Introduction
In December 2019, in the city of Wuhan, China, a new coronavirus (SARS-COV-2) was discovered, and the disease that it causes is the coronavirus disease 2019 (COVID-19). The virus spread rapidly, and by the end of January 2020, more than 830 cases of COVID-19 had been confirmed in 9 countries, mainly in Asia. This situation led the World Health Organization (WHO) to declare the outbreak of this disease as a public health emergency of international concern on January 30, 2020. Then, on March 11,2020, due to the alarming levels of spread and the few actions taken to prevent infection, the same organization declared COVID-19 a pandemic.1 Although it has not been demonstrated, the origin of the virus is believed to be related to a seafood market in Wuhan.2
At first, it was believed that COVID-19 affected older people only, but this notion has been proven wrong since people of all ages are susceptible to infection. In addition, regardless of the viral load, the clinical characteristics of this disease vary and can range from an asymptomatic state to acute respiratory distress syndrome (ARDS) and multiple organ failure, which require transferring patients to the intensive care unit (ICU). The most reported symptoms are fever, cough, sore throat, headache, fatigue, myalgia, dyspnea, and even conjunctivitis.2
Considering the impact of COVID-19 worldwide, several studies on this disease are currently underway. Adhikari et al.3 carried out a scoping review that analyzed 65 research articles published between January 1 and 31, 2020, which helped to understand its epidemiology, clinical diagnosis, prevention, control, and causes. This work raised the need to implement preventive measures such as the use of face masks, good hand hygiene practices, among others. The authors also reported that no specific antiviral treatment is effective to date and, therefore, infected people depend mainly on symptomatic treatment and supportive care. In this regard, the researchers highlighted the need for new, high-quality, and valid studies on the virus to establish short- and long-term solutions.3
COVID-19 is a global challenge given its impact on health systems around the world. According to the study by Lai eta/.,4 which included 278 patients in 3 studies of the clinical characteristics of patients with pneumonia caused by the Wuhan SARS-CoV-2, 25.9% of participants were admitted to an ICU, 20.1% developed ARDS, and 8.3% and 3.2% required invasive mechanical ventilation and extracorporeal membrane oxygenation due to refractory hypoxemia, respectively. Concerning the outcome of this disease, Cunningham et al. described a mortality rate of about 2% based on the findings reported by Lai etal.,4 who described a mortality rate of 2.5%.
As mentioned above, and according to various studies, SARS-CoV-2 can affect different age groups.6 10 However, Lloyd-Sherlock etal.11 show that the risk of mortality from COVID-19 increases in people over 60 years of age, especially those with chronic conditions such as cardiovascular disease. This is a worrying situation because the largest number of people in this age group are in low- and middle-income countries where health systems are weak and unable to meet the needs of these patients, who also require nutritional support adapted to their clinical evolution and specific conditions.
With this in mind, the objective of the present literature review was to identify recommendations given to hospital health care teams for providing nutritional care to inpatients over 18years of age infected with COVID-19.
Materials and methods
A literature review was conducted in PubMed taking into account the PRISMA guidelines12-14 and based on the following search strategy: Language of publication: English and Chinese; Publication period: December 1, 2019, to March 21, 2020; Search terms: "Coronavirus Infection", "Severe Acute Respiratory Syndrome", and "Nutrition for Vulnerable Groups". All clinical trials, clinical practice guidelines, original articles, and reviews (systematic or narrative) describing nutritional support practices in COVID-19 adult inpatients were included.
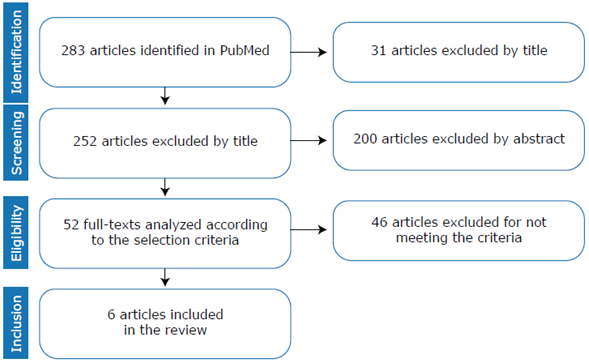
The initial search yielded 283 studies, of which 231 were eliminated because they were not relevant to the research objective. The remaining 52 articles were checked to confirmed if they met the inclusion criteria and 6 were finally selected for a comprehensive analysis (Figure 1).
Results
Of the 6 articles included in the analysis, 5 were published in English and only 1 in Chinese. Table 1 presents the main characteristics of the 6 studies that, in the authors' opinion, present the most relevant results with respect to the objective of this review (nutritional support and dietary recommendations for adult inpatients with COVID-19) and propose strategies for clinical practice.
