Introduction
Placenta previa is a major cause of bleeding during the second half of pregnancy, delivery, and puerperium, and a complication that has a high impact on maternal-perinatal morbidity and mortality.1-3 Its worldwide incidence is estimated to be 0.25-0.50%,4,5 however, in a systematic review and meta-analysis, Cresswell et al.6 stated that this may be up to 5.1% in the Americas and the Caribbean. In view of the above, it should be pointed out that classifications are not internationally standardized.1,4
Given that hemorrhage is the leading cause of maternal mortality worldwide (27%), placenta previa is a public health concern.7-9
According to the National Administrative Department of Statistics (Departamento Administrativo Nacional de Estadísticas - DANE),10 in 2014, there were 493 maternal deaths in Colombia, of which 27 were caused by bleeding during the first half of pregnancy, 8 by bleeding during the second half of pregnancy (1 associated with complications derived from placenta previa), and 46 by postpartum hemorrhage.
In order to prevent complications and reduce the obstetric impact of placenta previa, it is recommended that pregnant women have adequate prenatal care from the beginning of pregnancy and be classified in a timely manner according to their obstetric risk.8,9,11-15 Risk factors for placenta previa reported in the literature include previous Cesarean section; history of uterine surgeries such as myomectomy, uterine curettage, or manual removal of placenta; advanced maternal age; multiparity; multiple pregnancies; uterine myomatosis; smoking; assisted reproductive treatments; and being Black or Asian.2,4,11,16,17
Based on this premise, the objective of this study was to describe risk factors for placenta previa in a sample of pregnant women in Bogotá, Colombia, and their impact on maternal-perinatal morbidity and mortality.
Materials and methods
A retrospective descriptive study was conducted in 17 patients with a diagnosis of placenta previa between 2013 and 2017 treated at the High Obstetric Risk Unit of a tertiary care hospital in Bogotá.
During the study period, 23 pregnant women attended consultation due to vaginal bleeding and/or a diagnosis of placenta previa, but 6 were excluded because placenta previa was ruled out: 4 had a diagnosis of preterm birth threat and 2 a diagnosis of placental abruption. The remaining 17 patients were included in the study.
Data were obtained from the patients' medical records by the medical staff of the high obstetric risk service. The classification of placenta previa used was established according to the location of the placenta with respect to the internal cervical os as follows:1,4
Complete previa: when the placenta completely covers the internal cervical os. Partial previa: when the placenta partially covers the internal cervical os. Marginal placenta: when the placenta is within 2cm or less from the internal cervical os but does not cover it.
Low implantation: when the placenta does not reach the internal cervical os but is 2-3.5cm from it.
Patients were classified based on the traditional classification, which was the one reported in the medical records.1,4,18
A personal history of chronic diseases and OB/GYN conditions such as >4 pregnancies13 and number of previous Cesarean sections and curettage were considered. Clinical and sociodemographic characteristics were also analyzed, including maternal age; gestational age on admission; symptoms on admission; maternal (blood pressure, heart rate, and hemoglobin level) and fetal status (monitoring and ultrasound); findings on transabdominal and/or transvaginal ultrasound; management in place to treat placenta previa; and maternal-perinatal status at the end of pregnancy.
In the descriptive analysis, means and their corresponding standard deviations were calculated for quantitative variables, and absolute and relative frequencies for qualitative variables.
The study took into account the ethical principles for research involving human subjects established by the Declaration of Helsinki19 and the provisions on health research of Resolution 430 of 1993 of the Colombian Ministry of Health.20 It also received the approval of the ad hoc Ethics Committee of the Universidad El Bosque in Session No. 9 of June 27, 2019, and authorization of the Fundación Salud Bosque - Clínica El Bosque for the review of medical records according to the F.S.B.L. Minutes No. 05-473-19 of May 22, 2019.
Results
The 17 patients included in the study were distributed into 2 groups based on their placenta previa classification, as shown in Figure 1.
