Introduction
Throughout history, the training of health professionals has undergone significant changes, leading to new trends and challenges in medical education. To better understand this situation, this article will first discuss historical aspects of health science education and the various trends in teaching models and in the provision of health services that influence this type of education. The next section provides an overview of the numerous challenges that this field of education faces, as well as methods for dealing with them. Finally, it presents the conclusions on the panorama found.
Medical education is considered a subset of the teaching-learning-evaluation process used to train physicians, which aims to integrate the knowledge, experiences, skills, qualities, responsibilities, and values that qualify an individual to practice medicine. It is divided into undergraduate, postgraduate, and continuing education.1
The aim of this article is to reflect on the contextual factors that influence medical education in order to provide some recommendations based on the experience of the authors consulted, which can be applied in a critical and reflective manner when dealing with the challenges faced by physicians and may also be useful in other health professions.
Reports on health science education in the twentieth century
The education of health science professionals has deep historical roots in various societies, as described below.
During the early twentieth century, widespread improvements in medical education arose in response to the discovery of the hypothesis of pathogenic microbial organisms. For example, in the USA, reports such as the Flexner Report2, published in 1910; the Welch & Rose Public Health report3, published in 1915; and the Report of the Committee for the Study of Nursing Education4, published in 1923, paved the way for major changes in teaching of this area, as they established the scientific basis for teaching modern health sciences (public health, nursing, dentistry and related professions) in medical classrooms and laboratories.5
It should be noted that, in general, the aforementioned reforms were mainly based on the teaching of biomedical sciences, followed by training in clinical sciences and public health practices.
Three generations of reforms
From the preceding section, it is clear that understanding the evolution of health science education requires knowledge of the most relevant developments in the field during the twentieth century and subsequent years, which can be grouped into three generations of reforms, according to Frenk et al.6
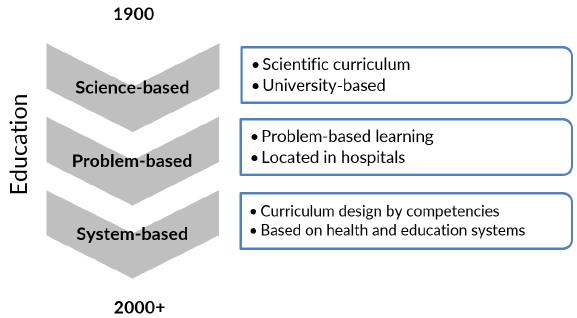
The first of these generations occurred at the beginning of the twentieth century and promoted a science-based curriculum at universities. The second took place in the mid-twentieth century, when teaching was taken to hospitals, and innovations such as problem-based learning (PBL) were introduced. Finally, at the beginning of the twenty-first century, changes were made to improve the performance of health systems by adapting to various contexts of professional competence (Figure 1).6
Historical debate topics in medical education
It is important to remember that there are issues that are constantly debated in medical education, such as: what role does theory play and how should it be balanced with practice?,7 who decides on the curriculum: the university or society?,8 what is the field of action of medicine and how should it be taught?, who sets the prerequisites for studying medicine and who certifies graduates?, where should medical students be trained?,9 is medical education an academic pursuit or just the preparation for a career? It is also essential to bear in mind that the answers to these questions depend on the social, political, cultural, and economic context of the place where they are formulated.10
Major trends in health care service delivery and pedagogy that have an impact on medical education
Following up on the historical analysis, some of the current trends in medical education and the delivery of health care services that have an impact on this type of education are presented below, along with the activities recommended for each trend (Table 1).