Table 1 Studies on nutritional intervention strategies.
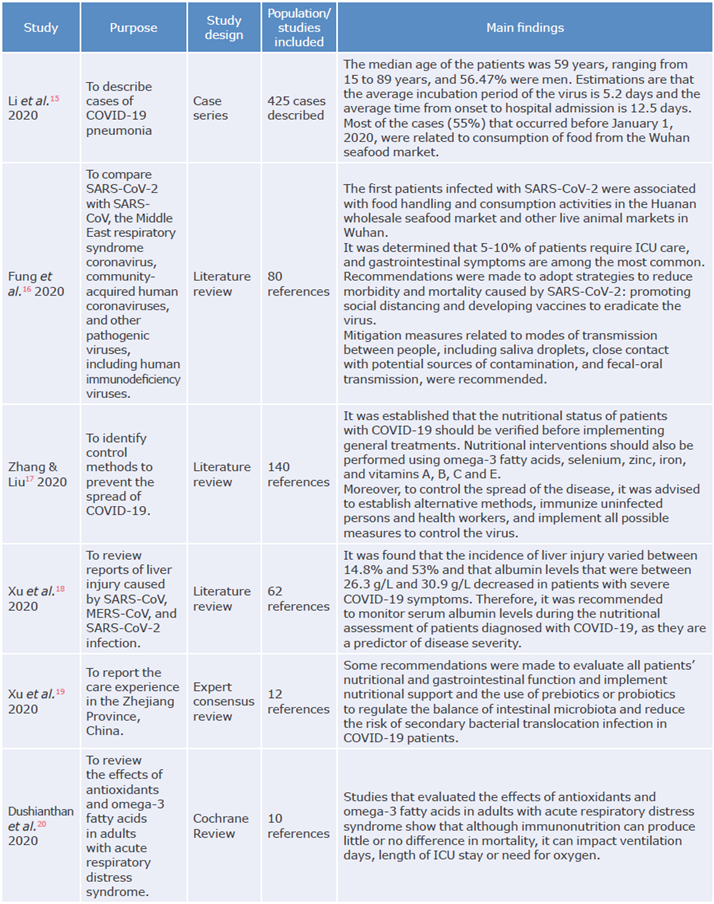
ICU: Intensive care unit.
Source: Own elaboration.
Except for a series of cases in the adult population,15 all publications were literature reviews. The main topics addressed by the selected studies were the implementation of practices related to the evaluation and monitoring of nutritional status;17,19 the evaluation of interventions to manage and reduce the severity of lung and liver complications,18 which is one of the objectives of specialized nutritional intervention; and the review of the effects of antioxidants and omega-3 fatty acids in patients with ARDS.20
Discussion
The International Committee on Taxonomy of Viruses named the disease caused by the SARS-CoV-2 virus COVID-19,16 which the WHO declared as a public health emergency of international concern on January 30, 2020, and as a pandemic on March 11 of that same year.1 It has a wide range of clinical manifestations that are determined mainly by virus-host interaction and the action of pro-inflammatory cytokines.21-23 Therefore, it is necessary to understand the mechanisms by which SARS-CoV-2 acts to design and establish effective therapies for infected patients.16
Although there is no specific treatment for COVID-19, it is known that respiratory support is essential to improve oxygenation and reduce mortality.24 Likewise, it has been established that alternative methods should be found to control the development of the disease, including the evaluation of the nutritional status of each patient with COVID-19 before providing general treatment.16,25,26
Nutritional support practices
Nutritional support should be one of the key measures for the comprehensive treatment of patients with COVID-19.27,28 The main aspects to be considered about hospital nutritional care of people who have contracted SARS-CoV-2 virus are presented below.
Identification of nutritional risk
As stated by Zhang & Liu,17 nutritional risks should be established for hospital stays of more than 48 hours, as well as the initiation and objectives of nutritional support in such a way that energy, proteins, and water balance are monitored, ensuring a daily contribution of 20-30 kcal and 1.2-2g protein/kg, as validated by Singer et al.29 Furthermore, according to the Spanish Academy of Nutrition and Dietetics and the General Council of Dieticians-Nutritionist of Spain,27 in case of enteral nutrition, it is necessary to consider measures to reduce the risk of aspiration pneumonia and the loss of respiratory protection.
Other important aspects should be considered when designing treatments for patients with COVID-19. For example, Barazzoni et al.30 recommend detecting patients with malnutrition and undernutrition because these conditions are associated with a higher mortality rate from this disease. In this regard, strategies should be implemented to improve nutritional status and ensure supplementation of vitamins and minerals in the general population, as well as to promote physical activity taking into account appropriate biosafety precautions and protocols.
