Introduction
Endoscopic removal of foreign bodies (e.g., a toothbrush) from the upper digestive tract is a major therapeutic challenge, whose success depends on extracting them without problems and avoiding surgical removal. Toothbrushes are rarely swallowed; for example, in a series published in 2020, of 172 cases of foreign bodies identified in the esophagus or stomach, only 3 were toothbrushes.1
As with any other foreign body, swallowing a toothbrush may be intentional or accidental, and is more common among older adults, patients with mental disorders or intellectual disability, people with alcohol problems, and prisoners.2
The following is the case of a young woman with bulimia nervosa, who swallowed a toothbrush while self-inducing vomiting, which was removed via endoscopy.
Case presentation
A 22-year-old woman diagnosed with bulimia nervosa two years earlier and under psychiatric treatment accidentally swallowed a toothbrush for adults while inducing vomiting. During this maneuver, which she had performed frequently over the past few years and was accustomed to doing while bending, she experienced a sudden retching that caused her to swallow the toothbrush immediately and involuntarily. Three hours after the incident, the patient visited the emergency service of a tertiary healthcare center in Bogotá D.C., Colombia, where she underwent an abdominal X-ray that did not reveal the toothbrush, but did reveal considerable food debris in the epigastrium
Since the patient was asymptomatic, the ingestion of the toothbrush was dismissed; however, due to her history of eating disorder (bulimia nervosa), she was referred to the psychiatry service and discharged six hours after admission.
The following day, despite continuing to be asymptomatic, the patient insisted on the ingestion of the toothbrush, so her relatives spoke with her treating physician, who referred her to a secondary healthcare center, where she was admitted 36 hours after the ingestion. On admission, besides bulimia nervosa, she reported being treated for hypothyroidism with levothyroxine 75 mcg/day.
On admission examination, the patient was found in good general condition and with the following vital signs: blood pressure: 111/70 mmHg, heart rate: 74 bpm, respiration rate:18 rpm, oxygen saturation: 92%, fraction of inspired oxygen: 24% and temperature: 36°C. No abnormal findings were reported on physical examination, and no respiratory distress, sore throat, or abdominal pain were observed. The patient weighed 64kg, was 1.55m tall, and her body mass index was 26.64 kg/m2.
Taking into account the unusual type of foreign body ingested (toothbrush), a team consisting of two specialists in gastrointestinal surgery and digestive endoscopy, a dentist, and three nurse assistants, all with extensive experience in foreign body extraction, was prepared. In turn, the following endoscopic instruments were available: three over-tubes of different calibers and length (Guardus-overtube Ref 00711149 from US endoscopy for gastroscopy, and ST-SB1 from Olympus and EN-580T Fujifilm for enteroscopy), large mouse-tooth forceps for foreign bodies, large polypectomy loop, electrosurgical unit with argon plasma coagulation, cervical pillow, laryngoscope, orotracheal tubes, and manual resuscitator (Ambu).
The anesthesiologist agreed to perform conscious or deep sedation (with propofol and remifentanil) depending on the course of the extraction procedure; the possibility of orotracheal intubation (OTI) was also considered.
Endoscopy confirmed the presence of the toothbrush in the stomach and established that the head had impacted the gastric folds (due to the greater curvature at the junction between the body and the antrum) (Figure 1A) and the tip of the handle crossed the pylorus to the duodenal bulb (Figure 1B); the toothbrush did not move.
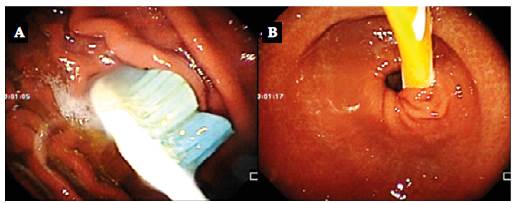
Source: Imaging scans obtained during the study.
Figure 1 A) Head of the toothbrush impacted in the gastric folds of the greater curvature at the junction of the body with the antrum; B) tip of the toothbrush handle passing the pylorus and moving towards the duodenal bulb.
Overtube (Guardus-overtube Ref 00711149 of US endoscopy, 19.5mm diameter and 50cm long) was mounted and passed in the left lateral decubitus position due to several failed attempts in the supine decubitus position, even with the patient under deep sedation. Due to the impossibility of releasing the ends of the toothbrush, which was arc-shaped (Figure 2A), it was decided to cut it by means of argon plasma coagulation. Although it was not possible to cut it completely, when heated, the toothbrush softened momentarily (Figure 2B), which allowed to move it into the stomach and, in this way, to position it longitudinally and in line with the esophagus (Figures 2C and 2D).