Table 1 Major trends in health care service delivery and pedagogy that have an impact on medical education.
| Trends | Recommended activities |
|---|---|
| 1. Demographic and epidemiological changes | Increasing outpatient and community practice Curricular changes such as increased emphasis on geriatrics |
| 2. Changes in medical knowledge, treatments, and technologies | Implementing an integrated and interdisciplinary curriculum Emphasizing professionalism, humanism, and ethics Including knowledge of information and communication technologies as core competencies |
| 3. Changes in health care delivery | Community-based education, not just hospital-based education Performing outpatient and community rotations Rural practices |
| 4. Changes in the roles of health professionals | Providing interdisciplinary and interprofessional education Promoting team-based learning Ensuring faculty development Promoting research in medical education |
| 5. Changes in the expectations and experiences of society and patients | Promoting a focus on health promotion Implementing a competency-based curriculum Emphasizing new evaluation modalities Implementing clinical simulation programs Using standardized patients |
| 6. Changes in the understanding of pedagogy and pedagogical technologies | Promoting problem-based learning Encouraging interaction between teachers, students, and patients in a virtual environment Promoting the training of students as if they were educators Ensuring patient participation in medical education |
Source: Own elaboration based on Aretz.10
Trend 1: Demographic and epidemiological changes
The epidemiology of diseases is rapidly and constantly changing around the world and, consequently, life expectancy is increasing in most populations.11 This is explained by the fact that, while acute diseases have not disappeared, the efficient and effective management of chronic conditions has become the primary focus of health care systems and modern medical education.12 The identification of successful experiences for teaching medical students in chronic care, the development of minimum skills for senior care, and the adoption of curricular approaches that stress outpatient and community care have all been suggested as ways to achieve this.13
In this context, medical education programs should incorporate geriatrics, both theoretically and practically, rather than teaching it as a separate discipline.14
Trend 2: Changes in medical knowledge, treatments, and technologies
Medical knowledge and technological advances have grown exponentially in recent years, so undergraduate medical education has had to look for the best way to teach this vast amount of specialized knowledge in a way that is both relevant to clinical practice and ensures that professionals act ethically and do not use these treatments and technologies for personal benefit. Curriculum integration is one of the strategies being considered to attain this goal, which attempts to shift this type of teaching from discipline-based to interdisciplinary.15
It is important to keep in mind that this attempt to integrate different disciplines is aimed at defining basic knowledge, essential skills, clinical reasoning and attitudes and experiences that are appropriate for all graduates16 and promote patient care.17
Another alternative for curriculum integration is the biopsychosocial model, which, unlike the biomedical model, aims to integrate theory with practice of biological, psychological, and social aspects related to patient care. Its main purpose is to produce "a whole that is greater than the sum of its parts"5, p 556 taking longitudinal topics into account, following a problem-based or clinical presentation approach through a continuum, and exposing students, from the beginning of their academic training, to the clinical,18 social and economic contexts of the patient, as well as to their experiences and to the family and social situations around them.
Concerning the teaching of professionalism, humanism, and ethics, it is important to note that these aspects are actually learned in the hidden curriculum,19 and hence their learning is primarily focused on role modeling, patient care, community activities, and the building of self-awareness.20
Another critical feature of medical education is the use of non-diagnostic and non-therapeutic health care technologies, such as information and communication technologies, particularly data banks, telehealth, and digital health.21 In this regard, it should be recalled that the World Health Organization (WHO), as reported by Pruitt & Epping-Jordan,22 stated that information and communication technologies are core competencies for health professionals.
Trend 3: Changes in health care delivery
In recent years, patient care has transitioned from in-patient to outpatient care due to advances in medical technology, the epidemiological transition from acute to chronic diseases, and the need to control health care costs.
Community-based medical education addresses needs such as producing relevant theoretical knowledge, providing students with experiences in primary care, instilling professional values, and positioning the understanding and practice of patient care beyond the individual level. In this regard, follow-up studies such as that of Dornan et al.23 show that students understand better the role of their profession and acquire better self-reflection skills with outpatient and community rotations because, as Borkan et al.24 state, they are in contact with the health care system, especially in the role of primary care, when they practice.
