Introduction
Portal hypertension, defined as a hepatic venous pressure gradient (HVPG) >5 mmHg, is the main complication of liver cirrhosis and a predisposing factor for the formation of esophageal varices (EV) when HVPG is >10 mmHg.1
Estimates are that the annual incidence of EV varies between 5% and 9% in people with cirrhosis, but it has also been established that about one third of patients with compensated cirrhosis and up to 60% of patients with portal hypertension ascites develop EV.2-4 On the other hand, the incidence of gastrointestinal bleeding in patients with cirrhosis is 12% and has a mortality rate of up to 22%, which depends on the severity of the disease, the size of the varices, the magnitude of the bleeding, and the level of care of the health institution where the patient is being treated.5
Esophagogastroduodenoscopy (EGD) is the gold standard for the diagnosis of EV, and the implementation of measures (pharmacological and/or endoscopic) to prevent the development of gastrointestinal bleeding depends on the findings of this test.6 However, it is essential to keep in mind that EGD should only be performed by highly trained physicians because it is an invasive, high-cost test that is not available in all care centers and during which complications may occur. Patients with compensated chronic liver disease do not need an EGD if they have a platelet count >150 000 a liver stiffness using transient elastography <20 kPa;7 nonetheless, elastography is a diagnostic test that is not widely available in Colombia.
In this context, several mechanisms have been developed to diagnose EV in patients with cirrhosis, such as platelet count in peripheral blood smear, measurement of serum albumin levels, Child-Pugh classification, right liver lobe diameter/albumin ratio, and platelet count/ spleen diameter ratio (PC/SD).8-10
The PC/SD ratio, which was proposed by Giannini et al.11 in 2003 and evaluated by Giannini et al.12 in 2005, is a non-invasive predictor of EV with a cut-off point <909, a positive predictive value (PPV) of 96% and a negative predictive value (NPV) of 100%. This index is easy to obtain in any secondary care center because it only requires an ultrasound equipment and a clinical laboratory where platelets can be measured. However, it has not been studied in Colombia to date, so the objective of this study was to evaluate the diagnostic performance of the PC/SD ratio (cut-off point <909) to detect EV in patients with cirrhosis treated a tertiary care university hospital in Bogotá, D.C., Colombia.
Materials and methods
Design and study population
Prospective diagnostic test accuracy study. The study population included all patients over 18 years of age diagnosed with cirrhosis of the liver, of any etiology and severity according to the Child-Pugh classification, treated at the Gastroenterology Unit of the Hospital Universitario de La Samaritana Empresa Social del Estado in Bogotá, D.C., between July and December 2018 and tested for platelet count, EGD and PC/SD ratio (N=80).
Patients admitted with active gastrointestinal bleeding or hypovolemic shock, as well as those who had already received pharmacological, endoscopic, or surgical treatment for EV or who had cancer of any type in any site were excluded (n=14). The final sample consisted of 66 patients.
Procedures
Cirrhosis was diagnosed based on the liver biopsy results (METAVIR scoring system) or imaging findings (resonance or tomography) of patients who underwent any of these tests; in the latter, liver surface nodularity, expanded gallbladder fossa, hypertrophy of the caudate lobe, enlargement of the hilar periportal space, and whether the caudate-right lobe ratio was >0.65 were taken into account. The severity of liver disease was classified according to the Child-Pugh score, considering laboratory results (albumin, pro-thrombin time, and bilirubin levels) and the presence or absence of complications such as hepatic encephalopathy and/or ascites.
Moreover, esophageal varices were diagnosed via EGD, and the criteria of the American Society for Gastrointestinal Endoscopy established in the BAVENO VI consensus were considered for classification purposes: small <5mm or large >5mm.7
Automated platelet count by peripheral blood smear was expressed in platelets/microliter. Abdominal ultrasound was performed by radiologists using a Toshiba Nemio XG system, while EGD was performed by gastroenterologists with more than 10 years of experience using Olympus GIF H180 and Q150 systems.
Statistical analysis
After being included in a database, the information collected was analyzed in the SPSS statistical software (IBM SPSS Statistics for Windows, Version 21.0., Armonk, NY: IBM Corp.). In the descriptive analysis, categorical variables were expressed as absolute frequencies and percentages, and continuous variables as measures of central tendency and dispersion (mean, standard deviation, and interquartile ranges).
