Introduction
Herlyn-Werner-Wunderlich (HWW) syndrome, also known as obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome since 2007,1 is a rare congenital malformation of the paramesonephric ducts characterized by uterus didelphys (uterovaginal duplication), obstructed hemivagina, and ipsilateral renal anomaly.2
The first case of uterus didelphys with obstructed hemivagina and ipsilateral renal agenesis was reported in 1922 by Purslow,3 and the second case was published by Wilson4 in 1925. Later, in 1971, Herlyn & Werner5 reported on a patient with simultaneous appearance of an open mesonephric duct cyst (Gartner's duct cyst), ipsilateral renal agenesis, and double uterus, and in 1976, Wunderlich6 reported the association of renal agenesis, bicornuate uterus with isolated hematocervix, and simple vagina.
The genitourinary system begins to develop embryologically during the fifth week of gestation. The paramesonephric ducts develop from the embryonic mesoderm to form the uterine tubes, migrate to the midline in the eighth week, and merge into the uterus, cervix, and upper vagina.7 When they fuse, they form a septum in the primordial uterovaginal canal, but if the reabsorption of that septum fails, various types of abnormalities may occur such as a uterus didelphys with hemivagina obstructed by the septum or septate uterus.8,9
During this formation process of the genitourinary system, the mesonephric ducts, besides giving origin to the kidneys, facilitate the fusion of the paramesonephric duct and are thus associated with changes in the regular ureteric bud and renal differentiation (with the consequent renal agenesis). When the mesonephric duct is absent, the paramesonephric duct shifts to the ipsilateral side and cannot fuse with the contralateral duct, resulting in uterus didelphys. Furthermore, because the displaced paramesonephric duct cannot contact the urogenital sinus, a blind sac forms, followed by an imperforate or obstructed hemivagina.10,11
Although the true prevalence of uterine malformations is unknown, it is estimated to be 1% among the general population and 3% in women with recurrent miscarriages. The most common paramesonephric duct abnormalities are septate uterus (55%) and uterus didelphys (11%).10,11 Moreover, in 75% of uterus didelphys and 25% of bicornuate uteri cases, patients also present with longitudinal vaginal septum, and when the vaginal septum is transverse or oblique, it causes obstructive hematocolpos.9 It should be noted that these abnormalities, mainly those related to uterus didelphys, are associated with renal tract malformations in up to 30% of cases.10,12
In 2001, Burgis13 reported that, although the incidence of paramesonephric duct abnormalities is unknown, it is believed to be between 0.1% and 3.8%. Later, in 2013, Tong et al.14 established that the mean age of diagnosis of HWW syndrome varies between patients with complete vaginal obstruction and incomplete vaginal obstruction, being 13.00t2.05 and 24.74t7.73 years, respectively.
In turn, the uterus didelphys related to HWW syndrome has an incidence that varies between 1 case per 2 000 women and 1 case per 28 000 women; likewise, renal agenesis is associated with 63-81% of uterine duplications and 92-100% of obstructed hemivagina cases.15,16
It has also been observed that renal agenesis is on the same side of the obstruction and that it is twice as common on the right side as it is on the left side in all cases of HWW syndrome.17 An association has also been found between this anomaly and asymmetry of labia minora.18
The diagnosis of HWW syndrome is usually made shortly after menarche and the initial symptoms are pelvic pain, dysmenorrhea, malodorous discharge, and pelvic mass.8 The gold standard for diagnosis is magnetic resonance imaging, although CT scans are also a useful alternative for this purpose, while ultrasound is used in the initial evaluation. As for treatment, management is surgical with resection of the septum and drainage of the blocked hemivagina.11,19
Patients with HWW syndrome should be closely monitored as complications such as endometriosis, pelvic adhesions, pyometra, pyosalpinx, intra-abdominal abscesses secondary to trauma from sexual intercourse, and neoplasms may occur; therefore, early diagnosis and treatment are essential for a good prognosis, hence the importance of reporting cases of this condition.
The following is the case of a patient diagnosed with HWW syndrome who received surgical treatment and had a satisfactory recovery.
Case presentation
A 22-year-old university student from Samacá, Boyacá (Colombia) visited the gynecology service of a secondary care center in the municipality of Sogamoso, Boyacá, due to a 9-year history of irregular menstrual cycles, amenorrhea of up to 8 months, heavy bleeding, dysmenorrhea, and pelvic pain. No abnormal findings were reported on physical examination. The young woman reported that the symptoms began at the age of 13 with menarche.
