Introduction
Tuberculosis (TB) can be diagnosed by finding Mycobacterium tuberculosis bacteria, either through smear microscopy, culture, or molecular methods.1-3 Extra-pulmonary tuberculosis (EPTB) diagnosis poses a challenge for physicians, provided that conventional techniques have limitations, its clinical presentation is variable, and samples used in pathology tests are generally paucibacillary.4,5 Different markers have been proposed as diagnostic tools for pulmonary TB and EPTB, including markers of cellular activity, acute-phase reactants, and enzymes.6-8 Cancer antigen 125 (CA-125) has been proposed as a useful biomarker for the diagnosis of TB, but its utility has not yet been validated.9
CA-125 is generally used as a diagnosis and monitoring marker of ovarian carcinoma; however, high concentrations of this glycoprotein have been described in other malignancies such as liver, colorectal, gastric, and pancreatic neoplasms.10 High CA-125 levels have also been described in benign diseases including heart failure, lung disease, liver cirrhosis and intra-abdominal conditions.11 CA-125 was also proposed as a useful marker to evaluate TB pleural effusions treatment response.12 Likewise, some authors have described the use of this biomarker in the diagnosis and treatment response evaluation in both pulmonary tuberculosis (PTB) and EPTB.13-19
In Colombia, a country where TB incidence and mortality rates are high, there is little information on the use of CA-125 test in TB diagnosis, and the limited data on this subject come from case reports in which patients with peritoneal TB had elevated levels of this biomarker that were similar to those reported for ovarian cancer .20,21 Therefore, further research is necessary to determine if CA-125 levels may be considered relevant in terms of PTB and EPTB diagnosis and in relation to the outcomes obtained in patients who were treated appropriately, particularly in Latin America where this relationship has been poorly studied.20,22 Taking this into account, the purpose of this study was to describe serum CA-125 levels behavior in patients with TB treated in a referral university hospital located in Cali, Colombia.
Materials and methods
Study design and patient selection
Cross-sectional study conducted in patients with TB and available serum CA-125 level measurements treated between January 2007 and January 2016 at Fundación Valle del Lili, a university hospital in Cali, Colombia, that works as a referral health center for the southwestern region of the country.
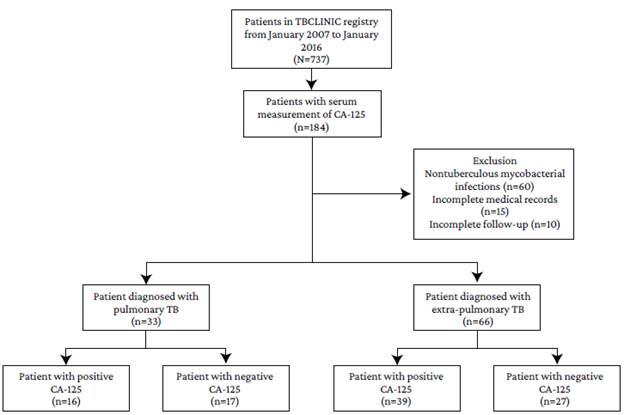
The TB Registry database (TBCLINIC) of the hospital and the medical records of TB patients were reviewed. The database included sociodemographic, clinical and laboratory information of these patients, as well as their treatment outcomes. Patients with TB and a serum CA-125 level measurement at the time of diagnosis and before treatment was initiated were included. All patients with nontuberculous mycobacterial infections, incomplete medical records, incomplete follow-up information, or conditions that have been associated with increased CA-125 levels were excluded. Taking this into account, 99 patients were included in the study. Figure 1 depicts the patient selection process.
Definitions
TB case were defined based on the definitions established by the World Health Organization23 and the technical and operational guidelines of the National TB Program implemented by the Colombian Ministry of Health.24
This study includes microbiologically confirmed and clinically diagnosed cases of TB. A TB case was considered microbiologically confirmed if M. tuberculosis was detected using a culture test or molecular biology-based techniques. Patients with a positive sputum-smear microscopy result alone were not considered as clinically diagnosed TB cases. Pleura TB cases were established using the adenosine deaminase (ADA) test with a cut-off point of 40 U/L, since it is the best test for detecting this type of TB in high prevalence areas and this cut-off point is widely accepted.25,26
Pulmonary TB (PTB) refers to any case of TB affecting the lung parenchyma, or tracheobronchial tree, whereas extrapulmonary TB (EPTB) to infections outside the tracheobronchial tree.23
Once patients were discharged from the hospital, follow-up was made through telephone calls until the prescribed TB treatment for each patient was completed.