Similarly, sensitivity, specificity, PPV, NPV, positive likelihood ratio (LR+), and negative likelihood ratio (LR-) of the PC/SD ratio (cut-off <909) for detecting EV in the study population were calculated, and the results were compared with the findings of the gold standard test (EGD), considering a significance level of p<0.05.
Ethical considerations
The study took into account the ethical principles for medical research involving human subjects established in the Declaration of Helsinki,13 the medical ethics standards established in Law 23 of 1981 of the Colombian Congress,14 and the scientific, technical and administrative standards for health research set forth in Resolution 8430 of 1993 of the Colombian Ministry of Health and Social Protection.15
This research project was approved by the Research Ethics Committee of the Hospital Universitario de La Samaritana Empresa Social del Estado through Minutes 06 of June 21, 2018, and all patients signed an informed consent in which they agreed to participate in the study voluntarily.
Results
Of the 66 patients included in the study, 35 (53.03%) were women. The average age of the participants was 65.5 years (range: 32-87 years and standard deviation: 13.6 years). The main causes of cirrhosis were chronic alcohol consumption (40.90%), autoimmune hepatitis (22.72%) and non-alcoholic steatohepatitis (NASH) (18.18%).
The severity of liver disease measured on the Child-Pugh score was classified as follows: class A: 40.90%, class B: 40.90%, and class C: 18.18%. EV were observed in 48 (73%) patients and mean platelet count, spleen diameter, and PC/SD ratio were 139.9x109/L, 125.5mm, and 1 211.9 n/mm3, respectively (Table 1). The results concerning the diagnostic performance of the test are shown in Table 2.
Table 1 Characteristics of patients with liver cirrhosis treated at Hospital Universitario La Samaritana Empresa social del Estado between July and December 2018.
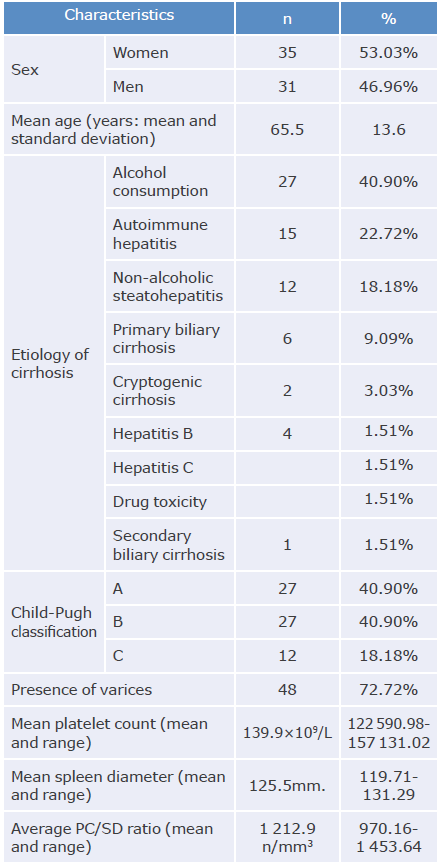
Source: Own elaboration.
Table 2 Diagnostic performance of the platelet count/spleen diameter ratio (cut-off point <909) to detect esophageal varices in patients with liver cirrhosis treated at Hospital Universitario La Samaritana Empresa social del Estado between July and December 2018.
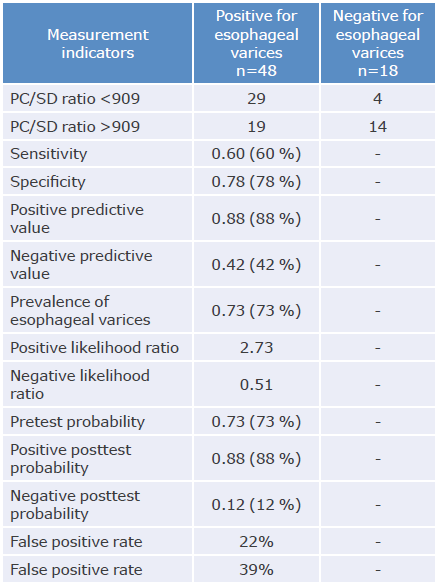
PC/SD ratio: platelet count/spleen diameter ratio.
Source: Own elaboration.