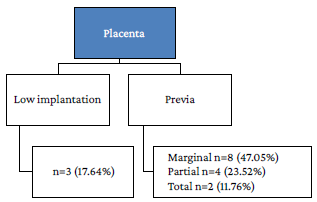
Source: Own elaboration.
Figure 1 Distribution of pregnant women based on their placenta previa classification.
The mean age of the patients was 31.5±6.8 years and the most frequent risk factors associated with placenta previa were ≥4 pregnancies (64.70%), maternal age >35 years (29.41%), previous miscarriages and curettage (29.41% and 23.52%, respectively), and uterine myomatosis (17.64%) (Table 1).
Table 1 Risk factors associated with placenta previa in the pregnant women analyzed (n=17).
| Risk factor | n (%) or x̅ (σ) |
|---|---|
| Mother's age (years) | x̅=31.5 (σ=6.8) |
| Pregnant women >35 years old | 5 (29.41 %) |
| Gestational age at the end of pregnancy (weeks.days) | x̅ =35.6 (σ=4.06) |
| Number of pregnancies ≥4 | 11 (64.70 %) |
| Previous miscarriages | 5 (29.41 %) |
| Previous Cesarean sections | 1 (5.88 %) |
| Previous curettage | 4 (23.52 %) |
| Uterine myomatosis | 3 (17.64 %) |
x̅: mean; σ: standard deviation.
Source: Own elaboration.
With regard to the reason for consultation, 13 patients presented with vaginal bleeding (in one of the cases following abdominal trauma), while the remaining 4 attended for other causes (2 were admitted for elective Cesarean section, one due to pain in the hypogastrium, and the other due to edema in the lower limbs), since they had already been diagnosed with placenta previa. Table 2 summarizes the clinical characteristics of pregnant women with placenta previa with respect to the presence of bleeding, the classification of the placenta, associated conditions, route of delivery, and gestational age at the end of pregnancy. Total placenta previa was found in 11.76% of patients, while 23.52% had partial placenta, 47.05% had marginal placenta, and 17.64% had low-implantation placenta.
Table 2 Clinical characteristics of the participants (n=17).
| Patient | Vaginal bleeding | Placenta previa | Gestational age at the end of pregnancy (weeks) | Associated conditions | Type of delivery | Transfusion |
|---|---|---|---|---|---|---|
| 1 | No | Low implantation | 38.3 | Preeclampsia | Cesarean section | - |
| 2 | No | Marginal | 38.0 | - | Cesarean section | - |
| 3 | Yes | Partial | - | - | Unknown | - |
| 4 | No | Total | 39.1 | Uterine atony | Cesarean section | Yes |
| 5 | Yes | Marginal | - | - | Unknown | - |
| 6 | Yes | Marginal | 22.1 | Preeclampsia | Vaginal | - |
| 7 | Yes | Marginal | - | - | Unknown | - |
| 8 | Yes | Partial | 29.6 | Preeclampsia | Cesarean section | Yes |
| 9 | No | Total | 37.5 | - | Cesarean section | - |
| 10 | Yes | Marginal | 37.4 | Uterine atony Placental accreta | Cesarean section | Yes |
| 11 | Yes | Partial | 38.6 | - | Vaginal | - |
| 12 | Yes | Marginal | 37.0 | - | Cesarean section | - |
| 13 | Yes | Low implantation | 37.6 | - | Vaginal | - |
| 14 | Yes | Marginal | - | - | Unknown | - |
| 15 | Yes | Partial | - | - | Unknown | - |
| 16 | Yes | Marginal | 36.4 | - | Cesarean section | - |
| 17 | Yes | Low implantation | - | - | Unknown | - |
| Total | Yes: 13 No: 4 | - | Placental accreta: 1 Preeclampsia: 3 Uterine atony: 2 | Vaginal: 3 Cesarean section: 8 Unknown: 6 | Yes: 3 |
Source: Own elaboration.