Also, before starting any treatment for COVID-19, it should be established whether the patient requires oral nutritional supplements to meet their specific needs.
Nutritional support formulation
Regarding the formulation of nutritional support, Siger et al.29 and Fan et al.31 suggest, first, evaluating muscle function through dynamometry and then prescribing formulas enriched with omega-3 fatty acids. This recommendation is based on the fact that this protocol results have a positive impact on the length of hospital stay, ventilation requirement time, and even mortality in patients with ARDS, acute lung injury, and sepsis.32-35
Other researchers also propose administering antioxidants as high-dose monotherapy only in cases of proven deficiency because oxidative stress occurs in severe critical care conditions that require mechanical ventilation due to ARDS.36,37 Reeves et al.38 also suggest evaluating the coverage of nutritional requirements in non-ventilated patients, as energy and protein intake may be inadequate, leading to the requirement and increase of time under non-invasive ventilation.
On the other hand, the benefits of using selenium to treat COVID-19 remain unclear, as research results in this regard are uncertain and, therefore, more clinical trials are required to establish its effectiveness.27,39
De Waele et al.40 reported that in pulmonary insufficiency, classically manifested as ARDS, proteins should initially be delivered at low volume and progressively increased to 1.3 g/kg/day after septic shock symptoms decrease, using both the enteral and parenteral route, or through mixed nutritional support to cover protein and caloric targets. Concerning pharmaconutrition, these authors do not recommend supplementation with arginine or selenium, but they do advise giving a low dose of glutamine to patients receiving parenteral nutrition.
It is worth noting that, as a result of the search for alternatives to curb the COVID-19 pandemic, vitamin C consumption has increased considerably thanks to its antiviral action, which has been reported for decades in multiple publications that recommend its use to prevent and treat infectious diseases.17,41,42 In this regard, Zhang & Liu,16 based on the Hemilá study43 and an analysis of SARS-CoV infection, state that this vitamin stimulates immune function and protects against infections caused by a coronavirus.
Moreover, recent publications report that vitamin D supplements can be used as a measure to reduce the risk of infection in general.44,45 In this way, Grant et al.46 established 10 000 Iu/day as the suggested dose and reported that higher doses of vitamin D3 may be useful for the treatment of patients with COVID-19.
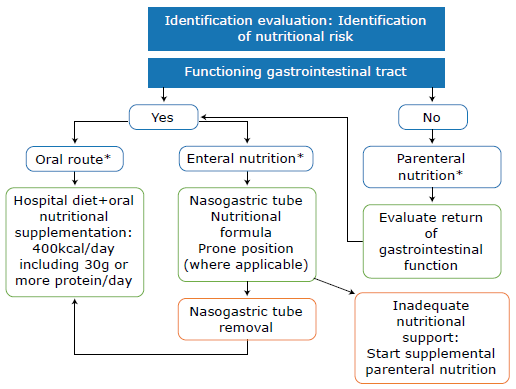
Other nutritional recommendations given by Barazzoni et al.30 focus on providing, at least for a month, at least 400 kcal/day of oral nutritional supplements that include 30g or more of protein per day. These authors also recommend prescribing enteral nutritional support to patients in whom oral nutritional needs cannot be met and evaluating the prescription of parenteral nutrition when enteral nutrition is contraindicated, or nutritional goals are not achieved by this route.
Nutritional therapy monitoring
Another recommendation to treat COVID-19 is to monitor diet and/or tolerance to enteral nutritional support in inpatients. Surveillance should be carried out based on the experience of the 2002 SARS outbreak, where between 16% and 73% of patients had gastrointestinal symptoms, mainly diarrhea during the first week of the disease.47
Feng et al.48 stated that coronavirus receptors, including angiotensin-converting enzyme 2 (ACE2) for SARS-CoV and SARS-COV-2, are digestive enzymes that can affect enterocytes in humans. Therefore, the use of probiotics or prebiotics is suggested since, in patients with COVID-19, gut dysbiosis has also been found with reduced probiotics such as lactobacillus and bifidobacterium. Also, Xu et al.19 suggested implementing nutritional support and supplying prebiotics or probiotics to regulate the balance of the gut microbiota and reduce the risk of secondary infection due to bacterial translocation.
Similarly, it is important to evaluate the passage of enteral nutrition through the nasogastric tube in intubated and ventilated patients or through the postpyloric tube in patients at high risk of aspiration or with gastric intolerance after prokinetic treatment.
The prone position per se is not a limitation or a contraindication to enteral nutrition according to Barazzoni et al.,30 who further recommend, on the one hand, to evaluate the benefit of switching to supplementary parenteral nutrition after one week of enteral nutrition and, on the other, consider the adaptation of food textures in ICU patients with dysphagia after extubation. To this end, it is necessary to assess the need to continue enteral nutrition by tube to meet the nutritional needs of patients.
