Introduction
Stevens-Johnson syndrome (SJS) is a disorder that causes oral, ocular, and genital mucocutaneous rash,1 with an annual incidence of 1.2-6 cases per million inhabitants , with women being more affected than men (1.5 :1).2 Patients with SJS have epidermal desquamation on less than 10% of their body surface, and, in some cases, desquamation may occur as a secondary lesion at the end of the disease process. It is essential to keep in mind that when lesions are present in 10-30% of the skin, there is an overlap between SJS and toxic epidermal necrolysis (TEN), but when this percentage exceeds >30%, itis considered to be TEN (also known as Lyell' s syndrome), a potentially life-threatening condition.
Mortality from SJS depends on the time of reaction onset, the extent of epidermal detachment, the patient's age, and underlying conditions. From the least to the most severe degree of skin involvement, mortality is almost 10% for patients with SJS, approximately 30% for patients with SJS/TEN overlap, and almost 50% for patients with TEN. It should be noted that SJS and TEN are considered two clinical spectrums of the same disease.4
At present, the etiopathogenesis of SJS has notbeen fully elucidated, althoughithas been associated withmalignancies (leukemia, lymphomas), autoimmune diseases (systemic lupus erythematosus, rheumatoid arthritis, Sjogren's syndrome, Hashimoto's disease, and sarcoidosis), drug reactions, and genetic (HLA antigen alleles), immune and infectious factors (herpes simplex virus (HSV) 1 and 2, herpes zoster, Epstein-Barr virus, cytomegalovirus, herpesvirus 6,7and 8, HW,Mycoplasma pneumoniae,Chlamydiapneumoniae, Mycobacterium tuberculosis and Candida spp.)5-12
SJS may be defined based on the involvement of two or more mucous membranes or calculating the percentage of body surface area affected. When symptoms appear, erythematous macules, which turn purplish - red and then grayish, are seen; flaccid and painful blisters eventually form, predominantly on the face and trunk. The so-called "target lesions" or "iris lesions" are observed in SJS, which can have three presentations: (i) typical raised target lesion (two concentric erythematous rings or circles over a central zone), (ii) atypical raised target lesion (a single raised, concentric erythematous ring or circle over a central point), and (iii) flat atypical target lesion (one or two flat concentric erythematous rings or circles over a central point). If symptoms progress to TEN, the Nikolsky' s sign can be recognized, in which the epidermis is detached from the deeper layers of the skin when massaging or rubbing the skin.12
The following is the case of a patient who developed SJS with reactivation of herpes simplex following paracetamol ingestion.
Case presentation
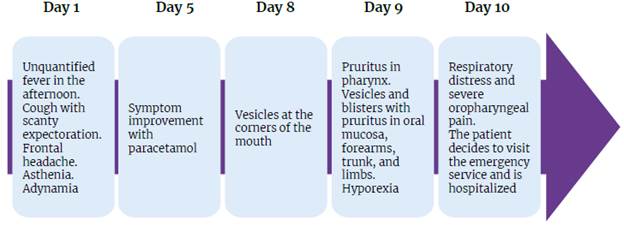
A 20 -year- old patient attended the emergency department of a tertiary care center in Popayán due to a 10 -day history of asthenia, adynamia, unquantified fever predominantly in the afternoon, episodes of cough with scanty whitish sputum, and episodic tension headache in the frontal region with intensity of 6/10 on the analogue scale of pain for 10 days; the symptoms improved after taking 1g of paracetamol, which the patient self-medicated on the fifth day of symptom onset.
On the eighth day, the patient presented vesicles in the corners of the mouth of 1-2 mm in diameter, and the next day he developed a sensation of pruritus in the pharynx and hyporexia, as well as vesicles and blisters accompanied by pruritus in the oral mucosa, forearms, trunk, and limbs. On the tenth day, he presented with an episode of odynophagia and respiratory distress, so he decided to visit the emergency department, where he was hospitalized (Figure 1).