One of the pregnant women diagnosed with marginal placenta previa also presented with placental accreta; she was a 37.4-week pregnant woman in her fourth pregnancy (with one vaginal delivery and two miscarriages that required obstetric curettage) and was admitted due to vaginal bleeding. This patient gave birth by Cesarean section and had uterine atony, requiring subtotal hysterectomy. In this case, the postpartum course was satisfactory for both the mother and the newborn.
Regarding previous uterine surgeries, it was established that 4 of the 5 patients who had had previous miscarriages required obstetric curettage (2 patients underwent 2 curettages, and the other 2 only 1). After curettage, the most prevalent surgical history was Cesarean section (5.88%). No patients with a history of myomectomy were found, but there were 3 patients (17.64%) with a diagnosis of uterine myomatosis.
On the other hand, it was found that 3 patients had preeclampsia; of these, 2 had a history of chronic arterial hypertension and the other had gestational hypertension, and 2 completed their pregnancy by Cesarean section and the other had an extremely preterm vaginal delivery. The latter patient (41 years old; admitted for vaginal bleeding at 19 weeks of pregnancy; with a history of previous delivery, miscarriage requiring curettage, chronic arterial hypertension, and uterine myomatosis not surgically operated, and diagnosis of marginal placenta) had to have her pregnancy terminated because her blood pressure levels progressively increased, and she was diagnosed with severe superimposed preeclampsia at 22.1 weeks.
Concerning the completion of the pregnancy, the route of delivery could not be established in 6 patients since follow-up was performed in another institution, 8 patients underwent Cesarean section (2 scheduled and the others emergency due to vaginal bleeding), 2 patients delivered vaginally at full-term and without complications (one with low-implantation placenta and one with partial placenta), and the other patient had a vaginal delivery with termination of pregnancy due to extreme maternal morbidity at week 22.1 (she had been diagnosed with marginal placenta).
On admission, hemodynamic alterations were only evident in patients who were diagnosed with preeclampsia. Three patients required transfusion of blood products, specifically due to puerperal hemorrhage, and gave birth by Cesarean section.
In relation to hospitalization, 14 patients were admitted between 1 and 4 days, and the remaining 3 were admitted for 13, 21, and 27 days. Eight patients were given home-based conservative management (of these, 2 had full-term vaginal delivery without complications and the outcome of the other six is unknown), while the remaining 9 completed their pregnancy in the hospital. There were no maternal deaths.
As for perinatal morbidity and mortality, the only complication reported was a stillbirth, which corresponded to an extremely preterm delivery. There was also a preterm delivery (36.4 weeks) by Cesarean section. None of the newborns were admitted to the neonatal intensive care unit (NICU).
Discussion
Placenta previa is a serious condition because it can result in a variety of outcomes, which may range from a full-term delivery without complications to unfavorable situations for both the mothers and the fetuses.5 It is a problem whose incidence increases every year, and its diagnosis is clinically suspected based on the presence of vaginal bleeding, but it could also be diagnosed incidentally by ultrasound in asymptomatic patients; the latter may result in a late diagnosis, which may impede timely management.5,16,18 In this sense, it is critical to understand the risk factors for placenta previa and to conduct adequate prenatal monitoring to ensure an early diagnosis, appropriate follow-up, and treatment, as this will allow for better maternal and perinatal outcomes and reduce mortality, which is the fundamental goal of every obstetrician and the health care system.9
There are numerous risk factors for placenta previa described in the literature.2,4,11,16,17 The most frequently found in this study were ≥4 pregnancies, maternal age >35 years, and previous miscarriage, coinciding with the study conducted by Nolasco et al.21 which established that elderly pregnant women have a higher number of complications. Nevertheless, in a study analyzing 283 324 deliveries between 2004 and 2008 in Finland, of which 714 (0.3%) were complicated by placenta previa, Roustaei et al.22 found that the risk of adverse maternal and neonatal outcomes for women with placenta previa was not significantly affected by maternal age if their different risk profiles were taken into account.
