Introduction
The knee is the largest joint in the human body. It plays a fundamental role in processes such as walking and supporting body weight in a bipedal position. To adequately fulfill these functions, the knee has a unique structure formed from the relationship between the articular surfaces of the distal epiphysis of the femur (femoral trochlea, lateral and medial condyles), the proximal epiphysis of the tibia (lateral and medial condyles with their respective menisci), and the posterior surface of the patella. For that reason, said structure is classified as a trochlear synovial joint, which means that it enables the sliding of a concave surface over a convex surface, allowing for motions along a single axis, in this case, leg flexion and extension.1
Moreover, the knee has a ligamentous system responsible for guiding adjacent bone segments during joint motion and restricting translation by passive loading on the knee; this system comprises the medial and lateral collateral ligaments, as well as the anterior and posterior cruciate ligaments.1
The anatomy of the knee and its ligaments is well described in the literature; however, recent studies have revealed new structures related to this j oint, as is the case of the anterolateral ligament (ALL) of the knee. This ligament, as reported by Gómez-Cáceres et al.,2 was first described in 1879 by Dr. Paul Segond as a "pearly-white fibrous connective tissue" located in the anterolateral region of the knee that causes Segond fracture,2 a condition that affects internal rotation and anterolateral stability of the knee.3-4
Following the discovery of the ALL, several studies have been conducted in the fields of biomechanics, imaging, histology and anatomy,3 giving this structure different names, including lateral capsular ligament, medial lateral capsular ligament, bone-capsule layer of the iliotibial tract, and mid-third lateral capsular ligament; however, the most widely used and standardized term at the moment is anterolateral ligament, which was coined in 2007.3,4
According to the literature, the prevalence of the ALL is highly variable, since even an absence of up to 100% has been reported. For example, Runner et al.,5 in a dissection study that included 44 cadaveric human knees, identified it in 45.5% of the sample; Van de Watt et al.,6 in a systematic review that included 19 studies, found it in 96% of the 449 knees analyzed in all studies; Partezani-Helito et al.,7 in a descriptive laboratory study performed on 20 human cadaveric knees, found it in 100% of the sample; and, in contrast, Almeida-Fardin et al.,8 in a study that included 15 knees, did not identify this structure in any of the samples.
Knowledge of the morphometric characteristics of the ALL and its possible functions has led to the development of several techniques for reconstruction of this ligament and the anterior cruciate ligament (ACL),9-11 hence the relevance of studying it.
Given this panorama, the objective of the present study was to determine the prevalence of the ALL and its morphometric characteristics in a sample of Colombian human cadavers, in order to obtain local data that will allow conducting comparative studies in the area of morphology and the development of new and improved surgical strategies in the field of orthopedics based on the characteristics of the Colombian population.
Materials and methods
Study type and population
Cross-sectional study. The lower limbs of 15 previously numbered human cadaveric specimens were dissected and preserved in 7.6% formalin, alcohol, glycerin, and water. All knee joints that had not been previously dissected were included to guarantee the integrity of structures such as ligaments and tendons. The right knee of specimen number 8 was excluded from the sample due to loss of integrity of the structures adjacent to the joint under study, so only 29 knees were included, 15 left and 14 right.
Procedures
First, the sex of the corpses was determined and corroborated by identifying the external genital organs, ovaries and uterus in females, and the external genital organs and prostate in males, finding 14 male and one female cadaveric specimens. The second step was dissecting the knees using the following technique: first, the knee was placed in 30° flexion on the horizontal plane to identify the tendon of the biceps femoris muscle by palpation of the anterolateral aspect of the knee, and a 6-8cm long incision was made along the anterior border of this tendon; the dermal layer was then dissected, followed by the subcutaneous cellular tissue, until the external patellar retinaculum was reached. The inferolateral aspect of the superficial and deep layers of this retinaculum were then dissected to find the lateral collateral ligament (LCL), taking care not to cut it accidentally.
Once the ligamentous structure was identified, its proximal and distal insertion sites were recognized to measure its width and length. Longitudinal cuts, no deeper than 1-2mm, were made along the posterior border of the LCL to facilitate the search for the ALL and avoid the involuntary rupture of the latter. Photographs were taken of the specimens in which the ALL was recognized, and the length and width of this ligament were measured.
The measurements obtained in the dissections were recorded and analyzed in Microsoft Excel 2013, while statistical data were processed in SPSS version 21.
Ethical considerations
The material was obtained in accordance with the criteria defined in Decree 786 of 1990 of the Colombian Ministry of Public Health12 on clinical and medicolegal autopsies. Likewise, the study adhered to the ethical principles for medical research involving human subjects established by the Declaration of Helsinki.13
Results
The ALL was observed in 7 of the 29 knees analyzed (4 left and 3 right), resulting in a prevalence of 24.13%.
In the knees in which the ALL was observed, the proximal and distal insertion sites were identified, establishing that the ligament was inserted proximally on the anterolateral surface of the external femoral condyle and in an anterior direction with an oblique shape to insert distally on the anterolateral surface of the tibia (external tibial plateau), thus positioning anteriorly to the proximal insertion site of the LCL and proximally and posteriorly to the popliteus tendon (Figure 1).
