Introduction
Smoking is one of the leading preventable risk factors for diseases such as cancer and cardiovascular and lung diseases. It also worsens the clinical outcomes of other conditions such as tuberculosis, mental illness, human immunodeficiency virus (HIV) infection, and alcoholism.1
The global prevalence of tobacco use is approximately 25%, with a significant mortality burden because it causes over 8.2 million deaths annually, of which 7 million are directly associated with tobacco consumption and 1.2 million are attributed to exposure to secondhand smoke.2,3 In Colombia, as reported by Peña et al.,4 smoking is the cause the death of about 32 088 people every year and, according to the National Survey of Psychoactive Substance Use,5 the lifetime prevalence of tobacco use in 2019 was 33.3% (43.0% in men and 24.3% in women).
The World Health Organization (WHO) Framework Convention on Tobacco Control, which was proposed as a strategy to control the tobacco epidemic,6 has made progress through the implementation of the six MPOWER measures in 2008 (1. monitoring tobacco use and prevention policies, 2. protecting people from tobacco smoke, 3. offering help to quit tobacco use, 4. warning about the dangers of tobacco, 5. enforcing bans on tobacco advertising, promotion and sponsorship, and 6. Raising taxes on tobacco); however, although tobacco consumption has declined in most countries and regions, the fact that the population has grown means that the total number of people who use tobacco has remained high, which shows that the tobacco epidemic is far from being overcome.3
Counseling and pharmacological therapy have been shown to be effective in smoking cessation7,8 and, as reported by Alba et al.,9 the combination of these interventions increases cessation rates from 5.1% to 22.7%, which has also been documented in other studies.10 Thus, it is recommended to implement short-term counseling strategies during the initial approach of patients who are smokers since it has been demonstrated, mainly in the outpatient setting, that they increase abstinence rates in about 5% of cases.9,11,12 However, there is emerging evidence of the effectiveness of these interventions in the hospital setting,13 which confirms the importance of addressing this risk factor whenever there is contact with the smoker, whether in inpatient or outpatient services.
In Spain, between 15% and 27% of patients admitted to hospitals are smokers, so hospitalization is considered an ideal moment for smokers to consider quitting tobacco consumption.14 It is therefore necessary to characterize this type of population, adapt the provision of services to their health conditions, and take action to intervene in their risk factors.15
Currently, in Colombia, there are few data on the prevalence and characteristics of smokers treated in hospital settings, so the objectives of this article were to describe the sociodemographic, family and clinical characteristics of smokers treated in a quaternary care hospital and to establish the variables associated with the smoking cessation intention in order to optimize the management of this risk factor in the hospital setting.
Materials and methods
Study type and population
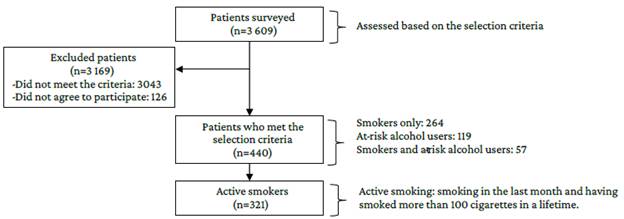
Cross-sectional descriptive study conducted between April 2018 and November 2019 in a quaternary care hospital in Bogotá, Colombia, and nested in a randomized clinical trial. The trial assessed 3 609 patients based on the following selection criteria: age between 19 and 64 years, active smoking (having consumed any tobacco product in the previous and having smoked more than 100 cigarettes in a lifetime), at-risk alcohol consumers (having consumed 4 or more standard alcoholic beverages per day in women and 5 or more in men in the previous 12 months at least once), and an AUDIT (Alcohol Use Disorders Identification Test) score between 8 and 15.16 They were also required to have a permanent address and contact information, in addition to being scheduled for surgery or any diagnostic procedure that necessitates preparation in advance.
Participants who were on smoking cessation treatment, were dependent on any other psychoactive substance, had diseases that compromised their ability to understand information or communicate verbally, and were in the action and maintenance stages of their smoking cessation process17 were excluded.