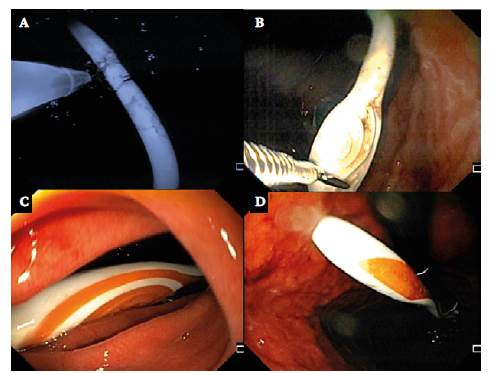
Source: Imaging scans obtained during the study.
Figure 2 A) Partial cutting of the toothbrush handle by means of argon plasma coagulation; B) proximal traction of the toothbrush head with foreign body forceps; C) longitudinal position of the toothbrush on the same axis as the esophagus (front view); D) longitudinal position of the toothbrush with the handle released and removed from the duodenal bulb (endoscopic retrovision).
The toothbrush slipped quickly when attempting to grasp its head with the forceps, so it was decided to pull it with a polypectomy loop, allowing the head to be brought closer to the gastroesophageal junction (Figure 3A). In turn, the tip of the overtube was moved by impulse and located about 38cm from the gastroesophageal junction. Given the size of the toothbrush head, it could not be fully inserted into the overtube (Figure 3B and 3C), but the latter was used as a guide for opening the esophagus and cricopharyngeal muscle during traction. The foreign body was extracted by simultaneous traction; to this end, one of the endoscopists was in charge of the overtube and the other of the toothbrush (Figure 3D). When the head of the toothbrush was in the cricopharyngeal muscle, cervical hyperextension was performed, which allowed retrieving it from the patient's mouth, prior removal of the mouthguard (Figures 4A and 4B).
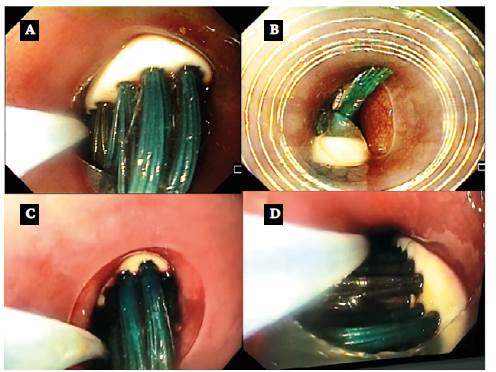
Source: Imaging scans obtained during the study.
Figure 3 A) grasping of the toothbrush head with a polypectomy loop and insertion into the overtube; B) loss of the toothbrush when taken with a foreign body forceps due to slipping on one side of the overtube; C) retaking of the toothbrush more proximal to the tip with a polypectomy loop; D) simultaneous traction of the endoscope, the loop capturing the head and the overtube.

Source: Imaging scans obtained during the study.
Figure 4 A) Final removal of the toothbrush in cervical hyperextension (caught with the loop and retrieved in the mouth with the fingers of one of the operators, after removing the mouthguard); B) standard adult toothbrush retrieved.
During a follow-up endoscopy performed immediately after the toothbrush was retrieved, two small 4-mm hematomas were observed in the posterior wall of the mid-esophagus (Figure 5A), but no lesions were found at sites that could be injured (cricopharyngeal muscle, gastroesophageal junction, gastric folds of the greater curvature, or duodenal bulb) (Figures 5B and 5C).
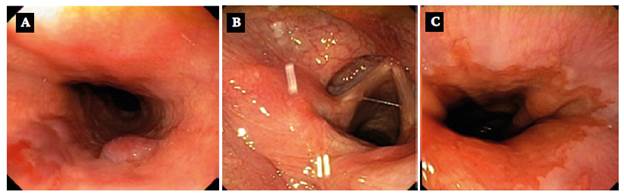
Source: Imaging scans obtained during the study.
Figure 5 Endoscopy performed immediately after extraction. A) non-expansive hematomas in the posterior wall of the mid-esophagus; B) hypopharynx and larynx; C) gastroesophageal junction and sites that could suffer damage intact.
The patient was discharged 90 minutes after completion of the procedure. No early or late complications or adverse events were detected in the 8-day follow-up. The young woman continued to be followed up by the psychiatry service.
Discussion
Toothbrushes, given their physical characteristics, are classified as long and hard foreign objects when swallowed;2,3 hence, they may have difficulties passing through the duodenum and should be retrieved.3
In Colombia, there are no epidemiological data on the prevalence of toothbrush swallowing, but it can be concluded that it is a very unusual event because this is the first case of its kind treated by the professionals who performed the extraction, who have more than 25 years of professional experience. In this regard, Skok & Skok,1 in a retrospective study conducted between January 1, 1994, and January 1, 2018, in 13 196 patients, reported that there were only three cases of toothbrush swallowing among the individuals in whom true foreign bodies were detected (n=172; 1.3%).
