Introduction
Since its emergence in December 2019, COVID-19, a disease caused by the novel SARS-CoV-2 coronavirus, has had a significant impact on the economy, health and culture, and has triggered a global crisis related to the high burden of the disease, so much so that the World Health Organization (WHO)1 declared it a pandemic in March 2020. As the crisis develops, the pandemic has created a synergistic effect in the economy and society that has exacerbated existing inequalities in several countries.2-5
In order to control the spread of the virus, governments around the world implemented biosafety protocols at the beginning of the pandemic and established lock-down measures that restricted the development of social and economic activities. Current efforts are aimed at reactivating the economy to improve social conditions, which have deteriorated as a result of the emergency. With this purpose in mind, multiple strategies have been designed to allow for this reactivation while reducing the impact of the virus. However, decision-makers are still divided on when and how restart economic activities because there is a potential risk of increasing the disease burden and overwhelming the health system if measures are implemented without controlling the epidemic first.
In Colombia, the Ministry of Health and Social Protection issued Resolution 777 on June 2, 2021,6 which defined the criteria and conditions for the resumption of economic, social, and State activities. That Resolution established that reactivation will be carried out in three phases depending on the score obtained with the Municipal Epidemiological Resilience Index (IREM), which allows identifying the territories with greater epidemiological resilience as the basis for reopening spaces for the development of economic and social activities.7,8 It should be noted that the experts consider that this is not the best time to present these guidelines, since the country is currently going through a prolonged plateau of what would be the third peak of the epidemic, making it inappropriate to consider reactivating restricted economic and social activities at this time.
Taking into account the profound implications of Resolution 777 of 20216 and the implementation of the IREM on public, health, social and economic policies, the objective of this reflection is to make a critical analysis of the technical aspects of the index and explore the feasibility of its implementation as a support for the resumption of all economic and social activities proposed in the resolution.
Municipal Epidemiological Resilience Index
The IREM is an index used as a tool to determine whether restricted economic, social, and cultural activities can be resumed in the territories affected by the COVID-19 pandemic. It consists of four dimensions: immunization, adjusted seroprevalence by youth ratio, health system capacity, and testing capacity (Table 1).7 The values obtained with the IREM measurement vary between 0 and 1, and the decision to resume activities is made if a value >0.5 is obtained in cycle 2, as established in Resolution 777 of 2021.6
Table 1 Dimensions and equations of the Municipal Epidemiological Resilience Index of the Colombian Ministry of Health and Social Protection.
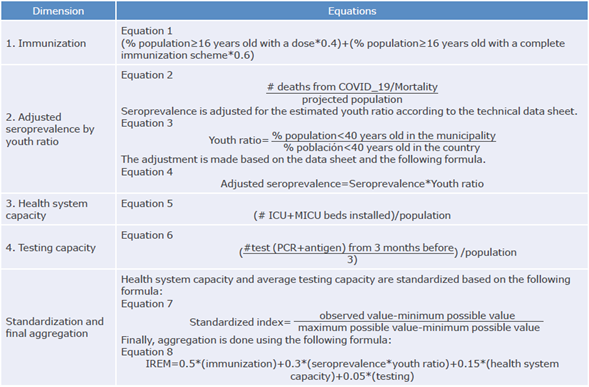
Source: Own elaboration based on the Technical Report of the Municipal Resilience Index.7
Critical analysis
The critical analysis of the IREM was carried out based on the following aspects: face validity, content validity, construct validity of the global index and construct validity of its dimensions. Finally, the feasibility of IREM implementation was assessed.
Face validity
Despite the subjectivity of this type of validation, the variables proposed to measure the IREM (i.e., immunization, seroprevalence, health system capacity and testing capacity) do not truly reflect epidemiological resilience, as this index reduces the concept to these four dimensions in the absence of other variables relating to the population and the specific dynamics of each territory. In other words, the IREM does not seem to measure what it intends to measure.
Content validity
The name of the IREM must be critically analyzed because, as a resilience index, it is expected to be a useful tool for accurately measuring the resilience of a municipality or department to determine measures for the resumption of restricted economic and social activities and establish measures aimed at controlling massive events.
Resilience is a polysemous concept that can refer to an individual, a family, communities/territories, countries and even health systems.9 Specifically, the resilience of territories or communities is defined as the capacity of a system or community to use the resources, services and opportunities available, that is to say, its capacity to interact with a more complex social, economic and cultural system (governmental and non-governmental agencies, natural and constructed environments, and citizens). These are capacities that allow the community to resist, transform, and recover in a timely and efficient manner from the effects of a dangerous or risky event.10-12 Thus, in this context, resilience is understood as the capacity of communities or territories to adapt and thrive during crisis, disaster, and emergency situations.
