Introduction
Alveolar soft part sarcoma (ASPS) is a malignant soft tissue tumor of uncertain histogenesis, with a poor prognosis and a very low frequency of occurrence among the different types of soft tissue sarcomas (STSs).1-3 It is a well-differentiated clinical and morphological entity characterized by a typical histological image, specific molecular alterations, and a unique and distinctive clinical behavior. 1-4 ASPS usually starts in the extremities, commonly in the thighs and buttocks, in adolescents and young adults. 2 Despite having a relatively indolent growth rate, up to 79% of patients suffering from ASPS develop a metastatic disease. Unlike other STSs, ASPS metastasizes not only in the usual places, but also in the brain. 4
The histopathological differences among STSs subtypes may have an impact on optimal treatment. For instance, surgical resection with or without radiotherapy is the standard treatment for localized diseases, while chemotherapy is the mainstay for the management of advanced and metastatic situations. 5-10 Although STSs are traditionally classified by the morphology and the type of tissue they resemble, 11 understanding of tumor biology and sensitivity is continuously evolving, enabling better therapies. Surgery can improve ASPS prognosis even in cases of metastatic disease; on the other hand, traditional chemotherapeutic agents and radiation therapy have yet to be proved being capable of increasing the survival of patients with ASPS. 11 The 5-year overall survival documented in the literature for patients younger than 25 years old is 83%.12
The following is the case of a patient with a rare condition (ASPS), who had multiple episodes of relapse and metastases prior to receiving adjuvant treatment with three-dimensional conformal radiation therapy (3DCRT), and who remains disease-free. The 3DCRT technique includes imaging, accurate radiation dose calculation, computer-optimized treatment planning, and computer-controlled treatment delivery.
Treatment plans are individually designed and based on patient-specific 3D images. When using 3DCRT, higher doses of radiation can be delivered to cancer cells while significantly reducing the amount of radiation received by the surrounding healthy tissue. To date, the best therapeutic approach to ASPS is not clear. Given the particular evolution of the patient and considering the concepts emerging in current radiotherapy, it is appropriate to share this information and reflect on the management of these ASPS cases and the effectiveness of their potential treatments.
Case presentation
Patient information
In November 2007, an apparently healthy 21-year-old woman, who did not smoke and was not taking any medication, was admitted to the Instituto de Oncología Ángel H. Roffo, Buenos Aires, Argentina. The reason for consultation was an increase in volume of the right thigh, without pain or discomfort.
Clinical findings
The initial physical examination confirmed the presence of a lump. Regarding her disease history, the patient did not report any relevant medical or family history. During the first medical appointment, biopsy and magnetic resonance imaging were prescribed.
Timeline, diagnostic assessment, and therapeutic intervention
In December 2007, a gross total resection of the primary tumor was performed. Macro-scopically, it was brownish, firm and uniform, and measured 10x8x7cm. Histologically, the tumor was composed of cells with a large nucleus, prominent nucleoli and clear cytoplasm, arranged in a predominantly solid and alveolar pattern. The resection edges were free of tumor tissue. Immunohistochemical staining revealed that the lesions were positive for vimentin, desmin, cytokeratin and cytoplasmic MYOD1, and negative for muscle-specific actin, S100, and MYF4 myogenin. These findings confirmed the diagnosis of ASPS.
Two years after the first surgery, two metastatic tumors were detected in the right lung, which were completely resected separately. A sarcoma metastasis with alveolar pattern was described in the histopathological report of both tumors. The resection limits were free of tumor tissue.
Two years after the second surgery, the patient had two independent relapse events, five months apart. In both cases, gross total resection of the tumor was prescribed. In the first episode, an irregular brownish-white mass of 7x5x4cm was observed at the level of the striated muscle of the right tight. The second event was presented to the Tumors Committee of the Instituto de Oncología Ángel H. Roffo since metastasis in the left adrenal gland together with local thigh relapse were observed. Brain magnetic resonance imaging (MRI), abdominal ultrasound and consultation with the infectious disease and endocrinology teams were indicated.
The brain MRI was normal but a solid nodular image of 3.5cm in diameter was recognized on the right pectineus muscle. The abdominal ultrasound showed a heterogeneous mass of 4.6cm in the left adrenal gland. Plasma and urinary cortisol, as well as adrenaline and noradrenaline levels, were within normal physiological ranges. Resection of the right thigh mass and laparoscopic adrenalectomy were performed. The margins of both resections were free of tumor tissue and a metastatic tumor diagnosis was histopathologically confirmed.
The following year, an MRI detected a focal area of enhancement of the right thigh. The patient was closely monitored and, two years later, an increase in size was noted, so surgery was recommended. A computed tomography (CT) of the lower limbs revealed two focal lesions and no involvement of the adjacent cortical bone was detected. The proximal and smaller lesion was associated with the area where surgical traces and scarring changes were evident, while the most distal lesion was associated with the thickening of the skin located in front of it.