Usually, people who swallow toothbrushes suffer from mental disorders4,5 or developmental delay;5 try to induce vomiting;6 have alcohol abuse disorders;7,8 or are deprived of their freedom (prisoners).2,5 Often, they do so unintentionally (as in this case) or intentionally out of curiosity or to obtain benefits, as in the case of inmates, who may be transferred to places with more favorable detention conditions following these events.
Given the length of the toothbrushes (usually >6cm), it is quite improbable that they pass beyond the duodenum in the digestive tract if swallowed; therefore, it is necessary to remove them, which involves careful planning and consideration of five specific factors:
Expertise of the work team: endoscopists and assistants who are experts in foreign body removal, overtube placement, and handling of endoscopic accessories should be selected; they should also have the ability to recognize when removal must be interrupted if it cannot be done endoscopically.9
Availability of endoscopes and removal devices: availability of equipment such as endo -scopes; mouse-tooth or alligator forceps for foreign bodies; Dormia baskets; plastic endoscope tip protector; polypectomy snares; mechanical lithotripter; and argon plasma electrosurgical unit.10,11
Overtubes: overtubes should be used as they serve as protectors against injuries caused by the ends of the toothbrush or its bristles if it can be inserted into them.12 However, these elements should be inserted carefully because there is a risk of injury to the cricopharyngeal muscle or esophagus, which was avoided in this case by pushing the overtube with the patient in the left lateral decubitus position and selecting the softest, thinnest overtube (19.5mm), with sufficient length (50cm) to allow it to go beyond the gastroesophageal junction.
Sedation and anesthesia: an anesthesiologist who is an expert in diagnostic and therapeutic digestive endoscopy should be available to determine the sedation plan to be used based on the patient's conditions.9 In most cases, foreign body removal procedures are performed under conscious sedation,3,13 but the possibility of deep sedation and even general anesthesia with OTI should always be considered. In the present case, the patient required deep sedation several times, which lengthened the total time of the procedure given the need to provide temporary ventilatory support.
Prevention of complications: international guidelines for performing foreign body removal procedures should be followed, as this helps prevent frequent complications such as bleeding; injury to the gastroesophageal junction, cricopharyngeal muscle, or laryngopharynx; esophageal, gastric, or duodenal perforation; mediastinitis; peritonitis; and fistulas.5,14 Endoscopy immediately after removal is essential to detect complications, since most lesions can be managed endoscopically by means of hemostatic clips, coated self-expanding prosthesis, epinephrine1, or electric or argon plasma coagulation, but this procedure eventually allows defining an immediate surgical conduct.14 In the endoscopy performed on the patient reported here after surgical removal, two small, non-expansive hematomas in the esophagus were observed that did not require any intervention.
Failure of endoscopic foreign body removal may result in surgical extraction under local anesthesia and laparoscopic gastrotomy.15
The publication of this case report teaches us several lessons, including the fact that neither non-enhanced abdominal X-ray nor abdominal ultrasound can be used to rule out the presence of foreign bodies because, for example, toothbrushes are radiolucent and thus best detected with three-dimensional reconstruction computed tomography.16 It is worth noting that the reported patient did not undergo an abdominal ultrasound because epigastric visibility would be inadequate considering that she had eaten immediately before swallowing the brush.
This case also showed the importance of believing the patient regardless of her psychiatric history and not stigmatizing her in order to provide adequate treatment and avoid delaying therapeutic decisions.
Similarly, taking into account the evolution of this case, it is suggested to follow the steps that have been recently established in clinical practice for the successful removal of foreign bodies: to identify; to mobilize; to catch; to align in parallel the longitudinal axes of foreign body and organ; to protect sites that may be injured; to mobilize the object until it is retrieved; to perform exploratory endoscopy immediately after removal to identify and solve immediate complications; and to perform early and late follow-up.
Finally, if the intervention is performed in a tertiary healthcare center, the use of OTI should be considered from the beginning since it allows the procedure not to be interrupted for ventilatory support if deep sedation is required, as in the present case. However, it should be kept in mind that OTI may make the placement of the overtube and the final removal of long foreign bodies, such as toothbrushes, uncomfortable or difficult.
Conclusions
Although cases of involuntary swallowed toothbrushes are rarely reported, they occur mainly in people with mental disorders, such as eating disorders when trying to induce vomiting. Therefore, even in the absence of symptoms and imaging findings, the patient's version should always be believed, as this allows for a timely referral to the digestive service to confirm the ingestion and perform endoscopic removal as soon as possible, because, due to their characteristics, they can cause serious complications.
Endoscopic removal of foreign bodies is a major therapeutic challenge requiring meticulous planning, specialized equipment, and exceptional technical and judgment skills to avoid complications.