The full protocol of the randomized clinical trial18 upon which the present study was based is available at ClinicalTrials.gov under the identifier NCT03521622.
Following the implementation of the selection criteria, 3 169 patients were excluded and 440 were selected (264 smokers, 119 with risky alcohol consumption, and 57 with both risk factors), of whom 321 were classified as active smokers in the present study (Figure 1).
Procedures and instruments
After the participants signed the informed consent form, the research team members administered a 46-item questionnaire to collect sociodemographic (age, sex, marital status, socioeconomic status, and educational level), family (family type, stage of family life cycle, and family functionality), clinical (concomitant conditions, type of care received, need for hospitalization, and days of hospital stay), and smoking-related information (history of smoking, pack-year, degree of physical dependence on nicotine according to the Fagerström Test,19 cessation attempts, and intention to stop smoking according to the stages of change of Prochaska and DiClemente).20
Data were collected in the REDCap electronic data capture system version 7.3.6. of 201921 while the participants were hospitalized. The prevalence of current smoking, with its corresponding 95% confidence intervals (95%CI), was calculated taking into account the total number of people assessed for enrollment in the study (N=3 609).
Statistical analysis
For data analysis, simple frequencies and proportions were used for categorical variables, and measures of central tendency (means or medians) with their respective dispersion measures for the numerical variables. Associations were established between the dependent variable (smoking cessation intention measured based on the placement of smokers in the stages of change proposed by Prochaska and DiClemente: precontemplation, contemplation, and preparation), intermediate variables (patient perception of the benefits of quitting smoking, perceived self-efficacy -ability to quit smoking-, degree of motivation-willingness to quit smoking-, and attempts to quit -prior attempts-), and the independent variables (sociodemographic, family, and clinical) by means of a bivariate analysis using the Chi-square statistical test and considering a significance level of p<0.05.18 It should be noted that intermediate variables were measured on a scale of 0 to 10 using verbal self-reporting.
Finally, a multivariate analysis was performed by means of an ordinal logistic regression model with its corresponding 95%CIs. Data were processed in R software version 4.0.3.
Ethical considerations
The present study took into account the ethical principles for medical research involving human subjects established by the Declaration of Helsinki,22 the international guidelines for biomedical research involving human subjects established by the Council for International Organizations of Medical Sciences and WHO,23 and the provisions on health research contained in Resolution 8430 of 1993 issued by the Colombian Ministry of Health.24 Likewise, it was approved by the Joint Ethics and Research Committee of the Pontificia Universidad Javeriana and the Hospital Universitario San Ignacio in accordance with Minutes No. FM-CIE-0025-18 of January 25, 2018. All participants signed the informed consent form.
Results
Of the 3 609 patients assessed in the randomized clinical trial and who met the selection criteria, 321 were classified as active smokers, i.e., the prevalence of tobacco use in the last month was 8.89% (95%CI: 7.97-9.82).