It is worth mentioning that one of the most significant and radical alternatives to community-based medical training has been the creation of new faculties, often located in the rural area, 25 either independently or as part of established universities.26,27
Trend 4: Changes in the roles of health professionals
Medicine and medical education have traditionally concentrated on the one-to-one relationship between physician and patient; however, it has become evident that the growing complexity of modern health care requires teamwork across disciplines and professions.28,29 Some studies aimed at hospital care in general,30 operating rooms, intensive care units, geriatrics and primary care31 have found that patients can have better recovery outcomes when medical practitioners are trained using an integrated, interdisciplinary32 and interprofessional team model.33,34
Similarly, the roles of non-medical health care professionals have evolved and expanded due to new technologies, new demands on the care system and changes in care in response to the multicausal origin of health disorders.
Another important change in medical education is that learning and teaching in small groups has become an essential element in both PBL and team-based learning, group project development and simulation-based training,35 or even in hospital ward teams. This is intended to encourage teamwork in preparation for medical practice because, while this learning has shown to improve individual training (since groups must solve problems and exchange knowledge during the process), it emphasizes the need for teamwork.36
With regard to teacher development in medical education, it is important to bear in mind that becoming an effective teacher is a process that requires both individual and institutional commitment and it is thus a critical aspect of promoting academic excellence and institutional vitality. In this sense, teacher training must encompass both formal and informal scheduled activities in real-world contexts, where learning is acquired through experience and reflective practice, individually, in groups, and in communities.37,38
In summary, it is imperative to keep in mind that the ongoing analysis of teaching development strategies in medical education can lead to excellence in health professionals when they assume roles as teachers, academic administrators, service providers, and researchers.39
Trend 5: Changes in social and patient expectations and demands
Society has redefined the role of physicians in the healthcare system (including their role in health promotion and disease prevention) in accordance with the WHO definition of health as "a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity."40, p. 1
Patients now have a better understanding of their care options due to increased access to information about services and research findings that analyze the effects of treatments and medical errors, allowing them to compare between chosen interventions and individualized care. This, in turn, has created the need for better control of the quality of medical education, the effectiveness of outcomes, and the evaluation of professional skills in healthcare staff.41
Similarly, the scenario described above has led to the development of performance-based and competency-based medical curricula42 that are well-defined and transparent to students and teachers. Furthermore, the design of such a curriculum ensures that students achieve their goals, that the developmental aspects of competencies are clearly defined, and that the evaluation process guarantees that competencies are demonstrated,6 including "reliable professional activities."43
Likewise, the assessment of students during their undergraduate studies in medicine has changed significantly and there is now a great deal of literature on the methods of evaluating the different competencies that are expected of these professionals.44 In this sense, it can be said that Miller's pyramid, which assesses the categories knows, knows how, shows how and does, has emerged as an efficient resource for evaluating students and medical professionals.45 However, some faculties still focus their efforts on evaluating the "does," that is, the last level of the pyramid.
Similarly, it is important to mention that standardized patients and simulation are increasingly used tools in the evaluation of medical students because of their efficiency since, for example, a structured objective clinical examination not only provides a standardized and controlled evaluation environment, but also allows students to practice and be observed in a safe environment of practice.46,47
Trend 6: Changes in the understanding of pedagogy and pedagogical technologies
Throughout the history of health science education, significant steps have been taken to understand learning theories, educational interventions, and the relationship between neurosciences.48 Two examples of these advances are tools such as concept maps, which aid clinical thinking and reasoning,49 and the experiential learning theory,50 based on which educational programs are designed. Moreover, in this process of evolution of medical education, special emphasis has been made on the application of psychological cognitive principles that promote the development of performances and competencies, which is an important objective of vocational education.51
PBL is another major advance in medical education; this is a teaching-learning method whose basic pedagogical principles relate to the activation of prior learning, learning in context, progress through additional experiences,52 the structuring of knowledge, motivation to learn, and the effects of group work. As for its effectiveness, in a literature review, Neville53 concluded that "graduates of PBL curricula demonstrate similar or greater professional competencies as compared to graduates of more traditional curricula." Similarly, Blake etal.54 found that utilizing evidence-based techniques improved scores on the national board exam, while Neville53 stated that knowledge acquisition is slightly weaker in those who learn through PBL, although its application in practice may be superior.