Both nodules were removed; from each resection, whitish lobed tumors measuring 2x1.5x1.5cm and 5x3.5x3cm were dissected. Both lesions were located in the subcutaneous cellular tissue and had non-infiltrative margins. The largest lesion extended to the muscular layer, compressing but not invading it. The limits of both resections were free of tumor tissue. The two thigh nodules that appeared during the last relapse caused a risk of amputation due to intimal injury with a nerve-vascular bundle. Therefore, the case was discussed by the Oncological-Surgical Forum of the Instituto de Oncología Ángel H. Roffo, which indicated the administration of 3DCRT as adjuvant treatment with curative purposes of the thigh on the surgical bed.
In June 2014, the 28-year-old patient was admitted to the Radiotherapy Center in good general condition, but with a decrease of the muscular component in the right thigh as a consequence of previous surgery. The patient presented complete surgical scarring and a hypertrophic scar due to thermal burns associated with a history of anesthesia, without clinical signs of distant metastatasis. A virtual simulation, planned on tomography, was done, taking the preoperative MRI and CT images as reference. Then, the limb was immobilized with a cushion and marked with skin tattoos longitudinally and laterally. Positioning was controlled with portal film imaging for the first 3 days.
The radiotherapy protocol consisted in irradiation from four fields. Figure 1A shows a 3D reconstruction of the right tight, where the irradiated areas can be seen. The clinical target volume (CTV) was irradiated with a total dose of 46Gy (ISO1), given at daily fractions of 2Gy from two fields each day (Figure 1B); the other two fields correspond to two boosts. The irradiated regions are shown in Figure 1C, upper (ISO2) and lower (ISO3) (2Gy per day; total dose: 20Gy and 10Gy, respectively). The treatment plan could not avoid irradiating the scar caused by thermal burns. Consequently, ISO3 had to be suspended after one week of treatment because the patient presented grade two dermatitis in this area according to the Radiation Therapy Oncology Group toxicity criteria.
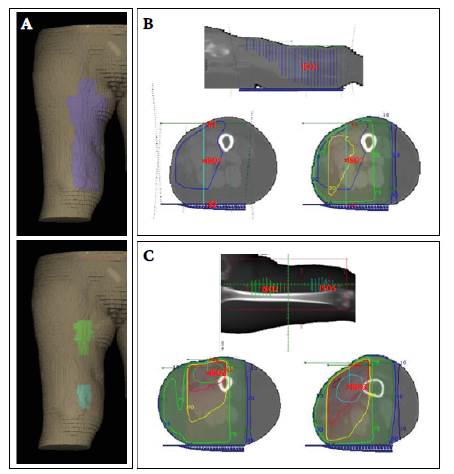
Source: Own elaboration.
Figure 1 A) 3D reconstruction of the patient's right thigh: clinical target volume (upper panel) and both boosts (lower panel). B) Clinical target volume. Upper panel: sagittal section of the thigh, showing the irradiated region and the accessory used during the radiotherapy (wedge). Lower panel: axial section of the thigh. Left: irradiated region (blue), isocenter (red cross), and irradiation fields (#1 and #2). Right: irradiated region and isodose curves. C) Boosts. Upper panel: coronal section of the thigh, showing the irradiated regions ISO2 and ISO3. Lower panel: axial section of the thigh. Left: irradiated region in ISO2, isocenter (red cross), and isodose curves. Right: ISO3 and isodose curves (dark red: 105; red: 97; yellow: 90; green: 75; blue: 30; dark blue: 10).
The estimated radiation dose for each ISO in the right thigh is depicted in Figure 2.
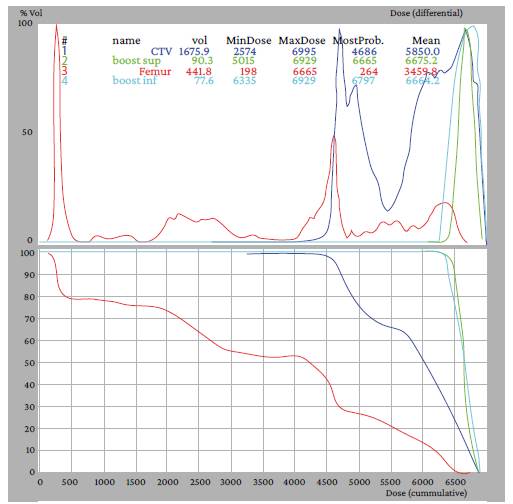
Source: Own elaboration
Figure 2 Histogram of radiation dose (X axis) versus tissue volume (Y axis). Upper panel: plot of the differential dose. Lower panel: plot of the accumulated dose (blue curves: CTV; green curves: upper boost; turquoise curves: lower boost; red curves: femur).