Discussion
Every year, about 2 million people die as a result of liver disease, and cirrhosis accounts for 3.5% of all causes of death worldwide, making it the eleventh leading cause of death in the world.16 Mexico was the country with the highest mortality rate due to cirrhosis in 2010, with 36 157 deaths (mortality rate: 38.5/100 000 inhabitants) and Colombia showed a significant increase in deaths from this cause compared to 1980, going from 1 503 to 3 674 deaths (mortality rate: 10.4/100 000 inhabitants in 2010).17,18
In the present study, alcohol abuse was the most common cause of cirrhosis in the analyzed population (40.90%), followed by autoimmune hepatitis (22.72%) and non-alcoholic steatohepatitis (18%), which coincides with the results reported by Asrani et al. ,16 who found that the main etiologies of this condition worldwide are chronic alcohol consumption, non-alcoholic steatohepatitis, and chronic hepatitis B and C virus infections.
Since Giannini et al.12 introduced the PC/SD ratio with a cut-off point <909 as a good predictor of the presence of EV in patients with cirrhosis, various studies have been conducted to analyze its effectiveness, yielding mixed results.
In Brazil, Mattos et al.,19 in a study conducted in 164 patients with cirrhosis (56.7% men) with an average age of 56.6 years and in whom the main cause of cirrhosis was viral infection (43.9%), found that the PC/SD ratio had a sensitivity of 77.5%, a specificity of 45.5%, a PPV of 79.5% and a NPV of 42.6%, and concluded that this is not a suitable method for the diagnosis of EV.
In Peru, Mosqueira et al.,20 conducted a study in 47 patients with cirrhosis with an average age of 60.7 years and in whom alcohol consumption was the main cause of cirrhosis (25.5%) and reported that the PC/SD ratio had a sensitivity of 40%, a specificity of 75%, a PPV of 82% and a NPV of 30%, concluding that the diagnostic effectiveness of this ratio is not acceptable.
In Cuba, Infante-Velazquez et al.,21 in a study of 102 patients with cirrhosis (54% men) with an average age of 55.8 years and in whom the main cause of cirrhosis was viral hepatitis, described that the PC/SD ratio had a sensitivity of 93%, a specificity of 45%, a PPV of 38.8% and a NPV of 97%, concluding that the cut-off point of 909 for this test was effective as a method to identify the presence of EV in their study population and that it is also an effective strategy for reducing health care costs and is therefore considered a safe alternative in countries with limited economic resources.
In Mexico, González et al.,22 in a cross-sectional study conducted in 91 patients with cirrhosis (55% men) with an average age of 53 years and in whom the main cause of cirrhosis was alcohol consumption (45%), found that the PC/SD ratio with a cut-off point of 884.3 had a sensitivity of 84%, a specificity of 70%, a PPV of 94% and a NPV of 40%, and concluded that this ratio is a good diagnostic tool.
Given the disparity in the reported results, Chen et al.,23 published a meta-analysis in 2017 that comprised 49 studies (22 prospective studies) in 6 274 patients with cirrhosis, whose condition was associated with alcohol consumption, schistosomiasis, and hepatitis B and C. The authors found that the cut-off point of the PC/SD ratio was <909 in 19 studies (38%), with a sensitivity of 84%, a specificity of 80%, an LR+ of 3.95 and an LR- of 0.23. Chen et al.,23 also reported that, despite the high heterogeneity of the results of the analyzed studies, the PC/SD ratio can be used to identify patients with EV, especially in cases of viral hepatitis cirrhosis, due to its high sensitivity.
Finally, Sami et al.,24 also in a systematic review and meta-analysis that comprised 21 studies (2 471 patients) aimed at identifying all primary studies that reported accuracy using EGD as the gold standard, found that 9 publications (823 patients) evaluated the PC/SD ratio, of which 5 had a cut-off point <909 and that sensitivity for this test was 87%, specificity was 71%, LR+ was 3.1, and LR- was 0.18. They concluded that this ratio is the most accurate noninvasive method for the diagnosis of EV.
The present study differs from those cited above in that women here made up the majority of patients (53%), viral etiology was the least common cause of cirrhosis (3%), and cirrhosis in most patients was related to diseases of immunological origin, such as autoimmune hepatitis (22.72%) and primary biliary cirrhosis (9.09%), followed by NASH (18.18%).
Similarly, most patients were classified as class A and class B on the Child-Pugh score (n=27 and n=27, respectively), the mean platelet count was >100x109/L, and the mean spleen diameter was 125.5mm, a figure close to the upper limit for the diagnosis of splenomegaly (120mm).
It should be noted that although the sensitivity, specificity, and NPV for the PC/SD ratio to detect EV (cut-off 909) were low, the PPV was high (88%), suggesting that there is a high probability of identifying patients with EV with a PC/SD ratio <909, but this is merely an assumption.