In view of the above, municipal epidemiological resilience should take into account the capacity of the territories to use services, resources and programs to overcome critical events such as the COVID-19 pandemic. A resilience indicator should comprehensively report the territory's capacity to manage its current situation and overcome the stressors resulting from such an event. In this regard, several authors have approached the assessment of resilience in the context of COVID-19 that could be taken as an example, which include social, economic, and health system indicators.13-19
The critical analysis of the IREM content validity shows how the variables that measure the territory's capabilities to overcome and cope with the pandemic are not included in the index, moving away from the established idea of epidemiological resilience, which is broader in its inception.
Global construct validity
The IREM technical report does not provide sufficient information on the theoretical or technical justifications that were used to develop this index or on the possible alternatives considered. The document also makes it difficult to establish its validity as a global construct because it does not allow generating a clear judgment on the variables included, nor on the weighting applied to each dimension (Equation 7, Table 1).
Construct validity of each dimension
As mentioned above, the inclusion or omission of specific variables, when viewed separately, lack proper justification. The generation of multidimensional indexes is a complex process that must consider the interaction between its components. In addition, an index must take into account the complementarity of its dimensions and provide a parsimonious explanation of the phenomenon without losing clarity and its capacity to register the ever-changing dynamics of the aspect being measured. The following is a description of each of the variables that make up the index proposed by the National Government:
1. Immunization: Equation 1 (Table 1) assumes that the proportion of the population vaccinated with a single dose accounts for 40% of the immunization value, whereas the proportion with a complete vaccination schedule accounts for 60%. Assuming that the entire population receives the first dose in the municipality (0.4) and that 16.6% of them have a complete scheme, this dimension alone would provide a value of 0.5 to the IREM (supposing that the minimum value is zero and the distance between the maximum and the minimum value is 1), thereby enabling the municipality to reactivate its restricted economic and social activities, regardless of the behavior of the other variables.
The way this dimension is estimated can send the wrong message to the population, as it suggests that the first dose grants immunity and safety. This assumption may backfire given that immunity is only achieved two weeks after administering the second dose, in the case of the Pfizer vaccine, and that this span varies for the other COVID-19 vaccines.20 Furthermore, the assumption under which the authors decide to weigh this dimension internally is not clear.
Similarly, Resolution 777 of 2021 uses vaccination coverage to define the scenario in which it is possible to move from phase 1 to phase 2. For this purpose, it was established that 69% of the population prioritized in stages 1, 2 and 3 (phase 1), that is less than 10 million people (approximately 19% of the population), should be vaccinated. It is also worth noting that the Resolution does not explain how the 69% figure was calculated to determine the transition from phase 1 to phase 2.
2. Adjusted seroprevalence by youth ratio: This variable requires making some precisions:
a. The estimate of what is called "seroprevalence" in the IREM is based on the infection-fatality ratio used to estimate the number of cases subsequently converted into population proportion (Equation 2, Table 1). This actually corresponds to the burden of infected people or infection rate.21
Using the burden of infected people instead of the seroprevalence is a mistake, since those who can be included in a seroprevalence indicator using infection as a proxy of natural immunity are the survivors of the infection. The burden of infected or sick people includes all deaths and survivors and is not equivalent to seroprevalence.22,23 This IREM bias skews the results toward an overestimation of the variable and alters the end result.
b. The youth ratio adjustment (Equations 3 and 4, Table 1) assumes that seroprevalence increases when the proportion of population under 40 years old in a territory is higher than the country average. In other words, the IREM authors assume that municipalities with higher proportions of population under the age of 40 have a higher seroprevalence. This assumption lacks scientific support and is not a variable in the estimation that accounts for the capacity to adapt, as evidenced in the aging indexes reported at the municipal level by the National Administrative Department of Statistics (DANE by its acronym in Spanish).24
c. The WHO defines people between the ages of 10 and 24 as young people,25 so the name "youth ratio" in Equation 3 (Table 1) is questionable since it establishes that young people are those under the age of 40. The definition of youth is particularly important in this context because, given the dynamics of immunization, it imposes greater risks on the population defined as such.
SARS-CoV-2 infection rapidly changes over time, requiring real-time adjustments and measurements that can be reflected by the burden of infection (based on the proportion of infected cases within the population) and the effective reproductive number (R(t)) in each territory of the country and in the subterritories within major cities.26 This gives clearer information for decision-making than the number of cases based on the overall case fatality rate for each territory.