Measurement of serum CA-125 levels
Serum CA-125 levels were measured using a commercial radioimmunoassay kit (Roche Elecsys® CA-125 II assay). According to the manufacturer's instructions, the standard range was set at <35 U/mL (95th percentile). The test was conducted at the discretion of the infectious disease specialist.
Statistical analysis
Descriptive statistics were used for data analysis. Quantitative variables are presented using central tendency and dispersion measures according to the distribution of data, which was determined using the Shapiro - Wilk test, and categorical variables, using frequency distributions and percentages. A bivariate analysis was performed to compare the variables of interest (sociodemographic, clinical [comorbidities, risk factors and diagnosis criteria], and laboratory findings data [CA-125 measurements and culture results] and outcomes [mortality]) between groups (PTB vs. EPTB, positive vs. negative CA-125 measurement, and alive vs. dead) using the Mann-Whitney U Test or the unpaired t test, and the Chi-squared test or the Fisher's exact test for continuous and categorical variables, respectively. A significance level of p<0.05 was considered.
Stata® software (StataCorp, 2011, Stata 12 Base Reference Manual, CollegeStation, TX: StataPress) was used to perform all statistical analyses.
Ethical considerations
The study protocol was approved by the Biomedical Research Ethics Committee of Fundación Valle del Lili (Protocol 566, Minutes 12-2018, of June 18, 2018), and followed the ethical principles for medical research outlined by the Declaration of Helsinki.27 It also took into account the health research scientific, technical, and administrative standards set forth in Resolution 8430 of 1993 of the Ministry of Health of Colombia.28 As this is a retrospective study, patient informed consent was not required.
Results
Sociodemographic and clinical characteristics are shown in Table 1. The median age of the study population was 47 years (IQR=29-61 years), there were no significant differences regarding sex, mestizo was the most frequent ethnicity (56.57%), and most of the subjects lived in urban areas (81.82%).
In relation to the type of TB, EPTB was the most frequent as it was diagnosed in 66 subjects, with 57.58% of these cases occurring in patients aged 16 to 45 years; on the other hand, 66.67% of PTB cases (n=33) occurred in individuals aged 45 and up.
The most common comorbidity among the sample was TB/HIV co-infection (22.22%), and other risk factors included the fact that most patients were smokers (16.16%) and had a history of TB contact in the household (13.13%).
Concerning comorbidities and other risks factors for PTB, chronic obstructive pulmonary disease (COPD) and smoking were the most prevalent with 24.24% and 30.30%, respectively, whereas for EPTB they were HIV infection (27.27%), TB contact in the household (12.12%), and history of solid organ transplantation (12.12%). There were significant differences in COPD (p=0.006) and smoking (p=0.009), both of which were more common in PTB patients.
Table 1 Comparison of sociodemographic and clinical characteristics of patients by type of TB.