On the other hand, in a study carried out in 62 pregnant women who were diagnosed with placenta previa between January 2003 and December 2005 at the Hospital Gine-coobstétrico "América Arias" in Havana, Cuba, Isla-Valdés et al.21 found that Cesarean section, with 32.3%, and previous curettage, with 25.8%, were the surgeries most related to placenta previa. These findings are consistent with those of the present study, although a history of curettage was more frequent here than Cesarean section.
However, the results of the present study are in agreement with the literature reviewed, which suggests that a history of Cesarean section, miscarriage, and curettage predisposes to the development of placenta previa and placental accreta due to the damage that these procedures may cause to the endometrium.24,25
In this regard, Hu et al.,26 in a retrospective cohort study that included 11 662 women who delivered singleton babies at the International Peace Maternity and Child Health Hospital in Shanghai, China, from January 2013 to December 2016, found that, after adjusting for potential confounding factors, women with previous Cesarean section were 2.11 times more likely to have placenta previa (95%CI%: 1.52-2.94). In turn, Gurol-Urganci et al.,27 in another retrospective cohort study of 399 674 women who delivered a singleton first and second baby between April 2000 and February 2009 in England, found that the risk of placenta previa in a pregnancy after the first Cesarean delivery is between 1.5 and 6 times higher than after a vaginal delivery.
This is of great importance since, in developed countries, Cesarean sections account for approximately 15% of births, unlike underdeveloped countries, where these numbers are increasing at an alarming rate.28 For example, in Colombia, according to official DANE figures, the percentage of Cesarean sections has increased considerably, from 37.2% in 2008 to 45.5% in 2017.29
Current evidence also suggests a correlation between the number of Cesarean sections and the occurrence of placenta previa, uterine rupture, and the need for hysterectomy. Thus, Hu et al.26 established in their study that primiparous women who have undergone Cesarean section had a greater number of complications in subsequent pregnancies, including placenta previa. However, Tahseen & Griffiths30 and Das & Varma,31 through systematic reviews, were able to determine that it is possible to successfully complete a pregnancy by vaginal delivery, even if the mother has had one or two Cesarean sections. Therefore, as established by Gibbins et al?2 in their secondary cohort study of 54 458 women who underwent Cesarean section, it is essential to determine the location of the placenta in relation to the internal cervical os and to define the route of delivery to avoid unnecessary surgery and thus avoid complications such as obstetric hemorrhage.
Some studies3,33,34 suggest that when the distance between the placental border and the internal cervical os is >20mm, patients have a high probability of successful vaginal delivery and that the number of complications is low, and further suggest that this situation should be considered as low-implantation placenta and not as placenta previa. These considerations are reflected in the present study, in which three patients diagnosed with placenta previa in the second trimester completed their pregnancy by vaginal delivery without hemorrhagic complications.
This can be explained on the basis of the theory of placental migration (progressive detachment of the placenta from the internal cervical os), a concept that, according to Cunningham et al.,4 was described in 1973 by King. Possible reasons for such migration are related to elongation of the lower uterine segment and the search by trophoblast cells for more vascularized areas in the uterus, moving away from the placental edge of the lower uterine segment that is less perfused.35
The traditional way of classifying placenta previa is marginal, partial, or total depending on the relationship of the placental edge to the internal cervical os;1,4 however, transvaginal ultrasound has now made it possible to determine a more precise location, offering a new classification that allows to guide its treatment and prevent possible complications with regard to the completion of the pregnancy. Thus, if the placental edge is in contact with or up to 1cm from the internal cervical os, completion of pregnancy by Cesarean section is indicated; if it is at a distance between 1cm and 2cm, it is considered as low-implantation placenta and treatment should be individualized; finally, if it is at a distance of 2cm or more, vaginal delivery may be possible.1,36-40
Thus, patients in whom the placental edge is close to the internal cervical os during the first and second trimesters must undergo a follow-up ultrasound, as this location would be classified as placenta previa if it persists after 28 weeks, and ultrasound evaluation and clinical treatment planning should be more stringent. In this regard, Alouini et al.,41 in a retrospective study of 319 patients treated at the Orléans Regional Hospital Center between 1998 and 2004 who presented with placenta previa or low placental implantation, established that most placentas that were less than 1cm from the internal cervical os did not migrate, while most of those above 1cm migrated 3 or 4 weeks later.