His personal medical history included chickenpox and measles during childhood; two episodes of oral herpes in the last seven years, which were satisfactorily treated with topical acyclovir; and allergy to apitoxin and soaps with salicylic acid and glycolic acid in their composition. In addition, the patient denied the use of drugs other than paracetamol and stated that he had a stable heterosexual partner and usedbarrier methods asa contraceptive method.
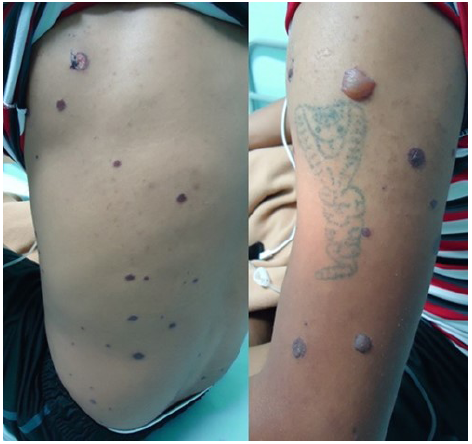
Upon physical examination on admission, he had the following vital signs: heart rate of 106 bpm, blood pressure of 130/70 mmHg, respiratory rate of 22 rpm, temperature of 36.5°C, and blood glucose of 135 mg/dL. Erythema and epiphora were also evident in both eyes, as well as extensive erosion in oral and nasal mucosa with erythema, hemorrhagic crusts in the vermilion zone, sialorrhea (Figure 2), and multiple vesicles and blisters in the thoraco-abdominal region and limbs along the dermatomes, of which some had a dark violaceous or hypochromic center and erythematous halo (Figure 3). The genital examination showed erosion of the glans and foreskin. No further alterations were found during the examination.
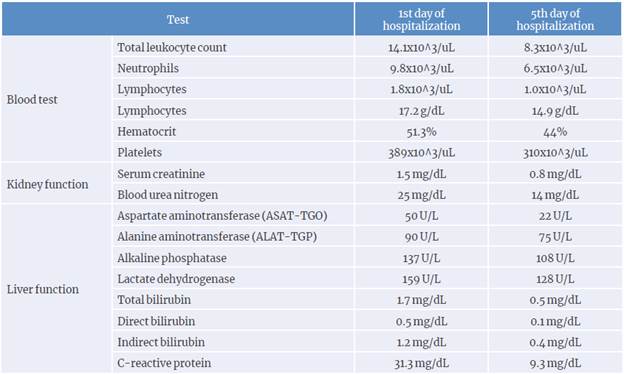
The initial diagnostic impression was disseminated herpes simplex with possible immune involvement, so it was decided to hospitalize the patient and perform achest X-ray that showed no alterations, in addition to a blood count that reported normal electrolyte levels, leukocytosis with neutrophilia, and elevated serum creatinine, blood urea nitrogen and C-reactive protein (CRP) levels. Laboratory tests were also requested, including a rapid test for HIV 1 and 2, serological test for syphilis, and hepatitis B test (Table 1). A dermatology assessment was also performed.
Initial treatment consisted of maintenance intravenous fluids, prophylactic antibiotics (ampicillin sulbactam 3g IV every 6 hours), fluconazole 200mg IV every 24 hours for prophylaxis of opportunistic infections, acyclovir 500mg IV every 8 hours, analgesics (tramadol 25mg IV every 6 hours, and dipyrone 1g IV every 8 hours), and ranitidine 50mg IV every 8 hours for gastric protection. Mouth rinses with nystatin 10mL every 6 hours were also prescribed.
On the second day of hospitalization, the patient was assessed by the dermatology service once again, establishing a differential diagnosis between SJS and systemic lupus erythematosus (SLE). Consequently, a skin biopsy and the following tests were requested: antinuclear antibodies, anti-DNA antibodies, C3 and C4 proteins, lupus anticoagulant, perinuclear anti-neutrophil cytoplasmic antibodies (p-ANCA), antineutrophil cytoplasmic antibodies (c-ANCA), and anti-cardiolipin antibodies. Immunological profile was negative, and HIV, syphilis and hepatitis B were ruled out.