It has also been established that students who learn with the PBL methodology appear to perform better in situations of uncertainty and in the assessment of legal and ethical aspects of health care, in addition to having better communication skills and continuous self-directed learning.55.56
Furthermore, Ruiz etal.57 reported that learning in a planned virtual environment is gaining wide acceptance in medical education, as e-learning (including b-learning) has been found to be equivalent to traditional methods in terms of knowledge acquisition and retention.
Another aspect of medical education that has evolved is the training of students and residents as educators, because the responsibilities of health staff include teaching patients and peers, as well as tutoring students from previous years, which have become more important in recent years.58,59
In this regard, it is also important to encourage the participation of patients in medical education in areas that can directly affect them, such as the administration of health policies and professional policies, conducting social responsibility audits to higher education and health institutions, and educating other patients.60
Challenges of medical education
Quantity issues: According to the WHO,61 statistics show that there are not enough physicians globally to care for the entire population and that they are also poorly distributed; it also reports that this problem is more severe in middle- and low-income countries.62 It is important to note that the WHO considers that the ideal number of physicians per 10 000 inhabitants is 25 Quality issues: Likewise, regardless of the number of physicians available, they will not be able to improve the health of the population if they do not possess the necessary skills, are not technically competent and efficient, and are not trained to work in teams and adapt to different contexts.6,63,64Relevance issues: It is also important to keep in mind that even well-trained physicians may feel unable to solve health challenges because their training is not contextualized, that is, it is not targeted at the workplace where they are practicing and does not respond to changing policies, epidemiological transitions, and technologies used in professional practice.63Funding issues: Moreover, overall investment in medical education is insufficient, constituting a minimal proportion of national investment in most countries.
So, what are the options for addressing these challenges? Figure 2 presents some of the proposals made by Prideaux65 and Pulido et al.66 that may be useful in addressing the problems mentioned above.
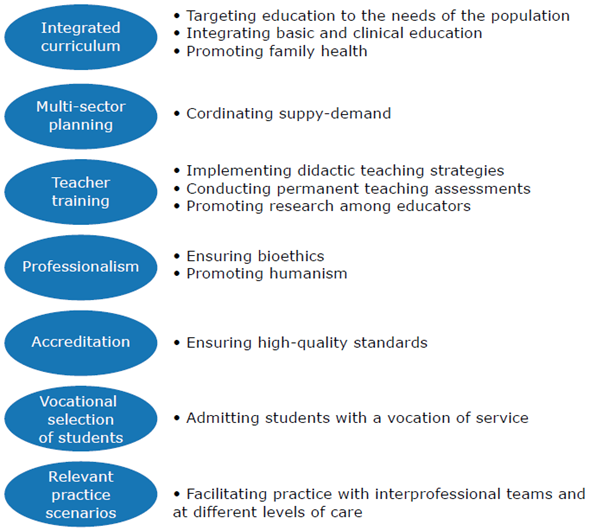
Source: Own preparation based on Prideaux65 and Pulido etal.66
Figure 2 Options to address the challenges of medical education.