In relation to nutritional biochemical parameters, levels of albumin, lymphocytes, lactate dehydrogenase, neutrophils, and C-reactive protein should be monitored as these parameters are highly correlated with acute lung injury. Liu et al.,49 from a study of 12 cases of patients infected with SARS-CoV-2 who developed pneumonia, described the laboratory characteristics and potential bio-markers for predicting the severity of COVID-19. They stated that 50% of cases develop ARDS, which presents with hypoalbuminemia; decreased CD8, lymphocytes and neutrophils count; and elevated C-reactive protein and lactate dehydrogenase. Based on such observations, the authors concluded that age, viral load, lung injury score, and blood biochemistry measures could be predictors of disease severity.
The following are the basic recommendations for clinical practice regarding the prescription and follow-up of nutritional support according to the literature reviewed (Table 2).
Table 2 Basic recommendations for clinical practice for the prescription and follow-up of nutritional support.
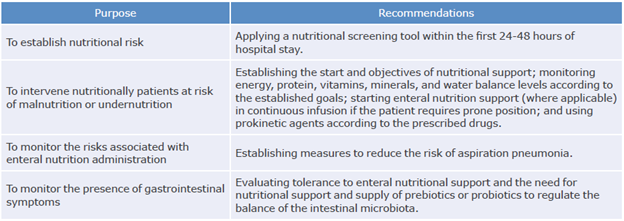
Source: Own elaboration based on Zhang & Liu,17 Xu et al.,18 Xu et al.,19 Li et al.28 and Singer et al.29
Finally, according to Heymann & Shindo,50 it is necessary to continue to design communication strategies that provide the general population and vulnerable populations with actionable information to know what follows regarding hospital nutritional care in the context of the coronavirus disease for self-protection. he following flowchart presents the aspects to be considered to care for inpatients with COVID-19 (Figure 2).
Practices in hospital food services
Because of the impact that COVID-19 has had around the globe and the complications it can cause in infected patients, actions should be proposed to respond to the health emergency that this disease has caused, prevent foodborne diseases, contribute to the containment of the virus, and establish theoretical-practical recommendations for hospital nutritional intervention.
In order to achieve this, first of all, workflows should be created, and the food service staff divided into two groups, one in charge of the provision of hospital food to patients with COVID-19 and another in charge of feeding the care and administrative staff. This is necessary because the virus has high transmissibility from person to person by air, through droplets and contact, so the strict application of protocols is required to isolate infected patients and prevent nosocomial spread.15,51,52
Secondly, systematic processes of risk analysis and critical control points should be strengthened.53 In this sense, it is essential to plan the safe transport of the food to be supplied to patients with suspected or diagnosed COVID-19. Similarly, food service workers in hospitals, in general, should be educated on the disease, biosafety protocols in the framework of the pandemic, and specific recommendations for infected patients.25
The following are the actions aimed at mitigating the spread associated with food services based on the authors' experience and the recommendations found in the literature:
From the perspective of patient safety, every health institution (medical centers, clinics, hospitals, etc.) must have a protocol to ensure nutritional care for patients. Such protocol should include indications of diet-based therapy and nutritional counseling forfood supply service companies41,54 and it should also implement sequence checklists for work teams in charge of preparing the menus to minimize the movement of personnel, control infection, and prevent cross-contamination.25
Finally, to ensure good hydration, nutrition, and food for patients with COVID-19, hospital food services should adopt the recommendations stipulated by the Spanish Academy of Nutrition and Dietetics and the General Council of Dietitians-Nutritionists of Spain.27 Also, as stated by Ren etal.,55 it is necessary to share open and transparent information with the general public about the outbreak.
Currently, evidence on nutritional interventions in the context of the COVID-19 pandemic is incipient, so methodological research should be developed to propose medium-and long-term solutions to treat these patients.
The limitation of the present research was that most publications found were literature reviews. Therefore, other studies of greater methodological rigor should be reviewed in the future to have more concrete evidence.
Conclusions
Given the complex and constantly evolving dynamics of SARS-CoV-2 infection and its outcomes, theoretical-practical nutritional intervention guidelines should be implemented to respond immediately to each patient's requirements.
Recommendationsfor hospital nutritional care of patients with COVID-19 are based on nutritional care processes and food services management. According to these recommendations, strategies for nutritional risk assessment should be established, as well as nutritional support interventions that reduce the risk of malnutrition by ensuring a caloric and nutritional contribution that favors clinical outcomes. It is also necessary to monitor the risks associated with the administration of nutritional support and metabolic alterations associated with this disease.