3. Health system capacity in the territory: This variable, which corresponds to the installed capacity of beds in intensive and intermediate care units (ICU and IMCU, respectively), has the following limitations in the IREM proposed by the Colombian Ministry of Health and Social Protection:
a. The IREM established that this variable should be monitored every two weeks to evaluate the resumption of economic and social activities; however, this is a static value that is not expected to change in that time span. In this regard, the ICOVID Chile group proposes using this variable to estimate the maximum limit of infected patients in the area of influence of the IMCU and ICU that requires public policy interventions after being exceeded to generate actions that ensure the delivery of health services for the expected demand or to design alternative strategies.21
b. Moreover, the IREM has a geographical limitation due to the referral and back-referral patterns between IMCU and ICU, since the indicator does not allow knowing the municipal installed capacity or the municipality response capacity, and penalizes the small municipalities where the resource is not available.24
The variable 'health system capacity in the territory' refers to a complex and unstable construct that must be measured in the space-time dimension and not only in absolute numbers of resources available at a given time. Thus, measurement of time intervals must consider, on the one hand, the availability of resources in the territory at any given time and the possibility of expanding this capacity through flexible referral and back-referral systems and, on the other, the complete inability to respond to demand. This would create a more realistic scenario for correct decision-making, which is the final goal of the IREM. From a territorial application perspective, this index, as designed, punishes small municipalities with insufficient or non-existent resources, which may result in inequity and frustration.27
c. A variable that has been classically used to monitor IMCU and ICU availability is occupancy percentage, which is not included in the IREM despite being mentioned with its corresponding cut-off points in Resolution 777 of 20216 for reactivation decision-making in phase 1, particularly concerning the gradualness of some measures such as public transportation capacity. The trend in IMCU and ICU percentage is an effective variable for monitoring the dynamics of SARS-CoV-2 infection, so an increase in occupancy guides the decision maker better than a cut-off point above or below 85%, as established in the Resolution.6
d. The measurement of health system capacity in the territory only reflects the tip of the iceberg regarding the care situation in the country for patients with COVID-19 and does not account for the installed capacity of services and supplies relevant to the care of critically ill patients with this disease. Besides the percentage of MICU and ICU occupancy, the measurement of the health system's installed capacity should consider the use of emergency services, mental health, general hospitalization and surgery rooms, as well as emergency transport systems, pre-hospital care and home care. Moreover, the index does not include the demand for and use of primary health care programs such as non-COVID immunization programs and clinical care for people with complicated influenza, who, until proven otherwise, are suspected COVID-19 cases.28
In this sense, health system resilience may be compromised if its capacity to respond to conventional demands for care postponed during the pandemic, or to emerging demands, is also analyzed, as demonstrated by other research works on other priority conditions.29-31
e. Other variables, such as the registration of patients with invasive mechanical ventilation outside the MICU and ICU, the number of patients with MICU and ICU waiting times longer than 24 hours, and the weekly variation rate of hospitalization by COVID-19, should be considered for SARS-CoV-2 infection decision-making. Therefore, these indicators should also be taken into account when measuring the capacities of the health system in a territory.
4. Testing capacity: This variable may be obtained daily or weekly for every 1 000 or 10 000 inhabitants. However, according to the IREM data sheet, it is extracted from the average number of tests (PCR and antigens) performed in the previous three months (Equation 6, Table 1) and does not allow making real-time decisions regarding the dynamics of COVID-19 infections. The positive rate of the tests taken is a critical variable for understanding the dynamics of virus transmission and making decisions from public policy, but it is not taken into account in the IREM.
This variable should be complemented not only with the positive rate but also with indicators of adoption and follow-up of the Testing, Tracing and Sustainable Selective Isolation strategy (PRASS by its acronym in Spanish). This program was established by the Colombian Ministry of Health to slow down the transmission of COVID-19 and break chains of transmission; however, its potential indicators are unknown and have not been integrated into this proposal for the reactivation of economic and social activities.32
In this regard, the ICOVID Chile group21 proposed the early confirmation of cases, which consists of identifying the proportion of symptomatic cases whose PCR test results are reported to health authorities within the first three days after the onset of symptoms as a good indicator of response to early case confirmation. Thus, testing accounts for early consultation, which is expected to occur within the first two days after symptom onset and considers an additional day to perform the laboratory test.21 In this regard, in the United States, the Centers for Disease Control and Prevention33 has also strengthened surveillance for SARS-CoV-2 based on testing.
It is assumed that early case confirmation implies the adoption of isolation strategies for asymptomatic patients and follow-up strategies for symptomatic patients who do not require hospitalization. This should be tracked through PRASS program indicators, and its territorial adoption should be reinforced through its inclusion in a high-impact measurement as the IREM is expected to be.