It is important to note that the curricula of medical programs emphasize the areas of pathology, clinical, diagnosis and treatment of diseases, and therefore do not respond to the needs of the population; consequently, changes should be made to orient them towards local needs and to take into account epidemiological transition, morbidity and mortality, demographic characteristics, population requirements, and health services available at the local level.65
Similarly, as Larsen states,67 changes are required in medical curricula that integrate basic and clinical sciences, while also considering psychosocial and ethical aspects, health promotion, disease prevention and community development. Similarly, when implementing these changes, it is critical to ensure multisector collaboration and planning, i.e., there must be coordination between the education sector and local, regional and national authorities,68 in order to achieve harmonization between medical education, research, services and needs of the population.69
On the other hand, it is critical to consider the lack of teacher training, as educators use inappropriate methodologies that promote rote learning.67 In turn, the teaching-learning-evaluation process is based on standardized, teacher-centered and discipline-focused programs, as well as lectures delivered to large groups of students, limiting the use of active pedagogies. In this sense, it is essential to make changes so that the curriculum is student-centered, based on the PBL model, integrated, flexible, and community-based.65,70
Additionally, teachers must be trained in both disciplinary and pedagogical fields so that they can fulfill their roles as medical educators, academic administrators, and educational researchers,71 which is achieved through continuing education.72
Furthermore, the teaching of bioethics is inadequate in the current medical curricula because it sometimes fails to take into account values formation, student attitudes toward professionalism, teaching effective communication, patient rights,73 and even professionalism as such.74
Another area of medical education that has to be improved is the increase in the number of private medical faculties, which is associated with the economic growth of some countries and the laxity in the rules governing the incorporation of such schools. The problem with this lies in the lack of regulation, leading to the creation of low-quality programs75 in which quality standards and accreditation criteria that ensure excellence in education and health care are not met.76
Moreover, there is now greater emphasis on the training of medical-surgical specialists as a result of advances in knowledge in medicine and technological development, while interest in training in family physicians77 and public health specialists has declined. This is significant because, given the socioeconomic and health features of developing countries, these sectors are crucial to health care, and it is therefore critical that there is a balance between both trends.66
Similarly, educational institutions should establish broad criteria for student selection to recruit applicants representing the entire spectrum of society and choose people with a vocation for health care.78 In this regard, such criteria should include socio-economic, physical health and mental well-being aspects.
Apart from the above, in order to design an adequate health teaching curriculum, academic practice scenarios at all levels of health care should be available, including rural areas and vulnerable or low-income communities.25 Finally, collaboration between training institutions (supply) and health service providers (demand) is critical to ensure the effective and efficient delivery of health care.79
Conclusions
Socio-economic transitions, globalization, changes in population structure, epidemiological variations, and the demands of the population for better education and greater access to information have imposed changes in health and medical education systems. In addition, the training of health professionals has been influenced by the needs of the population, system requirements, and scientific progress.
Medical education has evolved historically from a scientific curriculum at the beginning of the twentieth century to a PBL-based curriculum in the second half of the same century; however, further changes are now required to ensure that training programs are based on current educational and health systems.
Medical education in many countries has failed to adapt to societal changes, making training institutions not only to lag behind in curriculum development and the application of new teaching and learning methodologies, but also to create conflicts in the training of physicians to provide appropriate health care and meet the needs of the population.
In this sense, given that the training of medical personnel has not responded to social requirements, there is a need for curriculum reforms to ensure that professional competencies meet the priorities of society. Thus, it is essential to bear in mind that the challenges of training in low- and middle-income countries relate to the number of physicians, the quality of medical education and the relationship of medical education with the health needs and expectations of the population: these countries need more physicians, but not always more of the same physicians. Nevertheless, it should be recognized that in Latin America, despite its socio-economic, political and administrative conditions, there are physicians who have contributed significantly to the advancement of science despite the lack of opportunities.
On the other hand, current health and education systems face other challenges such as the incongruity between vocational training, the need for health care, the low capacity for interprofessional and teamwork, the higher prevalence of hospital training over primary care, the imbalance in the labor market, and the lack of results in the welfare and health care of the community.
In this scenario, key recommendations for the future include educational and institutional reforms. The first concern refers to training in competencies, the implementation of PBL, interprofessional and teamwork, the use of new information and communication technologies, and the teaching of ethics and professionalism. The latter involves the joint work between the education and health sector; the creation of local, national, and global networks; the adequate use of resources; and the implementation of a quality control system and a permanent teacher training program.
In this regard, there is a need for a social, political, regional, and global interest to ensure that medical professionals have adequate training so that they can fulfill the purpose of providing appropriate and humane care to the population.