On the other hand, about 28% of the total volume of the femur (the risk organ), that is, the bone part close to the CTV, received the maximum dose of the treatment, while the rest was preserved with less than 60% of the total dose. These data suggest that the treatment plan was successful in avoiding damage to this organ. At the end of treatment, patient evolution was favorable in general terms, except for scar dermatitis. It should be noted that the patient did not undergo any systemic treatment.
Follow-up and outcomes
By September 2020, at the age of 34 years, the patient was being monitored with periodic evaluations by magnetic resonance of the thigh and knee, as well as tomography of the lung area. The patient was not receiving any treatment and showed disease regression and stabilization without extension to other organs, achieving five-year disease-free survival.
Discussion
Alveolar soft tissue sarcoma is a rare disease that mainly affects females and youth. In young adults, it commonly occurs in the lower extremities and usually presents as a large long-standing tumor mass, as it was the case with this patient.2,3,13,14 Although histological analysis is decisive for tumor characterization in the diagnosis of ASPS, CT and MRI allow to define the precise extent of the tumor; the areas of necrosis; the presence of hemorrhage; the presence of calcification and extension to the bone; intra- or extra-compartmental distribution; possible metastasis; and the relationship of vessels and neighboring nerves with the tumor. 1,11,15
In the present case, morphologically, the primary tumor was a large size mass, larger than the average reported (9cm), suggesting an unfavorable course. 13,14 The histopathological analysis reported tumor cells with conspicuous nuclei and clear cytoplasm, arranged in an alveolar pattern. The characteristic immunohistochemical markers of these sarcomas were also confirmed. It is important to emphasize that a larger size and a later stage indicate a higher risk of metastasis and local recurrence. These tumors are very aggressive and, despite their slow development or as a consequence of it, they can cause early distant metastasis (most often in the lungs and brain) since they go unrecognized, produce no discomfort, and rarely present with functional deterioration of the limb on which they are located.
These lesions can occur long after the initial resection, even if there is no local recurrence. 2,3,13,14 In the case presented here, following the normal course of the disease, two events of metastasis were observed with multiple local relapses, one in the lungs and the other in the suprarenal gland. All tumors were successfully excised.
The particular characteristics of this case are associated with the outcomes of radiotherapy. Most reports suggest that resection of the primary tumor at an early stage is the mainstay of treatment, the standard approach regardless of the type of sarcoma, and that adjuvant RT is not indicated when negative margins are achieved; moreover, this patient was referred to consultation with the Oncological-Surgical Forum of the Instituto de Oncología Ángel H. Roffo due to multiple relapses.
Conventional chemotherapeutic agents and radiotherapy have, in general, failed to increase patient survival 4,11,14 However, although its role is critically discussed, radiotherapy appears to reduce local recurrence without altering patient survival. Furthermore, for advanced cases with multiple metastases and recurrence, palliative treatment is preferred considering the poor prognosis. 14 Even though the case presented here shares the overall characteristics discussed above, a striking improvement in the efficacy of radiotherapy can be inferred, namely improved disease control, as no metastases or recurrences were observed up until the time of writing this paper and five-year disease-free survival was achieved.
Radiotherapy has always been regarded as a fundamental part of oncological treatment. A standard radiotherapy treatment consists of a total dose of 50-66Gy administered at 1.8 or 2Gy per day, depending on whether the location allows it based on the tolerance of organs at risk. Being a locoregional therapy, it complements surgery and chemotherapy as local and systemic treatments, respectively. This type of treatment is implemented in at least 50% of patients, with curative purposes for localized cancers or isolated metastases, and as a palliative treatment in patients with disseminated disease. 16,17
However, in recent years, salient evidence indicates that radiation not only produces cytotoxic effects on irradiated tumor cells, but also induces an immune-mediated systemic response, with potentially anti-metastatic properties. 18,19 This phenomenon is observed outside the irradiated zone, is known as abscopal effect, and is currently a topic of significant scientific interest. An "abscopal" effect occurs when localized radiation alters the body as a whole; this term encompasses a dichotomy, which mainly includes distant tumor regression from the irradiated area until the induction of genomic instability and cell death in normal tissues. 20
Conclusions
Beyond presenting a particular histology and a well-characterized genetic translocation, many questions about the pathogenesis and treatment of ASPS remain unanswered. In this case, surgical removal of the primary tumor mass and metastases resulted in prolonged survival, while the benefit of adjuvant chemotherapy and/or radiotherapy has been questioned.
Although more results based on stronger scientific evidence are needed, taking into account the particular progress of the patient, especially after 3DCRT, emergent radiobiological paradigms should be considered, as they support the holistic effect of radiotherapy and would eventually explain some of the encouraging and unexpected results reported here.
In the light of the foregoing, a greater understanding of the non-focused effects of radiation would help determining its relevance for optimal treatment and the best clinical approach to ASPS.