At age 19, in September 2016, the patient underwent a transvaginal ultrasound in which bilateral micropolycystic ovaries and cervix displaced by an image suggestive of a 30x30mm vaginal wall cyst were observed; the uterus was not described in the report. Based on these findings, a 6- to 10-month course of vitamin E and metformin was initiated for the management of polycystic ovary, but no improvement was observed. Additionally, she was prescribed contraceptives (monthly injections), which she received for approximately 14 months, successfully regulating her menstrual cycle for a while, but with subsequent recurrence of initial symptoms.
In August 2017, a transvaginal ultrasound showed an increase of approximately 1 cm in mass size; 2 months later, an abdominal ultrasound showed polycystic ovaries, absent right kidney, uterus didelphys, and 20 cm3 of vaginal vault fluid collection. Due to the non-specific characteristics of the mass and its progressive growth, an MRI of the pelvis was performed in October 2018, finding uterus didelphys, multiple small cystic formations in both ovaries, left cervical canal of normal appearance, and right cervical duct with a 35x32x39mm hyperintense space-occupying lesion in T1 sequence and a diffuse and heterogeneous increase of the lesion in T2 sequence (Figure 1). It should be noted that approximately one year elapsed between the performance of the abdominal ultrasound clinical and imaging findings, HWW syndrome was not and the MRI due to administrative delays. Despite these initially considered as a differential diagnosis.
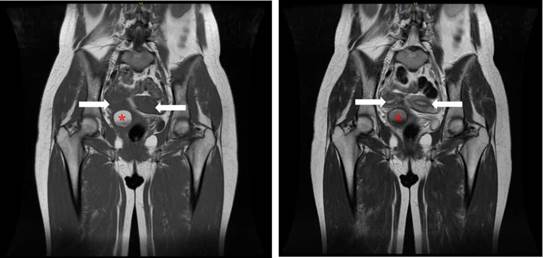
Note: The asterisk indicates a space-occupying lesion (hematocolpos), while the arrow indicates a uterus didelphys.
Source: Document obtained during the study.
Figure 1 Pelvic MRI in T1 and T2 sequence.
In 2019, the patient attended the outpatient gynecology service of a secondary care hospital, where, based on imaging results, it was considered that she met the diagnostic triad for HWW syndrome. She underwent a colpotomy plus resection of a non-invasive paracervical mass of approximately 60x60mm located on the right side and resection of the vaginal septum, with drainage of 100cm3 of brown blood material.
Two months after this procedure, a follow-up ultrasound was performed, showing no acute pathological alterations; on that occasion, the patient reported significant improvement in symptoms, regular menstrual cycles lasting 4 to 5 days, change in bleeding coloration (less dark), disappearance of pelvic pain, decrease in dysmenorrhea, and improvement in mood.
Finally, at a check-up 10 months after surgery, the patient reported that she was pregnant, had no complications, and felt healthy and asymptomatic.
Discussion
Bicornuate uterus and uterus didelphys are Class III and IV paramesonephric duct abnormalities according to the American Fertility Society classification19 (Figure 2) and are difficult to differentiate, even using magnetic resonance.8
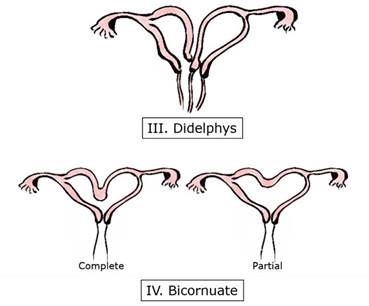
Source: Own elaboration based on The American Fertility Society.19
Figure 2 Classification III and IV of uterine malformations.
According to Fedele et al.,20 in most cases (72.4%), HWW syndrome presents with a classic variant involving a uterus didelphys, unilateral genital obstruction, and ipsilateral renal abnormality, as in the reported case; however, in the remaining 27.6% of cases, rare variants with different therapeutic implications have been described.
Various classifications for HWW have been established in the literature, such as the one proposed by Zhu et al.21 (hemivagina completely obstructed or not), or the 3 types described by Bian et al.22 (type I: imperforate oblique vaginal septum, type II: perforated oblique vaginal septum, and type III: imperforate oblique vaginal septum and cervical fistula) (Figure 3). These classifications are rarely used, but they demonstrate the variability in the presentation of the syndrome.23
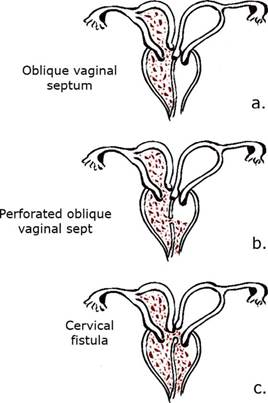
Source: Elaboration based on Wang et al.23
Figure 3 Classification of Herlyn-Werner-Wunderlich syndrome according to Bian et al.
