively.
Factors such as non-nuclear family composition,26 history of sexual,15,27 physical and/or psychological abuse,26 and poor academic performance5,12 have been associated with cutting. Therefore, these factors should be systematically evaluated in the pediatric population countrywide, as they are present in the Colombian context.
Although alcohol consumption is largely associated with cutting in many studies, especially in males,13,28-30 the present study could not explore this aspect since there was no information about it in 85.8% of the medical records. Further studies should take this risk factor into account.
The findings of the present study are consistent with those of Matsumoto et al.26 regarding the consumption of psychoactive drugs (1 in 4 males) but differ regarding the presence of suicidal ideation, which was 22.3% here, while for Matsumoto et al.26 it was 77.8%. At this point, it should be noted that the present research found a significant difference between boys and girls in relation to the presence of suicidal ideation: 31.8% versus 19%, respectively. As reported in the literature, in the male population, injuries accompanied by suicidal thoughts are more likely to become severe or turn into suicide attempts.5,31
In addition, more than half of the study population had a history of psychiatric illness, with major depression being the most common. In this aspect, the male population was also predominant, which coincides with what was reported by Robinson,17 Laukkanen et al.,32 Hintikka et al.33 and Mars et al.34
Contrary to the results of this work, Jones et al.,10 in a study on psychiatric disorders in 44 adolescents, concluded that 100% of the women (n=41) had internalizing disorders: 63% had major depressive disorder, 37% suffered from anxiety, and 15% had an eating disorder, conditions that were not mutually exclusive. While Laukkanen et al.12 and Gmitrowicz et al.13 showed a significant association between cutting and the presence of psychiatric disorders or substance abuse, in other studies5,7,34 many of the patients' behaviors were classified as normal from a psychological point of view.
Cutting is often a manifestation that precedes a suicide attempt. For example, Mars et al.34 established that patients engaged in cutting tend to commit more lethal forms of damage, thus becoming a predictor of this event (OR:3.94, 95%CI:2.67-5.83 and years of potential life lost: 31.4) but this does not happen in all cases. Mars et al.5 studied the association of risk factors with this outcome and found that those that pose the greatest risk for committing suicide were depression and anxiety disorder. As for the characteristics associated with the cutting act, the present study found that suicidal intent has a very low prevalence and was only reported in 1 of the patients, similar to what Muehlenkamp et al.3 and Calvete et al.35 have reported.
The most frequently injured body part in the target population was the forearm, specifically the wrists, regardless of sex. This differs from the findings reported by Albores-Gallo et al.11 and Matsumoto et al.26, where the prevalence of injuries in this area was 16.4% and 16.9%, respectively, and it occurred more frequently in women. The study by Matsumoto et al.26 also suggested that patients who performed wrist cuts were at higher risk of future suicide attempts than those who performed them in other locations.
In this study, 22.3% of the population reported a feeling of satisfaction and reduced anxiety after performing the cuts, with no differences between sexes, which coincides with what is described in the literature. Laukkanen et al.12 found that it is an autotherapy method for relieving stress; Jones et al.10 reported that these patients have an elevation of endorphins and serotonin during the cutting act that could produce a sense of well-being; and Reitz et al.,8 in a group of women with borderline personality disorder, concluded that those who self-injured showed a decrease in heart rate, and levels of stress and anxiety during the act. These results suggest that it is necessary to investigate possible stressors in the population that engages in cutting.
The prevalence of cutting in adolescents is on the rise;36 therefore, characterizing the population at risk is a first step towards establishing prevention and mental health promotion programs that take into account mental health as a vital component for the comprehensive development of children and adolescents. The present study is the first in Colombia to describe cutting and the prevalence of risk factors in the pediatric population; it also presents the characteristics and the history of this population, which may be useful to clinicians in emergency and pediatric services and specialists in the area of mental health to understand this condition in the local context and in similar scenarios. Likewise, this work opens spaces for research on variables associated with cutting, which have to do with family composition, school performance, and a history of mental illness and violence.
Although the design of this study and the sources of information do not allow establishing an association between cutting and the risk factors reported in the relevant literature, it is clear that multidisciplinary child health teams should pay special attention to these factors to identify the cases that are at higher risk of relapse and potential suicide attempts. This is especially important because two risk factors were found in the study population that are associated with a worse prognosis according to the literature: the presence of a psychiatric disease (more frequent in males) and the forearm as the most frequently affected part of the body. Therefore, it is necessary to carry out new studies to establish causal associations and determine the effectiveness of the treatments offered and, thus, extend the results obtained here.
One of the limitations of the present study was the low external validity since the population studied included only pediatric patients treated at the emergency department, which may represent only the spectrum of the cut with the highest severity. In addition, there were some limitations in identifying the population's own risk history, given the sources of information that were taken into account.
Conclusions
The findings of the present study allow establishing that the prevalence of cutting in the sample was lower than that reported in the general pediatric population in other countries. Also, this condition was three times more frequent in girls, and more than half of the patients had no nuclear family and had low school performance.
Personal history of psychiatric illness had an important correlation with the practice of cutting, especially in the male population, and therefore it should be explored as a risk factor in future studies.
The characteristics described here will make it easier to identify cutting in the Colombian pediatric population and fill a knowledge gap in the country about its prevalence and main features. However, further studies are needed to determine the effectiveness of therapeutic measures targeted at this population.