| Variables | General (n=99) | Pulmonary TB (n=33) | Extra-pulmonary TB (n=66) | p- value | |
|---|---|---|---|---|---|
| Age, mean ± SD | 46.12±18.35 | 52.84±19.14 | 42.75±17.10 | 0.009 | |
| 16-45 years, n(%) | 49 (49.49) | 11 (33.33) | 38 (57.57) | 0.023 | |
| >45 years, n(%) | 50 (50.51) | 22 (66.67) | 28 (42.43) | ||
| Sex, n(%) | Female | 49 (49.49) | 17 (51.52) | 32 (48.48) | 1.129 |
| Male | 50 (50.51) | 16 (48.48) | 34 (51.52) | ||
| Race/Ethnicity, n(%) | Mestizo | 56 (56.57) | 22 (66.67) | 34 (51.52) | 0.566 |
| Caucasian | 14 (14.14) | 5 (15.15) | 9 (13.64) | ||
| African-Colombian | 12 (12.12) | 2 (6.06) | 10 (15.15) | ||
| No data | 12 (12.12) | 3 (9.09) | 9 (13.64) | ||
| Other | 4 (4.04) | 1 (3.03) | 3 (4.54) | ||
| Indigenous | 1 (1.01) | 0 (0) | 1 (1.51) | ||
| Origin, n(%) | Rural | 18 (18.18) | 5 (15.15) | 13 (19.70) | 0.580 |
| Urban | 81 (81.82) | 28 (84.85) | 53 (80.30) | ||
| Comorbidities, n(%) | HIV | 22 (22.22) | 4 (12.12) | 18 (27.27) | 0.075 |
| Diabetes mellitus | 17 (17.17) | 5 (15.15) | 12 (18.18) | 0.683 | |
| COPD | 11 (11.11) | 8 (24.24) | 3 (4.55) | 0.006 | |
| Malignancy | 11 (11.11) | 5 (15.15) | 6 (9.09) | 0.499 | |
| Hepatitis C virus | 1 (1.01) | 0 (0) | 1 (1.52) | 1.000 | |
| Pregnancy | 1 (1.01) | 0 (0) | 1 (1.52) | 1.000 | |
| Other risks factors, n(%) | Smoker | 16 (16.16) | 10 (30.30) | 6 (9.09) | 0.009 |
| TB contact in the household | 13 (13.13) | 5 (15.15) | 8 (12.12) | 0.757 | |
| History of solid organ transplantation | 11 (11.11) | 3 (9.09) | 8 (12.12) | 0.746 | |
| Healthcare worker | 10 (10.10) | 4 (12.12) | 6 (9.09) | 0.725 | |
| Previous TB infection | 9 (9.09) | 5 (15.15) | 4 (6.06) | 0.155 | |
| Dialysis | 7 (7.07) | 3 (9.09) | 4 (6.06) | 0.683 | |
| Drug dependence | 6 (6.06) | 2 (6.06) | 4 (6.06) | 1.000 | |
| History of bariatric surgery | 2 (2.02) | 1 (3.03) | 1 (1.52) | 1.000 | |
| Former inmate | 2 (2.02) | 2 (6.06) | 0 (0) | 0.116 | |
| CA-125 (U/mL), median (IQR) | 43.59 (21.19-122.40) | 34.48 (22.10-77) | 48.74 (21.19-129.40) | 0.369 | |
| Negative (≤35), n(%) | 44 (44.44) | 17 (51.52) | 27 (40.91) | 0.317 | |
| Positive (>35), n(%) | 55 (55.56) | 16 (48.48) | 39 (59.09) | ||
| Culture, n(%) | Negative | 46 (46.46) | 16 (48.48) | 30 (45.45) | 0.776 |
| Positive | 53 (53.54) | 17 (51.52) | 36 (54.55) | ||
| Diagnosis criteria, n(%) | Microbiological | 78 (78.79) | 28 (84.85) | 50 (75.76) | 0.297 |
| Clinical | 21 (21.21) | 5 (15.15) | 16 (24.24) | ||
HIV: human immunodeficiency virus; TB: tuberculosis; COPD: chronic obstructive pulmonary disease; CA-125: cancer antigen 125.
Source: Own elaboration.
The median serum CA-125 level was 43.59 U/mL (lQR=21.19-122.40 U/mL). Positive results (>35 U/mL) were reported in 55 subjects (55.56%), and there was a higher proportion of positive serum CA-125 results in EPTB patients (59.09%) than in those diagnosed with PTB (48.48%). Taking this into account, serum CA-125 results were analyzed individually for each type of EPTB: in the case of tuberculous pericarditis, the 2 patients diagnosed with this form of EPTB had a positive CA-125 test result, while in the tuberculous peritonitis (n=19) and tuberculous pleuritis (n=12) cases, positive CA-125 measurements were observed in 68.42% and 66.66% of the patients, respectively. Moreover, 66.66% of patients with miliary TB and spinal TB, respectively, showed elevated CA-125 results (>35 U/mL) (Figure 2).
