Introduction
Central nervous system tumors are frequent in the pediatric population, accounting for 20% of all neoplasms in children under 18 years of age; 40% of these occur in the posterior fossa.1,2 The primary histologic subtypes of posterior fossa tumors are medulloblastoma, pilocytic astrocytoma, diffuse midline glioma, ependymoma, and atypical teratoid/rhabdoid.2,3
Currently, the World Health Organization (WHO) (cited by Wesseling & Capper4) recommends classifying posterior fossa tumors according to their phenotype (histology) and genotype (molecular characterization); however, in some countries such as Colombia, the molecular studies necessary to achieve such characterization are not yet routinely performed. In view of the foregoing, and given the histological heterogeneity of posterior fossa tumors, a proper imaging characterization of these neoplasms is essential to develop an adequate therapeutic approach.2,3
Magnetic resonance imaging (MRI) is the test of choice to study posterior fossa tumors; nevertheless, structural findings can be nonspecific when classifying them and differentiating their possible histological grades, especially in scenarios that may represent a diagnostic challenge, such as differentiating between a pilocytic astrocytoma and a medulloblastoma.1 In this regard, it is critical to assess the usefulness of radiological findings derived from advanced MR imaging, such as the DWI (diffusion-weighted imaging) sequence and the ADC (apparent diffusion coefficient) map, which provide functional information on tumor behavior and help establish an adequate differential diagnosis that allows predicting the histological subtype of the tumor.5-9
Given this scenario, the objective of this study is to determine the usefulness of apparent diffusion coefficient values (quantitative ADC) for the differential diagnosis of posterior fossa tumors in a pediatric population of a reference hospital in Bogotá, D.C., Colombia.
Materials and methods
Study type and population
Diagnostic validity study. All pediatric patients who were diagnosed with posterior fossa tumor at the Fundación Hospital Pediátrico de La Misericordia (quaternary care center) between 2017 and 2019 and underwent MRI with DWI sequence that allowed measuring quantitative ADC values (N=30) were selected. Patients whose diagnosis was not confirmed by histological analysis and in whom MRI scans could not be obtained were excluded, leaving a final sample of 28 participants (Figure 1).
Procedures
Information was collected from the Picture Archiving and Communication System (PACS) reports accessible in DICOM file format in the medical records of the Fundación Hospital Pediátrico de La Misericordia database.
The diagnostic images of the patients were obtained using a Philips Multiva 1.5T (Tesla) MRI system in accordance with the institutional pediatric neuro-oncology protocol that includes, but is not limited to, DWI sequence with b0 and b1000 factors, and axial ADC map with values of 10-3mm2/s.
A radiologist with experience in pediatric neuroimaging estimated the median quantitative ADC value at their workstation and without knowing the final histopathological diagnosis. For this measurement, areas of interest of 5-10mm established by manual technique were used in the solid tumor area, which was visually identified as the area with lower signal intensity (Figures 2 and 3). It should be noted that having diffusion restriction has traditionally been considered a qualitative item and that there is diffusion restriction on an MRI scan when 2 conditions are met: i) having hyperintense appearance in the DWI sequence and ii) having hypointense appearance in the ADC map.
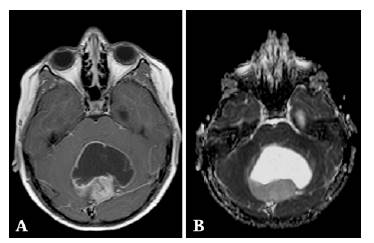
Source: Document obtained during the course of the study.
Figure 2 Midline posterior fossa mass with solid and cystic component. A) Axial post-gadolinium T1W-SE: the solid component shows avid postcontrast heterogeneous enhancement and no diffusion restriction (not shown); B) axial ADC map: median quantitative ADC value: 1.62 x10-3mm2/s. Histopathological diagnosis of pilocytic astrocytoma.
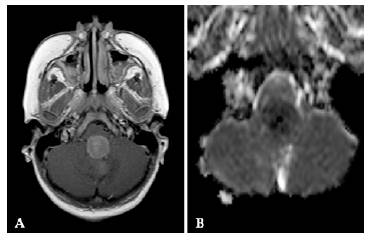
Source: Document obtained during the course of the study.