Patients with HWW syndrome are usually referred to the gynecology service after menarche due to pelvic pain, dysmenorrhea, foul-smelling discharge, and pelvic mass. These symptoms are often mistaken for inflammatory and infectious pelvic disorders, so they are prescribed anti-inflammatory drugs, contraceptives, and/or antibiotics that relieve symptoms but delay diagnosis.24,25 However, cases of successful prenatal diagnosis of HWW syndrome have been reported as early as the 25th week of gestation, when the fetus is under the influence of maternal and placental hormones.16 In these cases, a retrovesical cystic lesion (hydrocolpos) secondary to obstruction due to vaginal discharge is detected, as well as unilateral renal agenesis.26
Ultrasound is used in the initial assessment for the diagnosis of this syndrome; it detects hematocolpos as a rounded hypoechoic mass with smooth walls and absent flow in Doppler images, and it also identifies renal agenesis and uterus didelphys, as in the case reported here. While computed tomography is another option for diagnosing HWW syndrome,11 numerous studies have demonstrated that MRI is the most accurate imaging method, reaching even 100% accuracy.7,8 When the latter is not diagnostic or when an experienced radiologist is not available, a laparoscopic assessment of the pelvic anatomy should be considered in order to establish the diagnosis.15
Although surgical correction of the obstructive vaginal septum with resection and drainage is the preferred treatment for HWW syndrome,11,26 endoscopic ablation of the vaginal septum has been documented as an alternative to conventional open surgical excision.25 Regarding endometriosis, it has been established that laparoscopic removal alleviates pain and improves fertility and quality of life.21
It should be noted that in patients with obstructive cervical morphology, there is an increase in the complexity and postsurgical risk of contracture, stenosis, infection, and need for reoperation. Days & Jogo25 report that vaginal packing, vaginal dilators and stents are useful in these cases to maintain vaginal permeability. Although hysterectomy is not recommended to treat HWW syndrome because it is an invasive method and reduces the pregnancy rate, it can be considered in specific cases, such as severe infection.23,25
With regard to complications secondary to paramesonephric duct abnormalities, endometriosis rates of 17-35% have been reported in women with uterus didelphys, being higher when there is complete hemivaginal obstruction.14,27 Cases of endometrioid adenocarcinoma not associated with human papillomavirus in the semi-obstructed cervix and clear cell carcinoma on the obstructed side of the vaginal wall have also been reported.28
As for obstetric complications, Capello et al.1 report that they occur in 25% of women with paramesonephric duct abnormalities, such as primary infertility due to endometriosis and pelvic abscesses.
In patients with HWW syndrome without comorbidities, there is a greater chance of successful pregnancy, and the rate of miscarriage is not significantly different from that of the general population. However, an increased risk of preterm delivery, premature rupture of membranes, fetal growth restriction and fetal mal-presentation at delivery has been documented in these patients.15,29 It should be borne in mind that uterus didelphys is not an indication for cesarean delivery if there is no canal obstruction30 and that pregnancies on the side of the obstruction are not frequent.31
Finally, it is important to keep in mind that pelvic examinations in adolescents or virgin women may be significantly limited.15 Therefore, gonadotropin-releasing hormone analogs may be a good option for maintaining amenorrhea, especially in cases complicated by cervical atresia.14 For instance, in the reported patient, contraceptives temporarily alleviated symptoms, making them a viable option while awaiting surgery.
Conclusions
HWW syndrome is a rare malformation that should be considered as a differential diagnosis in women of all ages who have abnormal paramesonephric ducts and present with pelvic pain, dysmenorrhea, and a mass in the genital tract, as early diagnosis and treatment can decrease the incidence of complications and significantly improve obstetric prognosis and quality of life of these patients by reducing the severity of symptoms. For example, the patient in the present case reported resolution of symptoms only months after surgery and pregnancy in less than a year.
The gold standard for the diagnosis of HWW syndrome is magnetic resonance; however, as shown in this case, abdominal ultrasound can also detect the triad that characterizes HWW syndrome.