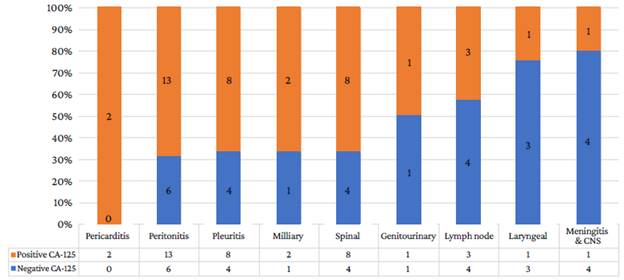
Source: Own elaboration.
CA-125: cancer antigen 125; CNS: central nervous system.
Figure 2 CA-125 results for each form of EPTB (n=66).
The majority of cases were microbiologically diagnosed (78.8%). After hospital discharge, complete follow-up during the treatment period was only possible in 66 patients, of whom 51 survived and 15 had a fatal TB-infection related outcome. A statistically significant difference was found in the analysis of CA-125 levels in relation to the clinical outcome reported for the study population (p=0.021); 13 (87%) of the 15 deaths had a positive CA-125 measurement before treatment initiation, while an elevated CA-125 level was observed in 24 (47%) cases of the surviving patients group. Of the mortality cases, 6 had PTB, 4 had EPTB (2 peritoneal, 1 pleural, 1 spinal), and 5 had miliary TB.
Discussion
This study describes an eight-year experience with PTB and EPTB diagnosis and follow-up, as well as CA-125 levels measurement, in a university hospital in Cali, Colombia.
CA-125 is found in derivatives of coelomic epithelia, mainly in serous membranes.29,30 This could explain why in the present study increased CA-125 levels were observed in patients with pleural, pericardial, peritoneal and miliary TB, as said elevations could be caused by an inflammatory response triggered by the involvement of these membranes due to TB infection.13,31 However, the small number of cases with serous membrane involvement included in this study does not allow concluding that this association exists; for this reason, further studies are required to address this relationship.
In the present study, high concentrations of CA-125 (>35 U/mL) were observed in 55.56% of the patients, regardless of the type of TB or whether the diagnosis was confirmed or only suspected. After stratifying the results by TB type, a higher frequency of elevated CA-125 levels (positive results) was found in patients with EPTB (59.09%) compared to PTB patients (48.48%), particularly in those with serous-membrane involvement (69.69%: [100%, 68.42%, and 66.66% for tuberculous pericarditis, peritonitis and pleuritic, respectively]).
The above results partially differ from the findings reported by Huang et al.13 in an observational case series study conducted in Taiwan between January 2000 and January 2007 involving 64 patients with PTB and EPTB. In that study, 100% of the patients with EPTB had elevated CA-125 levels, which is significantly higher than our results; however, in their PTB group, 45% had a positive CA-125 result, which is very similar to our findings. Likewise, Nakanishi et al.,32 in a study that measured CA-125 levels in TB and non-TB pleural effusion samples, documented elevated levels of this biomarker in all of the patients in the TB group (mean: 167.3±96.8 U/mL, n=8),13,32 being significantly higher than those in non-TB patients (mean: 36.9±18.4 U/mL; p<0.01).
As described above, elevated CA-125 levels were more frequent in serous-membrane involvement TB cases (69.69%). It should be noted that serous membrane involvement was confirmed through a pathology study in almost all cases and that diagnosis was established after peritoneal or pleural fluid PCR was performed only in 2 cases of tuberculous peritonitis and 1 case of tuberculous pleuritis. In addition, 68.42% of tuberculous peritonitis had a CA-125 positive result, which is consistent with what has been described in other studies.
For example, in a study conducted in 10 patients with tuberculous peritonitis by Mas et al.,15 the mean serum CA-125 level was 475.8 U/mL, which is significantly higher than the positive cut-off value (>35 U/mL) of the present study and demonstrates that patients with tuberculous peritonitis usually present with increased CA-125 values. As previously stated, the first descriptions of the connection between tuberculosis and increased CA-125 levels were associated with tuberculous peritonitis cases.33-35 Likewise, in the present study, CA-125 levels above the established cut-off point were observed in 8 patients with tuberculous pleuritis (66.66%) and in 8 with miliary TB (66.66%), which is consistent with the existing literature, where it has been described that patients with these forms of TB may have increased levels of CA-125.13,32,36
It is noteworthy that, in the present study, a positive CA-125 result was observed in the 2 tuberculous pericarditis cases, but since only these 2 cases were included, it is not possible to draw any valid conclusions given the small size of this population, even though, in general, this type of TB is rare, accounting for approximately 1% of TB cases worldwide.37 Finally, to the best of the author's knowledge, there are no studies addressing the correlation between CA-125 levels and tuberculous pericarditis, probably because its occurrence is rare.