Figure 3 Solid mass in the midline of the posterior fossa occupying the fourth ventricle. A) post-gadolinium axial T1W-SE: the solid component exhibits avid post-contrast enhancement and peripheral diffusion restriction (not shown); B) axial ADC map: median quantitative ADC value: 0.210x10-3mm2/s. Histopathological diagnosis of medulloblastoma.
Statistical analysis
Sensitivity, specificity, and positive and negative predictive values were obtained and processed using STATA and SPSS statistical software and compared with histopathological diagnosis as the gold standard for phenotypic tumor characterization.
Differences between medians were determined using the Kruskal-Wallis test. The p-value between the quantitative ADC value and the gold standard was calculated using the Pearson's chi-squared test, with a statistical significance level of p<0.05.
Ethical considerations
The study took into account the ethical principles for medical research involving human subjects established by the Declaration of Helsinki10 and the scientific, technical and administrative standards for health research of Resolution 8430 of 1993 of the Ministry of Health of Colombia.11 The research was approved by the Ethics Committee of the Fundación Hospital Pediátrico de La Misericordia, in accordance with Minutes No. CEI 201-19 of May 27, 2019.
Results
Epidemiological characterization
The mean age of the participants was 83.9 months, with a standard deviation (SD) of 57 months, and the majority (64.28%, n=18) were male. Medulloblastoma was the most common tumor (39.29%, n=11), followed by pilocytic astrocytoma (32.14%, n=9) (Table 1).
Imaging features
Based on the largest diameter of the lesion, the average tumor size was 42.8mm, with a SD of 15.4mm.
71.42% of tumors infiltrated into adjacent structures, 85.71% had structural signs of mass effect with adjacent tissue displacement, 67.85% were considered heterogeneous (cystic component, calcifications, and blood traces), and 78.57% had signs of intra- or perilesional vasogenic edema.
Following the administration of intravenous paramagnetic contrast agent, 71.43% of neoplasms showed heterogeneous enhancement patterns; 17.86% showed homogeneous enhancement; and 10.71% showed no significant enhancement. Leptomeningeal enhancement suggestive of meningeal spreading was also detected in three patients.
Qualitative restriction to the movement of water molecules in the DWI sequence and ADC map occurred in half of the lesions evaluated.
Comparison between the median values of the quantitative ADC map and the qualitative DWI restriction variable showed a statistically significant difference (p=0.0001): the median quantitative ADC value was approximately 0.57 10-3mm2/s in patients with qualitative restriction, whereas it was 1.645 10-3mm2/s in those without qualitative restriction in the DWI sequence with factors b0 and b1000.
The mean value of quantitative ADC for all histologic types and grades included was 1.09 10-3mm2/s, with a SD of 0.65 10-3mm2/s.
Statistical analysis between the quantitative ADC variable and tumor histology (gold standard), performed with the non-parametric Kruskal-Wallis test, demonstrated statistical significance (p<0.05) for the diagnosis of medulloblastoma and pilocytic astrocytoma (Table 2).
Table 2 Median apparent diffusion coefficient based on histological diagnosis.
| Histological diagnosis | Median quantitative ADC (x10-3mm2/s) | p-value |
|---|---|---|
| Medulloblastoma | 0.56 | 0.001 |
| Tumor other than medulloblastoma | 1.16 | |
| Pilocytic astrocytoma | 1.71 | 0.0054 |
| Tumor other than pilocytic astrocytoma | 0.63 | |
| Diffuse midline glioma | 1.62 | 0.05 |
| Tumor other than diffuse midline glioma | 0.66 | |
| Ependymoma | 0.63 | 0.23 |
| Tumor other than ependymoma | 0.97 | |
| Teratoid/Rhabdoid | 0.79 | 0.9 |
| Tumor other than rhabdoid-teratoid | 0.95 |
Source: Own elaboration.
Diagnostic performance of the quantitative ADC value
The quantitative ADC value that, collectively, had the highest sensitivity and specificity to indicate the histological type of tumors with statistically significant difference (medulloblastoma and pilocytic astrocytoma) was established as the best cut-off point for this purpose. Thus, a quantitative ADC value <0.6210 x10-3mm2/s was the best diagnostic performance for detecting medulloblastoma, while a value <1.03 x10-3mm2/s represented the best diagnostic capacity to rule out the presence of pilocytic astrocytoma (Table 3).