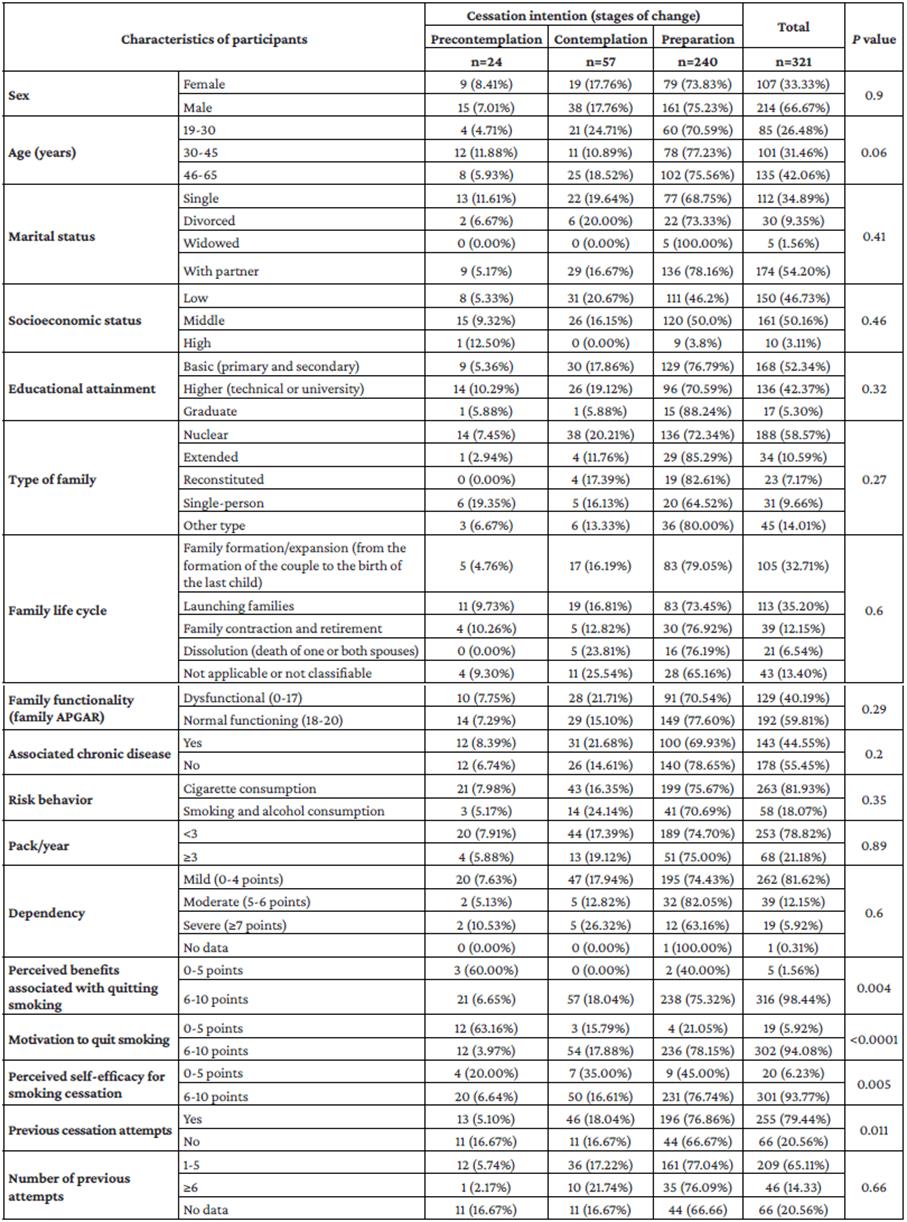
Of these 321 participants classified as active smokers, 66.67% were men, 96.89% had a low or middle socioeconomic status, 52.34% had a basic educational attainment, and 42.06% were between the ages of 46 and 65. Similarly, 44.55% had some associated chronic disease, the most frequent being obesity (13.62%) and arterial hypertension (10.61%), and 18.07% (n=57) had concomitant risk of alcohol use (Table 1).
Regarding family characteristics, it was found that 54.21% had a partner, 58.57% had a nuclear family, 40.19% were part of a dysfunctional family according to the family APGAR questionnaire (score <18), and the most frequent stages of the family life cycle were family contraction (35.20%) and family formation/expansion (32.71%) (Table 1).
Table 1 Sociodemographic and family characteristics of active smokers (n=321).
Source: Own elaboration.
With regard to tobacco use, most participants were mild smokers (pack/year <3) and had a low level of physical dependence on nicotine (score <4 on the Fagerström test) (78.82% and 81.62%, respectively).
Concerning smoking cessation intention (stage of change), 74.76% of participants were in the preparation stage (thinking about quitting within the next 30 days), 17.76% in the contemplation stage (considering quitting within the next 6 months), and 7.48% in the precontemplation stage (not thinking about quitting). In addition, most participants reported moderate to high perceptions (6-10 points) of health benefits associated with smoking cessation (98.44%) and moderate to high levels of motivation to quit smoking and self-efficacy (94.08% and 93.77%, respectively). Previous cessation attempts were reported by 79.44%, with a higher frequency of attempts between 1 and 5 times (64.49%) (Table 2).