As for mortality, a statistically significant difference was found when comparing patients with positive and negative CA-125 measurements made before treatment initiation (p=0.021), regardless the type of TB. Increased CA-125 levels have been correlated with higher mortality in patients with chronic obstructive pulmonary disease, pulmonary hypertension, and even in postmenopausal women.38-40 To the best of the author's knowledge, no studies have proposed CA-125 as a prognostic factor in terms of mortality for patients with PTB and EPTB. It is important to note, however, that nearly half (47%) of the surviving participants in the present study also had elevated CA-125 levels prior to treatment initiation.
Some studies have assessed the usefulness of this biomarker in TB treatment response. For instance, Huang et al.13 concluded that CA-125 testing, together with clinical response assessment, might be useful to monitor TB treatment. Another study suggested an association between TB infection and increased CA-125 levels in the context of the activity and severity of the disease, concluding that measuring CA-125 levels may be useful for monitoring treatment response in some PTB cases.19 Nevertheless, the role of serum CA-125 levels measurement in relation to mortality as an outcome of TB has not been analyzed to date.
It should be noted that 66 of the subjects included in this study (n=99) had extra-pulmonary involvement, which is considered a condition that makes TB diagnosis more challenging.4,5 EPTB was more frequent in patients <45 years old, with diabetes mellitus or HIV infection as comorbidities. This relationship has already been proposed in the case of HIV infection,41 but diabetes as a risk factor for EPTB has not been supported in the scientific literature.42
With respect to tuberculous pleuritis, the best data available suggest that a positive result of the ADA test in high-prevalence areas would be sufficient to make the diagnosis.25 In this regard, a meta-analysis that included 174 studies with 27 009 patients estimated a sensitivity of 0.92 (95%CI: 0.90-0.93) and a specificity of 0.90 (95%CI: 0.88-0.91) for this test, but all studies showed a high risk of bias.43 In turn, the Xpert MTB/RIF Ultra test has been found to have a better sensitivity (63.25%) compared to blood culture, Xpert MTV/RIP, or smear, as well as a reasonable specificity (98.81%).44 In future works, CA-125 performance could be evaluated together with ADA and the Xpert MTB/RF tests results in these patients .
Considering the results obtained here, it is not possible to propose CA-125 testing as a useful tool to make a differential diagnosis between PTB and EPTB; however, CA-125 measurement could be beneficial in the workup approach to cases in which TB of serous membranes or disseminated TB are suspected.
As for TB prognosis, CA-125 testing prior to initiating therapy may be effective in predicting the risk of mortality associated with TB infection. However, further research is necessary to assess the relevance of this biomarker as a predictor of TB-related adverse outcomes.
It should be noted that this was an observational study and that assessing the utility of CA-125 level measurement in terms of TB related mortality was not its sole objective; consequently, several significant limitations emerged. First, no sample size calculation was performed because all cases were obtained directly from the "TB registry. Second, only one CA-125 measurement test was performed prior to treatment initiation in all cases; however, multiple measurements must be made during and after treatment for a better analysis of the prognostic usefulness of this biomarker. Third, complete follow-up was not possible in all cases, mainly due to health system-related and geographic constraints, so the authors are unaware of the outcomes in these patients. Fourth, because the bio-marker was measured at the discretion of the infectious disease specialist, the study may have a selection bias. Finally, since only patients with a suspected or confirmed diagnosis of tuberculosis were included in the study, CA-125 measurements in the study population were not compared with a control group.
Conclusions
In this study, a greater proportion of CA-125 levels positive cases was found in patients with EPTB, especially in tuberculous serositis, miliary TB, and spinal TB. Although the CA-125 test is not routinely performed on these patients, the results reported here may be useful for further research on the usefulness of CA-125 measurement for prognostic purposes.