Table 3 Proposed apparent diffusion coefficient cut-off points and their diagnostic performance for the differentiation of medulloblastoma and pilocytic astrocytoma.
| Variable | Medulloblastoma | Pilocytic astrocytoma |
|---|---|---|
| Proposed cut-off points for apparent diffusion coefficient | 0.6210 x 10-3mm2/s | 1.03 x 10-3mm2/s |
| Sensitivity | 81.82% | 66.67% |
| Specificity | 76.47% | 89.47% |
| Positive predictive value | 69.23% | 75.00% |
| Negative predictive value | 86.67% | 85.00% |
Source: Own elaboration.
Discussion
According to Barkovich & Raybaud1, posterior fossa tumors in the pediatric population are common and include neoplasms of different grades (from low to high grade), a biological feature that dramatically influences the treatment approach to and prognosis of these patients. Therefore, proper identification of this type of tumor through diagnostic imaging is essential for proper management.
Based on the above, the present study discusses the usefulness of quantitative ADC values for the differential diagnosis of posterior fossa tumors in the pediatric population of Colombia since there are no data on this subject in the country to date.
In the present study, the median quantitative ADC in each histological subtype was also taken as a reference and compared with the median quantitative ADC in the other histological subtypes found. As a result of this analysis, the relationship between the value of quantitative ADC in medulloblastoma and in tumors other than medulloblastoma, and between the value of quantitative ADC in pilocytic astrocytoma and in tumors other than pilocytic astrocytoma were identified as variables with statistically significant differences (Table 2). For these variables, the cut-off point was established as the one with the best diagnostic performance in terms of sensitivity, specificity, and positive and negative predictive values. In this sense, it was identified that a quantitative ADC value <0.6210 x10-3mm2/s provides the best diagnostic capability for medulloblastoma, while one of <1.03 x10-3mm2/s provides the best performance to rule out the presence of pilocytic astrocytoma taking into account the greater specificity found in the relationship between the median quantitative ADC and the presence of pilocytic astrocytoma.
These cut-off points are consistent with what was previously described by different authors who have attempted to standardize diagnostic quantitative ADC values in posterior fossa tumors in the pediatric population and have identified an inversely proportional relationship between this value and tumor grade in the posterior fossa, with lower values for more aggressive tumors, as in the case of medulloblastoma.6,12-16
Thus, Rumboldt et al.,6 in a retrospective study carried out in the United States, reviewed brain MRI studies that included ADC maps of 32 pediatric patients with histologically proven cerebellar neoplasm. They found that ADC values were significantly higher in pilocytic astrocytoma (1.65±0.27 x10-3mm2/s) than in ependymoma (1.10±0.11 x10-3mm2/s) and medulloblastoma (0.66±0.15 x10-3mm2/s).
On the other hand, Mohamed et al.,16 in a prospective study conducted in Egypt between May 2018 and August 2019 in 30 pediatric patients (2-17years) with posterior fossa masses, found that ADC values were significantly different between pilocytic astrocytoma (1.43±0.28 x10-3mm2/s) and medulloblastoma (0.71±0.21 x10-3mm2/s), with a p<0.001.
Given the findings, it is considered that the proposed cut-off points can be used in the Colombian pediatric population; however, studies with larger sample sizes and in different population groups are required to validate the values proposed specifically for the diagnosis of medulloblastoma and pilocytic astrocytoma.
The limitations of the present study include its retrospective nature, as well as the lack of a molecular characterization of the different tumor subtypes, which is associated with the fact that the molecular studies needed to achieve such characterization are not yet routinely performed in Colombia. On the contrary, the sample size, the fact that low- and high-grade tumors were available, and that the same MRI protocol was followed in all patients were considered as strengths, thus allowing for the adequate interpretation of the results and a comparative analysis of the quantitative ADC.
Conclusions
The quantitative ADC value is useful to classify and differentiate posterior fossa tumors in the Colombian pediatric population, showing an inversely proportional relationship with the histological grade of the tumor. In this sense, it is recommended to use a quantitative ADC value of ≤0.62x10-3mm2/s as a cut-off point for the diagnosis of medulloblastoma and a value of ≤1.03x10-3mm2/s to rule out the presence of pilocytic astrocytoma in this population.
