Based on the f findings, paracetamol and prophylactic antibiotic and antifungal medication were stopped, and the patient was treated with methylprednisolone 50mg IV every 8 hours, artificial tears, and sucralfate suspension 5mL every 6 hours. After five days of hospitalization, control blood, kidney and liver function, and CRP tests were performed, showing improvement compared to the values obtained on the day of admission (Table 1).
The patient had a satisfactory progress and was discharged after 10 days of hospitalization. During subsequent follow-up appointments (at two weeks with the internal medicine service and at two months with the dermatology service), he was found in good general condition, although there was evidence of dyschromic macules in the thorax without ocular or genital involvement in the last consultation.
Discussion
The diagnosis of SJS is based mainly on clinical findings (fever, involvement of two or more mucous membranes, and <30% involvement of the body surface), with biopsy and histological examination being required for confirmation. It is worth noting that in the case reported here, these parameters were met, but the histopathology photograph could not be included in the report due to administrative complications with the laboratory.
According to the literature,14 the pathology study in SJS cases reports initial lesions with superficial perivascular lymphocytic infiltrate, together with dermal edema, accumulation of lymphocytes along the dermoepidermal junction, and degenerative and necrotic keratinocytes (interface dermatitis pattern). As the syndrome progresses, lymphocytes ascend to the epidermis and there are confluent, demarcated areas of epidermal necrosis with blister formation leading to epidermal detachment. Macroscopically, the lesion observed is a typical target lesion (blister or area of central epidermal necrosis surrounded by macular erythema), as evidenced in the case reported here (Figures 2 and 3).
Although the patient in the present case only had some dyschromic macules on the thorax as sequelae, in 90% of the cases there are evident ocular complications.1,15
Systemic manifestations in SJS include a discrete elevation of transaminases, altered kidney function test, and intestinal and respiratory symptoms with sphacelation of the epithelium.15,16 In the reported case, the liver profile was slightly elevated, and renal function alteration, leukocytosis with neutrophilia and elevated CRP were determined, all of which were attributable to the systemic inflammatory response. Even though there is usually pulmonary involvement (alveolar lesion) in one third of the cases of this syndrome,13 the patient in this case had no respiratory complications and the chest X-ray showed no alterations.
The acute phase of SJS is marked by nonspecific symptoms (fever, myalgias, arthralgias, ocular irritation, odynophagia, and cough) that appear days before the onset of cutaneous manifestations, as was the case of this patient. Furthermore, in more than 90% of cases, erosions appear in the oral, nasal, ocular and/or urogenital mucosa, which in severe cases also involve the respiratory and gastrointestinal mucosa.12,16 This patient had lesions on less than 30% of the body surface, which, as noted above, is a characteristic of SJS. Because SJS and TEN can overlap, they are considered to be within the spectrum of the same disease and should not be mistaken for erythema multiforme minor, which is more of an antiherpetic reaction than a drug allergy.13
The concomitant infectious component of herpes simplex reactivation as a predisposing factor for SJS is interesting since it has been linked to the family of human herpes viruses by various authors since the 1980s (HSV 1 and 2, varicella zoster, Epstein-Barr virus, cytomegalovirus, and herpesviruses 6, 7 and 8.)17-22 However, according to Irungu et al,23various analytical epidemiological studies have been conducted since 2015, showing conflicting results and attributing 94.8% of SJS/TEN cases to drug usage and only 5.2% to infectious agents (HIV, HSV 1, and M. pneumoniae).
Furthermore, by 2013, the Food and Drugs Administration had already issued a report on the risk of rare but severe skin reactions, such as SJS, TEN, and acute generalized exanthematous pustulosis following paracetamol consumption.24 Other studies have also described the association of SJS with more than 100 drugs (including paracetamol),25-28 most notably EuroSCAR, which monitored the risks of SJS/TEN as a drug reaction through case-control studies (Table 2).28 It should be noted that the patient in the present case consumed paracetamol five days before consultation.