In the present study, maternal morbidity prevailed over perinatal morbidity, with a predominance of procedures such as Cesarean section and obstetric hysterectomy, and the use of blood products, which is consistent with the findings by Crane et al.,42 who established in their review that morbidities associated with placenta previa include hysterectomy (RR: 33.26; 95%CI: 18.19-60.89), antepartum hemorrhage (RR: 9.81; 95%CI: 8.92-10.79), intrapartum hemorrhage (RR: 2.48; 95%CI: 1.55-3.98), postpartum hemorrhage (RR: 1.86; 95%CI: 1.46-2.36), and the need for blood transfusions (RR: 10.05; 95%CI: 7.45-13-55).
Regarding perinatal morbidity, it was found that 3 newborns were premature but 2 of them were born before the due date because of maternal reasons (preeclampsia). This is in agreement with Ahumada et al.,43 who reported in their study of 452 pregnant women treated between October 2014 and May 2018 at three antenatal care centers in Bogotá, D.C., that having a diagnosis of preeclampsia (severe and non-severe) was the main risk factor associated with preterm delivery.
Kollmann et al.,2 conducted a study in 10 hospitals in Austria, with a sample of 328 pregnant women, which showed perinatal complications such as prematurity, low birth weight <2 500g, Apgar score at 5 minutes <7, and fetal mortality. This finding of neonatal morbidity was also described by Vahanian et al.44 in their systematic review of 2015, although the present study did not find high perinatal morbidity rates due to complications of placenta previa.
Similarly, it is noteworthy that in the present study no newborn required admission to the NICU, which is consistent with what was described by Téllez-Santos & Wandurraga-Barón,45 who also reported a low rate of perinatal morbidity, but different from the reports by Roustaei et al.,22 whose multivariate logistic regression result showed that babies of women with placenta previa were at increased risk of admission to the NICU and a low Apgar score at 5 minutes.
In the study by Kollmann et al.,2 the evaluated population was stratified into two groups: patients with total or partial placenta previa and patients with marginal placenta or low-implantation placenta. It was concluded that patients diagnosed with marginal placenta or low-implantation placenta should not be underestimated, as this type of placenta does not affect the severity of bleeding or complications, which is consistent with what was found in the present study, where the patient who required subtotal hysterectomy and blood product transfusion had a diagnosis of marginal placenta.
The limitations of the present study were its small sample size, its retrospective nature, and the possible bias during the collection of the data since they were obtained from the medical records. As a consequence, the results obtained here cannot be extrapolated to the Colombian population in general. However, this study provides the basis for future research on the subject.
Conclusions
Since it has been established that there are multiple risk factors for placenta previa, it is worthwhile to know the most common risk factors in specific populations. In the present study, the most prevalent risk factors were >4 pregnancies, maternal age of >35 years, and a history of miscarriage.
Furthermore, it was demonstrated that maternal morbidity prevailed over fetal morbidity and that the degree of maternal-perinatal complications was independent of the type of placenta previa. Knowing which population is most at risk of developing this condition through early identification of risk factors allows for a better diagnosis, clinical approach and follow-up, as well as the design of strategies for both preconceptional and antenatal care with the aim to significantly reduce morbidity and mortality and complications of the mother-child binomial.