Table 2 Clinical characteristics of active smokers (n=321).
Source: Own elaboration.
The assessment of factors associated with stages of change (bivariate analysis) revealed a statistically significant association between perceived health benefits from smoking cessation and intention to quit (p=0.004). It was also found that the greater motivation to quit smoking and the more self-efficacy, the higher the probability of being in the preparation stage (p<0.0001 and p=0.005, respectively). Previous cessation attempts were also associated with a higher probability of stopping tobacco use (p=0.011) (Table 3).
Table 3 Sociodemographic, family, and clinical characteristics associated with cessation intention in active smokers (n=321).
The multivariate ordinal logistic regression model confirmed that perceived benefits of quitting smoking and high perceived self-efficacy are associated with a greater likelihood of being prepared to attempt smoking cessation (OR=9.44; 95%CI: 1.27-85.03 and OR=3.73; 95%CI: 1.55-8.78).
Smokers with previous attempts are more likely to have future cessation attempts; however, in the present study, this association was not statistically significant (OR=1.81; 95%CI: 0.98-3.26) (Table 4).
Table 4 Factors associated with smoking cessation intention in active smokers (n=321).
| Variables | OR (95%CI) |
|---|---|
| Perceived health benefits of smoking cessation | 9.44 (1.27-85.03) |
| Perceived self-efficacy for smoking cessation | 3.73 (1.55-8.78) |
| Previous cessation attempts | 1.81 (0.98-3.26) |
Source: Own elaboration.
Discussion
The prevalence of tobacco use in the present study (8.89%) is lower than that reported in the 2007 National Health Survey25 (12.8%) and in other studies conducted in hospitalized patients (11-54%).26-30 This could be related to the fact that a significant proportion of participants were in the 46-65 age range (42.06%) and had a concomitant chronic disease (44.55%) that may have led to smoking cessation. Nevertheless, it is important to highlight that the literature reports a higher prevalence of smoking in patients with chronic conditions such as asthma, chronic obstructive pulmonary disease, HIV infection, and mental illness.26-30
Smoking prevalence figures reported in hospitalized patients are not homogeneous across the various published studies. Auteri et al.,31 for example, found a prevalence of tobacco use of 30.3% in a study that surveyed 376 patients treated in 9 hospitals of Buenos Aires (Argentina) for respiratory diseases, while De La Torre-Hasbum et al.,32 in a study conducted on the medical records of 592 patients to determine the prevalence of hypertension in residents of Santa Marta, Colombia, reported that 11.7% of the patients were tobacco users.
Regarding sex distribution, the proportion of men in the present study was higher than that of women (66.67% vs. 33.33%), similar to what is reported worldwide by WHO (33.7% vs. 6.2%)2 and in Colombia by the National Administrative Department of Statistics (43% vs. 24.3%).5
On the other hand, in the present study, the prevalence of active smokers who also consumed alcohol at risk levels was 18.07%, lower than the 32.8% found by Becerra et al.33 in a study that reviewed the medical records of 134 users of an interdisciplinary smoking cessation program in a university setting in Colombia.
On the other hand, 52.34% had a basic level of education (primary and secondary), a much lower proportion than the 82.09% described by Auteri et al.31 (primary level: 45.19% and secondary level: 36.90%).
In the present study, 58.57% of participants belonged to a nuclear family, a percentage similar to the 55.5% reported in the 2015 National Demographic and Health Survey for the general population in Colombia.34
The presence of family dysfunction in the present study (40.19%) was lower than that reported by Cogollo-Milanés et al.,35 who conducted a study to determine the factors associated with susceptibility to cigarette smoking among 10- and 11-year-old sixth-grade schoolchildren in Cartagena, Colombia, and found that 57.1% of the 289 participants came from dysfunctional families, although this prevalence was higher than the figure reported by Becerra et al.,33 which was 26.1%. These findings are noteworthy since, as indicated by González-Rodríguez & Cardenteey-García,36 family dysfunction, due to its frequency and complexity, poses a challenge for both the diagnostic and therapeutic approach to patients who consume tobacco.