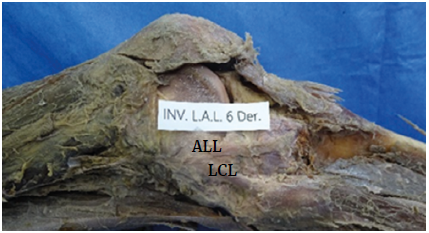
ALL: anterolateral ligament; LCL: lateral collateral ligament.
Source: Document obtained during the study.
Figure 1 Lateral region of the right knee.
The morphometric study found that the length of the ALL ranged from 24mm to 52.4mm, with an average of 37.34mm, and that the width at the middle third of the ligament ranged from 2.6mm to 6mm, with an average of 3.91mm (Figure 2 and Table 1).
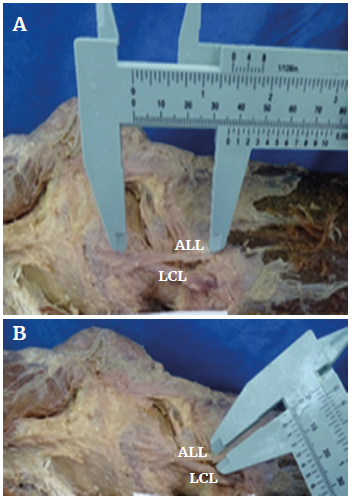
ALL: anterolateral ligament; LCL: lateral collateral ligament.
Source: Document obtained during the course of the study.
Figure 2 Measurement of the anterolateral ligament. A) length measurement; B) width measurement.
Table 1 Length, diameter, and central tendency measurements of the anterolateral ligament.
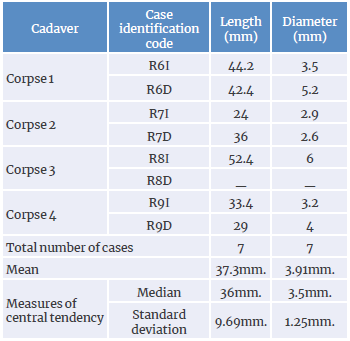
R: knee; I: left; D: right.
Source: Own elaboration.
Furthermore, the LCL was identified in 100% of the knees analyzed, and it was determined that its proximal insertion was located in the external femoral condyle and its distal insertion in the head of the fibula.
As with ALL, LCL length and width were measured to compare these measurements between knees with and without ALL; however, these measurements were excluded from the results because they did not have a reliable association.
Discussion
The LCA is essential for stability and proper rotational function of the knee;1 however, this function is not exclusive to this ligament, as other structures related to the biomechanics of the knee, such as the ALL, are unquestionably present (over half of the sample), as reported in several studies.7,9,11,14-22 In this sense, the present study found that the prevalence was 24.13%, a percentage evidently lower than the 100% described by Partezani-Helito et al.7 in a study carried out in Brazil in 20 knees, by Toro-Ibarguen14 in 34 knees in Spain, by Farhan et al.18 in 26 knees in India, by Vincent et al.19in 30 knees in France, by Daggett et al.20 in 52 knees in France, by Kennedy et al.21 in 15 knees in the United States, and by Caterine et al.22in 19 knees in Canada.
Likewise, the prevalence of ALL reported here is considerably lower than that described by Claes et al.16 in a study performed in France in 41 knees (97.56%), by Zhag et al.9 in 20 knees in China (90%), by Doods et al.11 in 40 knees in England (82.5%), by Capo et al.17 in 10 knees in the United States (80%), and by Cai et al. 15 in 16 knees in China (75%). Nevertheless, other authors have reported that this ligament has been observed in less than 50% of the sample, such as Runner et al.6 in a study conducted in Austria in 50 knees (45.45%) and Watanabe et al.23 in 94 knees in Japan (37.23%).
On the other hand, regarding the morphometric characteristics of the ALL, studies describing its measurements are scarce; however, among these, the studies of Partezani-Helito et al. ,7 Zhang et al. ,9 and Claes et al. stand out16 since they have reported the following length and width measurements: 37.3mm, 35.8mm (in extension) and 38.5mm (in extension), and 7.4mm, 11.3mm (femoral origin) and 8.3mm (femoral origin), respectively. Based on these values, it can be established that the world average length and width of the ALL is 35mm and 3.9mm, respectively, and that the averages found in the present study (37.3mm and 3.91mm) are similar.
One of the main strengths of the present study is that physicians specialist in morphology can use it as a guide to carry out comparative studies of the Colombian population and, as a result, develop new and improved surgical strategies in the field of orthopedics based on the feasibility provided by the characteristics of this population. On the other hand, one of the potential limitations is the scarcity of studies on the subject carried out in Colombia, which prevents contrasting the results reported here with data obtained in this population; thus, additional research, preferably with larger cadaveric samples, is necessary to confirm these findings.
Conclusions
The present study confirmed the existence of the ALL in the Colombian population; however, its prevalence (24.13%) is significantly low when compared to populations in countries such as France, India, China, USA, Canada, and Brazil, where it has been found in up to 100% of the samples analyzed.
This study also corroborated that, as described in the literature, the ALL is a pearly, resistant, fibrous band with an oblique trajectory from its proximal insertion on the anterolateral aspect of the external femoral condyle to its distal insertion on the anterolateral aspect of the external tibial plateau, and that the length and width averages found (35 mm and 3.9mm, respectively) are within the averages found worldwide, which demonstrates the low variability of the morphometric characteristics of this ligamentous structure among different populations.