As explained before, the monthly average testing based on the average of the preceding three months is a very simple variable that does not cover all possible monitoring suggestions that are unquestionably more convenient to support decision-making.
In summary, based on the critical analysis of the IREM, it can be established that in order to consider this index as valid and precise, it requires a systematic development process and validation to guarantee face, content and construction validity, especially of its internal and global weightings.34 Therefore, it is clear that the index proposed by the Colombian Ministry of Health and Social Protection does not meet the requirements of this type of tool and its validity is questionable for decision-making in public policy.
Appropriateness of the use of the Municipal Epidemiological Resilience Index
Although it is understood that there is a need for instruments to support public policy decision-making, they must be developed on the basis of evidence and withstand critical analysis of their validity and accuracy. This is mostly due to the fact that the use of invalid instruments can influence decision-making, which, in turn, can have serious consequences for the health of the population.
In order to validate the IREM, it is recommended to consider the impact of patient mobility between territories and demographic density. Both situations, besides changing the dynamics of virus dispersion and of potential serotypes that may worsen the burden of infection,35 require making adjustments to the public health response capacity.
Furthermore, in Colombia, the COVID-19 epidemic has greatly affected vulnerable groups since a greater impact and a higher mortality rate have been observed in people living in low socioeconomic conditions, enrolled in the subsidized health scheme within the Colombian healthcare system and indigenous communities.3 This has also been evident in the proportion of cases accumulated in socioeconomic strata 1 and 2 (strata range from 1 to 6, being 1 the lowest and 6 the highest), as well as in some specific localities of Bogotá, both during the first and second peaks of the epidemic.4 This is relevant because, to date, there is no evidence of strategies to mitigate the social and health impacts on vulnerable populations and, on the contrary, this situation perpetuates the social and economic vulnerability of these groups.
Recently, Oliu-Barton et al.36 compared the impact of the COVID-19 pandemic in the countries that implemented elimination strategies (actions to control SARS-CoV-2 and stop transmission in the community) with those that implemented mitigation strategies (gradual and specific measures to avoid overburdening health systems), among them Colombia. They found that health outcomes (deaths per million, per day), economic growth (weekly change in gross domestic product), democratic solidarity and civil liberties were better in those countries that opted for elimination strategies (Figure 1).
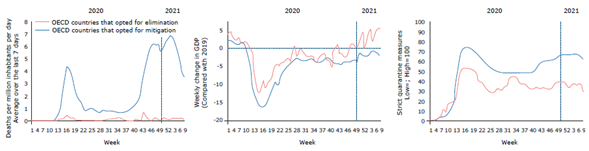
Source: Taken from Oliu-Barton et al.36
Figure 1 Effect of elimination or mitigation strategies in countries of the Organization for Economic Cooperation and Development. 2020-2021.
Resolution 777 of 2021,6 enacted during the crisis caused by the third peak of the pandemic, when the occupation of the MICU and ICU was at its worst historical moment since the beginning of the emergency and with an anticipated shortage of oxygen and medicines,37 conveyed the wrong message to the community regarding the resumption of activities in the midst of the crisis.
The "do-no-harm communication" strategies during the COVID-19 pandemic focused on both press and mass media communications, as well as those coming from governmental and public health entities38,39 and, therefore, information has not been properly transmitted.
In this sense, without an appropriate communication strategy, the protocol for the resumption of economic and social activities based on a "resilience" index could be misinterpreted, as the ability to "resist the virus" would be considered achieved. As a result, people and institutions of the country may be less likely to adhere to biosecurity measures (hand washing, physical distance, face masks, and no crowding), which should be maintained even after the economic and social reactivation of restricted activities.
Conclusions
The IREM proposed by the Colombian Ministry of Health and Social Protection is a tool included in the action route of a resolution issued by the same institution, whose purpose is to guide the resumption of all economic and social activities that were suspended to mitigate the effects of the COVID-19 pandemic. However, the index has serious limitations in terms of formal and technical validity, and it is not based on the evidence of what is happening in Colombia,3,4 nor does it take into account what has been recommended in other countries.36
Controlling the transmission of the virus is fundamental to overcoming the pandemic. To accomplish this, it is essential that the PRASS strategy (applied correctly) is the primary focus in the territories, and that it is accompanied by the implementation of an appropriate immunization plan and integrated strategies based on primary health care that provide sustainability to the health systems.
Priority must be given to highly vulnerable social sectors with low resilience, where the social and economic impact of the pandemic is greater, in order to reactivate the restricted activities towards a new normality.