Regarding nicotine dependence, 81.62% of participants had a mild level of dependence (score <4 on the Fagerström Test), which is in agreement with the low level of smoking also found in the present study (78.82% with pack index <3). This figure is much higher than the 49% reported by Carrión-Valero et al.31 in a study conducted in 307 patients of a university hospital in Valencia, Spain, that aimed to determine the characteristics of smokers admitted to different medical and surgical services of the institution. This difference may be explained by the fact that participants included in the present study were candidates for surgery or diagnostic procedures and a significant percentage had a concomitant chronic disease (44.55%).
Concerning the stage of change for smoking cessation, a high percentage of people in the preparation stage was identified (74.76%), which also contrasts with what was reported in the study Carrión-Valero et al.,31 where only 1.7% of the subjects were in said stage of change.
It has been reported that hospitalization is an appropriate moment to carry out preventive interventions to mitigate risk factors such as smoking, since patients are perceived to be more vulnerable and therefore more receptive to change during this time. In this regard, Auteri et al?1 found that 79.7% of the 376 patients treated for respiratory diseases included in their study showed moderate to high motivation to quit smoking.
The variables associated with increased intention to quit smoking in the present study were perceived benefits (p=0.004), degree of self-efficacy (p=0.005), and number of previous smoking cessation attempts (p=0.011), which could be influenced by the fact that participants were hospitalized and this, as mentioned above, can generate a desire to transform bad habits, both to cope with the current condition and to improve the health status.13,31,38
This also coincides with what was reported by Sachs et al.,39 who conducted a study comparing uptake, implementation and effectiveness of two approaches in the delivery of a smoking cessation intervention during pre-admission clinic assessments and identified 1 225 smokers, of whom 714 (58.3%) were enrolled in the smoking cessation program and had a high motivation to quit smoking (7.7 on a scale of 0 to 10).
As previously stated, in the present study, self-efficacy was a variable associated with more willingness to quit smoking. This is consistent with the findings of Balmford et al.40 who, in a study aimed to describe the implementation and effectiveness of a smoking cessation service in Freiburg, Germany, found that patients with greater self-efficacy were more likely to achieve sustained abstinence. In turn, Stegberg et al.41 investigated changes in smoking prevalence, support for smoking cessation, and factors associated with successful smoking cessation in patients with asthma and chronic obstructive pulmonary disease, finding that less nicotine dependence and high self-efficacy are associated with a higher chance of smoking cessation. Finally, Yu et al.,42 in a study conducted to test the hypothesis that perceived health risks of smoking are independently associated with both preoperative intention to abstain and self-reported abstinence at 30 days after surgery, found that factors associated with abstinence included older age, self-efficacy, major surgery, and previous cessation attempts. In this sense, identifying factors associated with increased willingness to quit smoking is essential for planning cessation interventions in hospitals.
Limitations of this study include that smoking status was established based on self-reports without an additional objective confirmation; that participants were in the perioperative period or about to undergo a diagnostic study, a situation that may have biased their consumption responses out of fear of interfering with the provision of the service; and that larger sample sizes may be required to find associations with other variables reported in the literature as influential in the intention of change of behavior. Consequently, more studies should be carried out in Colombia in order to better characterize the smoking population in hospitals and not losing the opportunity of intervening on the main risk factor related to chronic diseases.
Conclusions
The results of the present study demonstrate that there is an association between smoking cessation intention and perceived health benefits and self-efficacy in hospitalized smokers and, therefore, they may be used as a recommendation for implementing smoking cessation treatments in hospital settings, considering that smokers are more motivated to change their risk behaviors in this care setting. Therefore, identifying and characterizing smokers in the hospital setting provides insights to personalize smoking cessation interventions.