Table 2 Drugs with a risk of causing Stevens-Johnson syndrome/toxic epidermal necrolysis.
| High risk | Low risk | Potential risk * | Undetermined risk |
|---|---|---|---|
| Nevirapine | Beta-blockers | ||
| Lamotrigine | Paracetamol | Angiotensin-converting enzyme | |
| Carbamazepine | Sertraline | Corticosteroids | inhibitors |
| Phenytoin | Macrolides | Acetylsalicylic acid | Calcium channel blockers |
| Phenobarbital | Quinolones | Pyrazolones | Thiazide diuretics |
| Sulfonamides | Cephalosporins | Tramadol | Furosemide |
| Allopurinol | Tetracyclines | Ibuprofen | Propionic acid |
| Sulfasalazine | Aminopenicillins | Pantoprazole | Insulin |
| Nonsteroidal anti-inflammatory | Nimesulide | Antidiabetic sulfonylureas | |
| drugs (oxicams) | Proton pump inhibitors |
* Further evidence required.
Source: Own elaboration based on Mockenhaupt et al.28
In cases of SJS, laboratory tests are necessary to determine whether there is systemic involvement, and the Score of Toxic Epidermal Necrosis (SCORTEN) test is useful to establish the severity and risk of mortality (Table 3). However, this score does not consider possible concomitant infections and immune involvement, which have been reported to be predisposing factors in the pathophysiology and natural history of SJS/TEN. After assessing all items, except bicarbonate, the reported patient had a systemic involvement of 3.2%; it is important to mention that arterial blood gas tests were not performed due to an infectious process at the puncture site.
Table 3 Independent prognostic factors in Stevens-Johnson syndrome/toxic epidermal necrolysis: each parameter is assigned 1 point.
| Age | >40 years |
|---|---|
| Heart rate | ≥120 bpm |
| Diagnosis of malignancy | Yes |
| Body surface with detachment on the first day of admission | >10% |
| Blood urea nitrogen | >28 mg/dL |
| Bicarbonate | <20 mg/dL |
| Glucose | >252 mg/dL |
| SCORTEN (mortality rate) | 0-1 (3.2%) 2 (12.1%) 3 (35.3%) 4 (58.3%) >5 (90%) |
Source: Own elaboration based on Bastuji-Garin et al.29
The main differential diagnoses of SJS/TEN are fixed erythema pigmentosum, bullous skin diseases (pemphigoid, erosive lichen planus), SLE (Rowell syndrome), Behcet's disease, linear IgA dermatosis, and staphylococcal scalded skin syndrome.12,30 31 It should be noted that, although several authors have reported the association of SLE with SJS/TEN,30,32-34 the patient was negative for immunological profile.
The Centers for Disease Control and Prevention state that it is not mandatory to screen for HSV 1 or 2 in the general population; however, one of its indications is to perform serology tests in patients with a clinical diagnosis of active HSV 1 or 2 infection and no confirmatory test.35,36 This is mentioned because, due to administrative difficulties with the health care delivery company, it was not possible to request antibody tests, cell culture or Tzanck test, nor was it possible to perform polymerase chain reaction to confirm the concomitance of these virus -es with SJS, despite the symptoms being very suggestive.
The limitations of this study include the fact that it was not possible to attach the histopathology image and that, as mentioned above, due to administrative reasons, arterial blood gas tests were not performed, nor were serology, cell culture, Tzanck test or molecular tests for HSV 1 and 2 and other herpesviruses.
Conclusions
The development of SJS may be associated with the consumption of paracetamol; however, its use is not discouraged due to its great overall benefits. In this sense, given that paracetamol is an over-the-counter drug widely used in Colombia and that it is also classified as a potential risk in the EuroSCAR study, it is essential to recognize the clinical manifestations of SJS to provide adequate treatment and avoid complications in cases such as the one reported here.